2010Rh阴性输血策略(尼日利亚Du)
Rh阴性患者输血策略
Rh阴性患者输血策略兰炯采【期刊名称】《上海医药》【年(卷),期】2015(36)12【摘要】近年来,有关Rh阴性患者的输血问题由于媒体炒作而变得复杂化,不利于临床对患者的生命抢救。
政府已对Rh阴性患者的输血颁布了有关法规,以指导临床安全、有效和科学的输血。
对于体内无抗-D抗体的Rh阴性患者,在血资源紧急情况下可以输配血相合的Rh阳性血,而对于有抗-D抗体者则应尽量输注Rh阴性血。
本文阐述Rh阴性患者安全、有效、科学的输血策略。
%In recent years, the blood transfusion in Rh negative patients has been complicated due to media hype, which hampers the patients’ life in clinical emergency treatment. The government has already issued the relevant laws and regulations for Rh negative blood transfusion in order to guide the safe, effective and scientiifc blood transfusion. When the blood resources are insuifcent in an emergency situation, the Rh negative patients without anti-D antibody can receive Rh D-positive blood, while those with anti-D antibody must infuse Rh D negative blood as possible. This paper states the strategy for safe, scientiifc and reasonable blood transfusion in patients with Rh negative blood.【总页数】3页(P6-7,10)【作者】兰炯采【作者单位】南方医科大学南方医院输血科广州 510105【正文语种】中文【中图分类】R457.1+1【相关文献】1.不同疾病RhD阴性患者成分输血策略探讨 [J], 马曙轩;徐樨巍;宋文琪;薛晖;邵华;刘景汉2.Rh(D)阴性患者紧急抢救输血中应用“配合型输血”的回顾性分析 [J], 梁静;杨丽萍;刘雯;刘景汉;兰炯采3.1例Rh(D)阴性患者输血引发迟发性输血反应原因探讨 [J], 王振芳;袁青柳;王帅;王亚;闫有敏;胡佳丽;刘洋;杨连莲;尹虎;蔡金生4.浅谈输血工作中RH阴性患者的临床输血 [J], 段丽华5.浅谈输血工作中Rh阴性患者的临床输血 [J], 屈英晓;刘再清因版权原因,仅展示原文概要,查看原文内容请购买。
RH阴性血型患者的输血原则

RH阴性血型患者的输血原则1、患者没有抗-D存在时,男性RH阴性患者或无生育能力的RH阴性妇女初次输血可输注RH阳性血,再次输血时则只能输RH阴性血,但有生育能力的妇女及儿童最好输RH 阴性血,否则将来妊娠可能产生新生儿溶血病。
2、患者自身有抗-D存在时,最好输RH阴性血,但紧急情况下也可输RH阳性血。
因为抗-D属IgG型抗体,不会发生急性输血反应,一般要2周后才会发生迟发性输血反应,此时病人已度过危险期,有充足时间寻找RH阴性血源,但要与病人亲属签订协议书,注明风险以及将来只能输RH阴性血或可能产生RH新生儿溶血病。
3、尽管血小板表现无抗-D抗原,但制品中含有一定量的红细胞(可使患者致敏),故RH阴性生育期的女患者(包括女童)应输RH阴性血小板,至于RH阴性男患者和RH阴性无生育能力的女患者只要体内无抗-D,紧急情况下可输RH阳性血小板。
4、RH抗体为IgG型,故在盐水介质中不凝集相应红细胞,配血时应加用抗球蛋白试验,聚凝胺试验等,以避免漏检而发生迟发性溶血性输血反应。
5、RH阴性全血或红细胞在4℃条件下只能保存35天,为避免血液资源浪费,在过期前没有用于RH阴性患者,可输给RH阳性患者(要求ABO同型,交叉配血试验相合)。
6、RH阴性患者需要输注新鲜冰冻血浆时,可按ABO同型输注,RH(D)血型可忽略。
Rh阴性输血原则来源:本站原创编辑:yatao 添加日期:2011年02月20日关键字:RH阴性输血原则导读:Rh阴性输血原则一、基本原则Rh阴性是指Rh(D)抗原表达为阴性。
Rh阴性病人输入Rh阳性血后,大部分患者在两周后会产生抗-D,当再次输注Rh阳性血时会导致严重输血不良反应,因此Rh阴性病人的输血需遵循以下原则详细内容:Rh阴性输血原则一、基本原则Rh阴性是指Rh(D)抗原表达为阴性。
Rh阴性病人输入Rh阳性血后,大部分患者在两周后会产生抗-D,当再次输注Rh阳性血时会导致严重输血不良反应,因此Rh阴性病人的输血需遵循以下原则:1、病情允许,严格遵守ABO同型输血和配合型输血的原则,输注Rh阴性血液。
Rh(D)阴性患者输血管理制度
XX县第一人民医院Rh(D)阴性患者输血管理制度Rh(D)阴性患者需要输血时,由于血源极度稀少,往往难于满足临床需要,在紧急情况下由于不能提供足够血源可能危及患者生命,导致医疗纠纷或不稳定事件,加强对Rh(D)阴性患者输血的管理,避免医疗安全事件发生,特制定以下规定。
第一条择期手术或平诊Rh(D)阴性患者需要输血时,经治医师要充分预定用血量,并要求至少提前3天向输血科送交输血申请单,输血科接到输血申请单后向市中心血站申报预约计划,尽可能输注Rh(D)阴性血。
为保障患者安全,在未准备好手术所需足够血源前,择期手术应暂缓实施。
第二条Rh(D)阴性患者必须实施紧急输血时,医院输血科与市中心血站又不能调配到Rh(D)阴性血液时,启动应急用血预案。
立即向分管院长和医务科报告,组织医院临床输血管理委员会专家进行紧急会诊,并按照本制度相关规定和《紧急用血管理制度》确定紧急输血方案。
确立的紧急输血方案需要输血管理委员会成员3人、临床用血科室主任、主管医师、患者家属(或监护人)共同签字确认并签署同意书后方可实施。
无受血者家属(或监护人)签字的紧急输血,严格按《紧急用血管理制度》中第9条规定办理。
第三条患者为Rh(D)阴性,没有检测到抗-D,如需紧急输血又无同型血时,男性患者及无生育能力或无再次生育要求的妇女可输Rh(D)阳性血,但应向患者和家属(或监护人)说明并签署知情同意书后方可实施。
第四条有生育能力的Rh(D)阴性妇女(包括女童),应当输注Rh(D)阴性血,在无Rh(D)阴性血源时,如不立即输血可危及患者生命,应本着抢救生命第一的原则,先输Rh(D)阳性血挽救患者生命,但应向患者家属(或监护人)说明可能产生的后果,并签署知情同意书后方可实施。
第五条Rh(D)阴性生育期的女性患者(包括女童)在输注血小板时,尽管血小板表面无D抗原,但血小板制品中含有一定量的红细胞也可使患者致敏,故Rh(D)阴性生育期的女性患者(包括女童)应输Rh(D)阴性血小板。
RH阴性患者输血管理制度

RH阴性患者输血管理制度第一篇:RH阴性患者输血管理制度标准化操作规程RH(D)阴性患者输血管理制度SOPSX015.04 景德镇市1、择期手术或平诊RH(D)阴性患者需要输血时,要求提前3天,申请单向血站预约,尽可能输注RH(D)阳性血。
2、患者的RH(D)阴性,没有检测到抗-D,如需紧急输血又无同型血时,男性患者及无生育能力的如可输RH(D)阳性血,但应向患者家属说明并征得同意。
3、患者RH(D)阴性,体内虽未检测抗-D,但患者是有生育能力的妇女(包括女童),最好输注RH(D)阴性血。
4、患者的RH(D)阴性,又是有生育能力的妇女,但一时代不到RH(D)阴性血,不立即输血会危及患者的生命,此时应本着抢救生命第二篇:发现Rh阴性血型处理流程输血科Rh(D)阴性血型的处理流程1.输血科工作人员进行血型检验发现患者为Rh(D)阴性时,应首先进行血型复查(必须重新采血样),确认为Rh(D)阴性时,应及时上报科主任。
2.科主任了解相关情况后根据病情作必要的安排,需要联系血站,安排人员将病人标本送往市中心血站进行确证试验。
3.临床科室如需要Rh(D)阴性血液制品时,参照《中心医院紧急特殊用血(稀有血型)预案》执行。
4.妇产科的产妇为Rh(D)阴性时,需要提前安排检查其配偶的血型,为可能发生的新生儿溶血病作准备。
**医院输血科第三篇:RH阴性孕妇注射抗D免疫球蛋白申请尊敬的医疗科、护理部:随着我院产科分娩量的增加,RH阴性孕妇也随之增加。
由于RH 阴性孕妇在孕期及产褥期可能因胎儿RH阳性而发生致敏,导致再次妊娠时可能发生胎儿溶血,导致胎儿贫血、严重者需换血,甚至威胁胎儿生命。
根据目前的诊治规范,需要给RH阴性孕妇分别在孕28周、孕37周以及分娩后72小时内注射抗D免疫球蛋白以阻断抗D抗体的产生。
但目前国内医药市场缺乏抗D免疫球蛋白制剂,该药通常由患者在香港或国外医药市场自行购买,再到医院完成注射。
目前,有部分医院在与患者签署知情同意书的情况下予以注射,但我院目前没有相关规定。
Rh阴性患者输血存在的问题及应对之策

Rh阴性患者输血存在的问题及应对之策Rh阴性患者输血问题相对较复杂,存在极多的特殊情况,往往涉及了伦理、医学、社会、法律法规等各方面。
因临床Rh阴性的供应十分紧张,有一些医务人员存在对Rh阴性输血知识问题的欠缺以及大众媒体、影视剧等相关传播对于Rh阴性患者未进行科室严谨的宣传,为此,社会大众则认为Rh阴性输血应当输入Rh阴性血液,即红细胞,有些Rh阴性患者由于输血未得到及时抢救而造成死亡,致使医疗纠纷问题的产生。
下面我们则针对Rh阴性患者输血存在的问题进行分析,并探讨应对措施。
一.Rh血型介绍Rh血型系统包含D抗原、C抗原、c抗原、E抗原与e抗原,在临床上,所有带D抗原的均称之为Rh阳性,对于不带D抗原的则称为Rh阴性。
在我国,仅汉族群体中所占据的Rh阴性例约4‰。
Rh在临床输血时,若机体内有针对D抗原的抗体,输入Rh阳性血液则会出现溶血性输血反应,其临床症状为头痛、寒战、腰背酸痛、高热、尿呈酱油色,对于情况严重的还堆叠造成休克、血压降低、肾功能衰竭等情况,更有甚者则有生命危险。
Rh阴性患者体内中若不具备抗-D,在为其输入Rh阳性血液后如果未发生溶血性输血反应,但并不代表不会被免疫产生抗-D,若在此之后再次输血则只能输入Rh阴性血,女性患者在怀孕时有可能产生新生儿溶血病。
二. Rh阴性患者输血存在的问题在临床中,无论患者机体内是否存在抗D抗体、是否为育龄少女、无论患者性别如何、无论患者需要输注哪一类血液成分,一些医务工作人员、患者个人以及家属等一律等到有Rh相关血液成分后才能输注。
此类问题是相当严重的,比如据临床报道有一例Rh阴性产妇出现大出血,从基层医院转送至上级大医院后也未能及时为患者输注血液,并造成患者死亡,死者家属状告血液中心以及相关医院引起医患纠纷案。
输血科或血液中心在有效期内Rh阴性血液成分分配发给Rh阴性患者时,有些医务人员或患者不接受输注,从而会造成血液的浪费。
Rh阴性血液成分红细胞上无D抗原,输送给D阳性患者不会产生抗D抗体,极为安全。
新RH阴性血型患者的输血原则

RH阴性血型患者的输血原则
(1)患者没有抗-D存在时,男性RH阴性患者或无生育能力的RH阴性妇女初次输血可输注RH阳性血,再次输血时则只能输RH 阴性血,但有生育能力的妇女及儿童最好输RH阴性血,否则将来妊娠可能产生新生儿溶血病。
(2)患者自身有抗-D存在时,最好输RH阴性血,但紧急情况下也可输RH阳性血。
因为抗-D属IgG型抗体,不会发生急性输血反应,一般要2周后才会发生迟发性输血反应,此时病人已度过危险期,有充足时间寻找RH阴性血源,但要与病人亲属签订协议书,注明风险以及将来只能输RH阴性血或可能产生RH新生儿溶血病。
(3)尽管血小板表现无抗-D抗原,但制品中含有一定量的红细胞(可使患者致敏),故RH阴性生育期的女患者(包括女童)应输RH阴性血小板,至于RH阴性男患者和RH阴性无生育能力的女患者只要体内无抗-D,紧急情况下可输RH阳性血小板。
(4)RH抗体为IgG型,故在盐水介质中不凝集相应红细胞,配血时应加用抗球蛋白试验,聚凝胺试验等,以避免漏检而发生迟发性溶血性输血反应。
(5)RH阴性全血或红细胞在4℃条件下只能保存35天,为避
免血液资源浪费,在过期前没有用于RH阴性患者,可输给RH阳性患者(要求ABO同型,交叉配血试验相合)。
(6)RH阴性患者需要输注新鲜冰冻血浆时,可按ABO同型输注,RH(D)血型可忽略。
RhRh(D)阴性患者输血管理制度
Rh(D)阴性患者输血管理制度由于在我国汉族人中Rh(D)阴性者约占3 %,加之输血时要求ABO同型,交叉配血试验完全相合,所以Rh(D)阴性血源难免紧张,为了满足临床用血,特制定本制度。
1、择期手术或者平诊Rh(D)阴性患者输血时,要求临床科室至少要提前3天提出申请,由输血科向血站预约,尽可能输Rh(D)阴性血。
2、患者为Rh(D)阴性且含有抗-D,必须输注Rh(D)阴性血。
3、择期手术的Rh(D)阴性患者要尽可能开展自身输血或动员患者亲属互助献血,具体按《临床输血技术规范》第7、8条执行。
4、患者为Rh(D)阴性,没有监测到抗- D,如需要紧急输血又无同型血,男性患者及无生育能力的妇女可输Rh(D)阳性血,但必须征得患者家属或监护人的签名同意,并在《输血治疗同意书》上注明。
以后需要输血时有可能只能输注Rh(D)阴性血。
5、患者为Rh(D)阴性,体内虽未监测到抗- D,但患者是有生育能力的妇女(包括女童),最好输注Rh(D)阴性血。
如一时找不到Rh(D)阴性血,不立即输血会危及生命的,应本着抢救生命第一的原则,征得患者家属或监护人同意后先输注Rh(D)阳性血抢救,同时要向家属说明如果将来生育有可能发生新生儿溶血病,尽管输注Rh(D)阳性血后72小时内注射足够剂量的抗- D免疫球蛋白可预防Rh同种免疫,但此药在我国市场上难以买到。
6、尽管血小板上无D抗原,但血小板制品中含有一定量的红细胞(可使患者致敏)。
故Rh(D)阴性生育期的妇女患者(包括女童)应输Rh(D)阴性血小板,紧急情况下要输注Rh(D)阳性血小板须征得患者家属或监护人签名同意。
至于Rh(D)阴性男性患者和Rh(D)阴性无生育能力的女患者只要体内无抗- D,可输Rh(D)阳性血小板。
7、Rh(D)阴性患者需要输注新鲜冰冻血浆时,可按ABO同型或相容输注,Rh(D)血型可忽略。
8、Rh(D)阴性全血或红细胞在4℃条件下只能保存35天,在过期前没有用于Rh(D)阴性患者,为避免血液资源浪费,可输给Rh(D)阳性患者(要求ABO同型,交叉配血相合)。
Rh阴性血型患者的输血问题
Rh阴性患者输血的案例
张某,女34岁,1个孩子母亲,因车祸脾破裂就 诊,需手术备血2000毫升,ARh阴性,血清 未检出Rh抗体, 处理:因患者家属拒输ARh阳性血液,手术迟迟 不能进行延误了救治时机,患者失血性休克状 态持续24小时后开始手术,术中输ARh阴性 冰冻红细胞2800毫升、输Rh阴性血浆1200 毫升, 效果:于术后第二天身亡 不合法、不合情
Rh(-)患者的科学输血原则
建议政府有关部门或医院制定《 Rh(-)患 者紧急抢救输血预案/规程》
明确采取”配合性输血”的临床指征、原 则、操作审批程序、注意事项、纳入规 范化管理 既不耽误Rh(-)重危患者的抢救,医生、 血库又有章可循,无后顾之忧
4.19.5.3医院有应急用血预 案,并能得到落实。
解决Rh(-)患者临床输血问题
1.建立现代化管理、资源共享、能满足临 床需要的Rh-供者库的稀有血型库 2.研究建立快速、有效、适合临床紧急用 血的Rh-血保存技术 3.普及Rh-患者的科学输血知识 (什么情 况必须输R原的免疫性 D>E>C>c 先产生IgM,再产生IgG 抗体量及免疫次数有关:小量不反应 大 量反应;一次不反应 多次反应 永远不反应:机体的免疫状,1/3Rh阴性 者不反应者 抗D以外的抗体检出率逐渐增高
Rh阴性患者输血的案例
病例2 情况:患女换血治愈后2周,因产后胎盘 剥离不全再次住院,要求清宫治疗备血 400毫升 ,0Rh阴性,血清抗D抗体效价 为1:1024 ,血站仍无0Rh阴性血 处理:查看患者一般情况好,血色素13g,无心 脑肾及 血液系统疾病,经家属同意,为该患者行储存式 自体输血,术前自采血400毫升,放入血库冰箱 出血再还输病人。 效果 :手术成功进行。
RH阴性血型患者的输血原则及注意事项

RH阴性血型患者的输血原则及注意事项字体:小中大发布: 07-02 11:35 作者:学术发表网来源:中国知网查看:150次【关键词】RH阴性血型输血原则注意事项1 RH血型人类红细胞血型有多达二十多种的血型系统组成,ABO和RH血型是与人类输血关系最为密切的两个血型系统,当一个人的红细胞存在一种D血型物质(抗原)时,称为RH阳性,用RH(+)表示,当缺乏D抗原即为RH阴性,用RH(—)表示。
2 分布RH(-)的分布因种族分布不同而差异很大,在白种人中的比例较高,约15%,黑种人约占4%,中国人群中新疆维吾尔等少数民族RH(—)的分布为5%,蒙古族人接近1%,汉族人所占的比例较少,仅占0.3%,属稀有血型,RH(-)A型、B型、O型、AB型的比例关系是3:3:3:1。
3 检查RH血型的必要性[1]RH血型检查在临床上的重要性,仅次于ABO系统而处于第二位,RH血型不合的输血有可能危及病人的生命。
(1)母子RH血型不合的妊娠有可能产生死胎,早产,新生儿溶血病.(2)RH阴性的人输入RH阳性血液后(特别是多次输血),在其血清中可能出现RH抗体,若以后再输入RH阳性血,即可发生凝集,造成溶血性输血反应。
(3)RH阴性妇女怀孕阳性胎儿时,胎儿的红细胞借机会进入母体.也可刺激母体产生RH抗体,即使第一次输血也可引起溶血性输血反应。
(4)RH阴性个体输1个单位RH(+)红细胞,约80%患者在2~5个月以内产生抗-D.4 输血原则(1)病情允许,严格遵守ABO同型输血和配合型输血的原则输注RH阴性血液.(2)择期手术的RH阴性患者,应尽可能开展自身输血.(3)紧急情况下,可排除输血史,妊娠史,流产史的RH阴性患者首次输血可输RH阳性血。
(4)弱D及部分D患者应视为RH阴性处理。
5 注意事项[2~4](1)患者没有抗-D存在时,男性RH阴性患者或无生育能力的RH阴性妇女初次输血可输注RH阳性血,再次输血时则只能输RH阴性血,但有生育能力的妇女及儿童最好输RH阴性血,否则将来妊娠可能产生新生儿溶血病。
RH阴性血型患者的输血原则

RH阴性血型患者的输血原则1、患者没有抗-D存在时,男性RH阴性患者或无生育能力的RH阴性妇女初次输血可输注RH阳性血,再次输血时则只能输RH阴性血,但有生育能力的妇女及儿童最好输RH 阴性血,否则将来妊娠可能产生新生儿溶血病。
2、患者自身有抗-D存在时,最好输RH阴性血,但紧急情况下也可输RH阳性血。
因为抗-D属IgG型抗体,不会发生急性输血反应,一般要2周后才会发生迟发性输血反应,此时病人已度过危险期,有充足时间寻找RH阴性血源,但要与病人亲属签订协议书,注明风险以及将来只能输RH阴性血或可能产生RH新生儿溶血病。
3、尽管血小板表现无抗-D抗原,但制品中含有一定量的红细胞(可使患者致敏),故RH阴性生育期的女患者(包括女童)应输RH阴性血小板,至于RH阴性男患者和RH阴性无生育能力的女患者只要体内无抗-D,紧急情况下可输RH阳性血小板。
4、RH抗体为IgG型,故在盐水介质中不凝集相应红细胞,配血时应加用抗球蛋白试验,聚凝胺试验等,以避免漏检而发生迟发性溶血性输血反应。
5、RH阴性全血或红细胞在4℃条件下只能保存35天,为避免血液资源浪费,在过期前没有用于RH阴性患者,可输给RH阳性患者(要求ABO同型,交叉配血试验相合)。
6、RH阴性患者需要输注新鲜冰冻血浆时,可按ABO同型输注,RH(D)血型可忽略。
Rh阴性输血原则来源:本站原创编辑:yatao 添加日期:2011年02月20日关键字:RH阴性输血原则导读:Rh阴性输血原则一、基本原则Rh阴性是指Rh(D)抗原表达为阴性。
Rh阴性病人输入Rh阳性血后,大部分患者在两周后会产生抗-D,当再次输注Rh阳性血时会导致严重输血不良反应,因此Rh阴性病人的输血需遵循以下原则详细内容:Rh阴性输血原则一、基本原则Rh阴性是指Rh(D)抗原表达为阴性。
Rh阴性病人输入Rh阳性血后,大部分患者在两周后会产生抗-D,当再次输注Rh阳性血时会导致严重输血不良反应,因此Rh阴性病人的输血需遵循以下原则:1、病情允许,严格遵守ABO同型输血和配合型输血的原则,输注Rh阴性血液。
RH阴性血液输注管理规程

RH阴性血液输注管理规程由于我国汉族人中RhD阴性者约占3‰,加之输血时要求ABO 同型,交叉配血试验完全相合,所以RhD阴性血源难免紧张,为了满足RhD阴性患者急救时的输血,应按临床输血技术规范第十条规定施行配合性输血,以免坐等 RhD阴性血而延误抡救时机。
现将 R hD阴性患者输血应掌握的基本原则作简要介绍,仅供临床临床医师参考。
1择期手术的RhD阴性患者首选自身输血;2择期手术或者平诊RhD阴性患者输血时,要求临床科室至少提前3d提出申请,由输血科(血库)向血站预约。
3患者为RhD阴性且含有抗 -D,必须输注RhD阴性血。
4弱D患者要看作RhD阴性,申请RhD阴性血,供者为弱D,所采出的血液要当RhD阳性血用。
5紧急情况下,患者为RhD阴性,没有检测到抗-D,男性患者或无生育能力的女性患者可输RhD阳性血,但必须征得患者家属的同意,并在《输血治疗知情同意书》上注明。
若有抗体产生,以后输血只能输注RhD阴性血。
6患者为RhD阴性,体内虽未检测到抗-D,但患者是有生育能力的妇(包括未成年女性)应输RhD阴性血液;如一时找不到RhD 阴性血液,不立即输血会危及患者生命,此时应本着抢救生命第一的原则,先输RhD阳性血抢救。
因为生命权优于生育权,没有了生命谈何生育?更谈不上“将来输血”。
抗体一般在2—5个月内产生,最快也要在2周以后。
只要患者渡过危险期就有充裕时间寻找RhD阴性血液。
经治医生要在《输血治疗知情同意书》上注明可能产生抗-D,将来只能输RhD阴性血液或发生新生儿溶血病,征得家属同意后才能实施。
7尽管血小板表面无D抗原,但血小板制品中含有一定量的红细胞(可使患者致敏),故RhD阴性生育期的女患者(包括未成年女性)应输RhD阴性血小板。
紧急情况下要输注RhD阳性血小板须征得患者家属或监护人签名同意。
至于RhD阴性男性患者或RhD 阴性无生育能力的女性患者只要体内无抗-D,可输RhD阳性血小板。
Rh阴性患者输血注意事项
Rh阴性患者输血注意事项
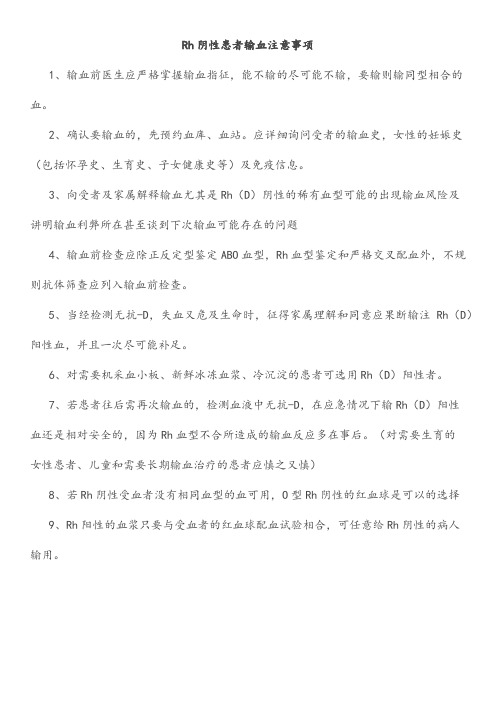
1、输血前医生应严格掌握输血指征,能不输的尽可能不输,要输则输同型相合的血。
2、确认要输血的,先预约血库、血站。
应详细询问受者的输血史,女性的妊娠史(包括怀孕史、生育史、子女健康史等)及免疫信息。
3、向受者及家属解释输血尤其是Rh(D)阴性的稀有血型可能的出现输血风险及
讲明输血利弊所在甚至谈到下次输血可能存在的问题
4、输血前检查应除正反定型鉴定ABO血型,Rh血型鉴定和严格交叉配血外,不规则抗体筛查应列入输血前检查。
5、当经检测无抗-D,失血又危及生命时,征得家属理解和同意应果断输注Rh(D)阳性血,并且一次尽可能补足。
6、对需要机采血小板、新鲜冰冻血浆、冷沉淀的患者可选用Rh(D)阳性者。
7、若患者往后需再次输血的,检测血液中无抗-D,在应急情况下输Rh(D)阳性
血还是相对安全的,因为Rh血型不合所造成的输血反应多在事后。
(对需要生育的
女性患者、儿童和需要长期输血治疗的患者应慎之又慎)
8、若Rh阴性受血者没有相同血型的血可用,O型Rh阴性的红血球是可以的选择
9、Rh阳性的血浆只要与受血者的红血球配血试验相合,可任意给Rh阴性的病人
输用。
RH阴性血型患者的输血原则及注意事项(一)

RH阴性血型患者的输血原则及注意事项(一)作者:张强,石安平,冯利珍,金炜,赛杰勒日呼【关键词】RH阴性血型输血原则注意事项1RH血型人类红细胞血型有多达二十多种的血型系统组成,ABO和RH血型是与人类输血关系最为密切的两个血型系统,当一个人的红细胞存在一种D 血型物质(抗原)时,称为RH阳性,用RH(+)表示,当缺乏D抗原即为RH阴性,用RH(-)表示。
2分布RH(-)的分布因种族分布不同而差异很大,在白种人中的比例较高,约15%,黑种人约占4%,中国人群中新疆维吾尔等少数民族RH(-)的分布为5%,蒙古族人接近1%,汉族人所占的比例较少,仅占0.3%,属稀有血型,RH(-)A型、B型、O型、AB型的比例关系是3:3:3:1。
3检查RH血型的必要性〔1〕RH血型检查在临床上的重要性,仅次于ABO系统而处于第二位,RH 血型不合的输血有可能危及病人的生命。
(1)母子RH血型不合的妊娠有可能产生死胎,早产,新生儿溶血病。
(2)RH阴性的人输入RH阳性血液后(特别是多次输血),在其血清中可能出现RH抗体,若以后再输入RH阳性血,即可发生凝集,造成溶血性输血反应。
(3)RH阴性妇女怀孕阳性胎儿时,胎儿的红细胞借机会进入母体。
也可刺激母体产生RH抗体,即使第一次输血也可引起溶血性输血反应。
(4)RH阴性个体输1个单位RH(+)红细胞,约80%患者在2~5个月以内产生抗-D。
4输血原则(1)病情允许,严格遵守ABO同型输血和配合型输血的原则输注RH 阴性血液。
(2)择期手术的RH阴性患者,应尽可能开展自身输血。
(3)紧急情况下,可排除输血史,妊娠史,流产史的RH阴性患者首次输血可输RH阳性血。
(4)弱D及部分D患者应视为RH阴性处理。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
A Strategic Approach to the Problems of Providing Rhesus D–Negative Blood Transfusion in Geographic Areas With Low RhD Negativity:A Nigerian PerspectiveSagir G.AhmedIn contrast to the white prevalence,the frequency of rhesus D(RhD)negativity in the Nigerian population ranges from less than1%to about6%in the different ethnic population groups across the country.Conse-quently,there is often a severe scarcity of RhD-negative blood in Nigeria,leading to undue delay in transfusing RhD-negative patients.This situation has led to the prolongation of hospital stays as well as increased morbidity and mortality in affected patients.The problem is compounded by the general unavailability of donor RhD-negative blood,which is partially related to a suboptimal national blood transfusion service.This situation has thus relegated the responsibilities of donor recruitment and blood collection to individual hospital blood banks.This has led to the necessity of finding a variety of ways to mitigate the daunting problem of the provision of RhD-negative donor blood in Nigeria.In this article,we review the roles,advantages,and disadvan-tages of various methods including the use of auto-logous donations,D u testing,inter–blood bank transfers,voluntary RhD-negative donor recall,family donations,and cryopreservation to ameliorate the problem.The real need is nonetheless to optimize the functional capacity of the Nigerian National Blood Transfusion Service.©2010Elsevier Inc.All rights reserved.T HE RHESUS(Rh)system consists of5major antigens:D,E,e,C,and c,of which D is the most antigenic.1Unlike the ABO system,naturally occurring antibodies are not usually found in individuals who lack the various Rh antigens.1 Antibodies of the Rh system are all alloimmune in nature with the exception of some naturally occurring anti-E antibodies.1The Rh system was the fourth system to be discovered,yet in terms of clinical importance,it is only second to that of the ABO system because most RhD-negative indivi-duals become alloimmunized after exposure to RhD-positive red blood cells(RBCs),and such antibodies can cause severe hemolytic transfusion reactions and hemolytic disease of the newborn.1In the white populations of Europe and North America,the major clinical problem associated with rhesus system is that of hemolytic disease of the newborn(HDN).2The incidence of HDN is significant in white populations because of the relatively high frequency of RhD-negative indivi-duals that constitute approximately15%of the populace.1In contrast to white figures,the frequency of RhD negativity in the Nigerian population ranges from less than1%to about6% in different ethnic population groups across the country.The highest frequency of RhD negativity is found in the southern part of the country where frequencies of 6.01%and 5.46%have been reported in the south central and southwestern regions,respectively.3,4The frequency of RhD negativity is even lower in the northern regions where frequencies of1.44%and0.6%have been reported in the northeastern and northwestern regions,respectively.5,6One advantage of the low frequency of RhD negativity among Nigerians is the low incidence of HDN in the country.7On the other hand,the low frequency of RhD negativity has resulted in the severe scarcity of RhD-negative RBCs in Nigerian blood banks,a situation that has practically made any request for RhD-negative blood a nightmare for both clinicians and blood bank staff.The problem is compounded by the overall inadequacy of allogeneic donor blood provision in Nigeria,coupled with a suboptimal national blood transfusion service.8This situation has virtually relegated the responsibilities of donor recruitment and blood collections to individual hospital blood banks with the predominance of often unsafe commercial donors.8Clinical experience in Nigeria had shown that RhD-negative blood is not readily available in the blood bank at the time of request in the over-whelming majority of cases.The scarcity of RhD-negative blood in Nigerian blood banks had often resulted in undue delay in transfusing RhD-negative patients,a situation that had led toFrom the Aminu Kano Teaching Hospital,Kano State,Nigeria.Address reprint requests to Sagir G.Ahmed,MBBS,FWACP,Department of Haematology,Aminu Kano Teaching Hospital,PMB3452,Kano,Kano State,Nigeria.E-mail:drsagirahmed@0887-7963/09/$-see front matter©2010Elsevier Inc.All rights reserved.doi:10.1016/j.tmrv.2009.11.005Transfusion Medicine Reviews,Vol24,No2(April),2010:pp140-146 140prolongation of hospital stay as well as increased morbidity and mortality in affected patients.It has therefore become necessary to find ways of mitigating the daunting problem of RhD-negative donor blood scarcity in Nigeria.In this article,a multifaceted strategic approach is reviewed as outlined in Table 1.SCALING DOWN THE SIZE OF THE PROBLEMAutologous Blood DonationsAutologous blood donation and transfusion have not yet been given the level of attention it deserves in Nigerian hospital blood banks,and the autolo-gous blood procedure is largely restricted to the elites in whom the main motivation is the avoidance of transfusion transmissible infections.8A rational approach toward solving the problem of RhD-negative blood scarcity in the hospital setting would be to scale down the number of requests for RhD-negative allogeneic blood through a process of mandatory preoperative blood group testing of all elective surgical patients.All those found to be RhD-negative thus would become eligible for the autologous donation program and would be en-couraged to participate in such an autologous program.For each eligible patient with normal bone marrow function and with the use of iron supplementation,it should be possible to collect 1U of blood at weekly intervals leading to up to 5U collected over a 5-week period.9Autologous transfusions could also be expanded to include pregnant women that are clinically stable andwithout anemia.Previous reports on autologous donations from pregnant women,for reasons including the avoidance of transfusion transmissi-ble infections or anticipated obstetric hemorrhage,have proven to be safe even in the third trimes-ter.10,11Thus,eligible pregnant women who are RhD-negative could be scheduled for autologous donation at a gestational period that is close to term to secure autologous blood that can be used for unexpected bleeding.All RhD-eligible patients could thus be encouraged to participate in an autologous transfusion program by explaining to them the potential difficulties associated with the rarity of their blood group and reassuring them on the safety of the program as well as highlighting the added advantage of total reduced risk of disease transmission or alloimmunization that may be associated with allogeneic transfusions.8,12Furthermore,autologous donation programs would have the additional advantage of boosting the blood bank reserve of RhD-negative blood because unused units that had satisfied standard safety criteria could be used to transfuse other RhD-negative patients,particularly those in life-threat-ening emergency situations.13It must however be emphasized that the role of autologous transfusion in alleviating the problem of RhD-negative trans-fusion is to a large extent dependent on the effective collaboration between the blood bank and the attending surgeons.There is therefore the need for individual hospital transfusion committees to promulgate standard guidelines for the use of autologous transfusion that would synchronize theTable 1.Strategic Approaches to the Problem of the Provision of RhD-Negative Blood in NigeriaApproachObjectives and benefitsAutologous donations Scale down demand for allogeneic RhD-negative blood.Freedom fromimmunological and infectious complications of transfusion.D u testingScale down demand for RhD-negative blood by transfusing D u -positive patients with RhD-positive blood.Conserves RhD blood for genuineRhD-negative patients.Inter –blood bank transfer of Rhd-negative blood Effective utilization of ⁎redundant RhD-negative blood units transferred from neighboring blood banks.Recall of accredited voluntary RhD-negative donorsEmergency blood donations from registered voluntary donors (unrelated to patients)to provide RhD-negative blood whenever such blood is notavailable in the blood bank.Donations from RhD-negative family members Emergency blood donations from RhD-negative family members as asupplement to inadequate unrelated donor blood or as the sole source of blood.Cryopreservation of redundant RhD-negative bloodSalvage and freeze ⁎redundant RhD-negative blood units to createRhD-negative RBC reserves for future use.⁎Redundant:RhD-negative units that were randomly donated by voluntary donors in the absence of need by RhD-negative patients.141RHD NEGATIVE BLOOD IN NIGERIAelective preoperative assessments of patients be-tween the surgical departments and the blood banks with the aim of facilitating a program of autologous transfusions.13However,if an RhD-negative pa-tient is not eligible for autologous transfusion and it becomes clear that RBC transfusion is inevitable, the RBCs of such a patient should be subjected to D u testing.D u Testing of RhD-Negative PatientsThe RhD antigen is carried on nonglycosylated proteins of the RBC membrane.1The normal RhD-positive individual has RBCs that express the D antigen within the range of9900to33000 antigenic sites per cell.1Individuals may have RBCs that express fewer D sites per RBC than normal,and such subjects are referred to as having the D u-positive phenotype.1The D u phenotype is subclassified into high grade,low grade,and very low grade,the latter of which has the lowest expression of the D antigen.1RBCs with the D u phenotype have weak expression of the D antigen and thus may be misclassified as D-negative cells in routine rhesus grouping procedures.1However,the direct antiglobin test is potentially capable of detecting all grades of D u with the exception of the very low-grade types.1In clinical practice,it is usually not necessary to determine whether an RhD-negative patient is of the D u phenotype because no harm results from transfusing Rh-negative blood into such patients even if they are D u-positive.1This approach is particularly suitable for white populations in which the frequency of RhD negativity is up to15%.1,2In contradistinction to the situation in whites,the RhD frequency in Nigerians could be less than1%,resulting in severe scarcity of RhD-negative donor blood.6It is therefore rational to attempt to scale down the number of requests for RhD-negative blood by subjecting RBCs of all RhD-negative patients who might require an RBC transfusion to an indirect antiglobin test to detect those that are D u-positive so that they can be transfused with RhD-positive blood,ultimately reducing the burden of RhD-negative RBC transfusions with its attendant problems of blood procurement.Previous studies in Nigeria had shown that the prevalence of D u phenotype among individuals that were grouped as RhD-negative ranged from only 0.95%in the south central to3.4%in the northwest and up to8%in the southwest.4,14,15It is therefore possible to reduce the burden of RhD-negative blood transfusion in Nigeria by the application of the D u test to a variable extent depending on the prevalence of D u phenotype among regional populations.The identification of D u-positive patients thus has a3-fold clinical advantage in the Nigerian environment where RhD-negative blood is scarce.Firstly,the major advantage is that such patients can be transfused with RhD-positive donor blood without the risk of alloimmunization.1 Secondly,valuable and scarce RhD-negative blood would be conserved for use in patients that are genuinely RhD-negative.This is particularly important because donor blood is always in short supply and inadequate with respect to the clinical requirement of patients in Nigeria.8,16Thirdly, female patients that are identified as D u-positive will not be subjected to unnecessary and costly anti-D immunoglobulin(RhIG)injections if they deliver RhD-positive babies.15This is important in Nigeria where RhIG is imported and thus expensive.The identification of the D u phenotype is particularly useful in patients having high RBC transfusion requirements,such as patients with HIV/AIDS,hemophilia,renal failure,malignancies, aplastic anemia,and other types of bone marrow failure,sickle cell anemia(SCA),and other types of chronic anemia.17,18With a population of more than140million,Nigeria is the most populous black nation that carries a heavy disease burden due to SCA,which affects about2%of the general population.17Therefore,from global perspective, Nigeria has more patients with SCA than any other country in the world.17It is therefore imperative that patients with SCA and other transfusion-dependent patients that are RhD-negative be tested for the D u phenotype so that their high transfusion requirements may be easily met with the use of RhD-positive blood if they are D u-positive.Occa-sionally,multiple anemia-causing diseases may coexist in a particular RhD-negative patient,thus amplifying transfusion requirements.For example, the author had the rare opportunity of participating in the management of1RhD-negative patient with both SCA and hemophilia and another RhD-negative patient with both SCA and chronic renal failure.It is in these types of patients that a positive D u test would be particularly helpful.It must however be appreciated that although the D u test has the potential of easing the RBC transfusion requirements if an RhD-negative patient is found to142SAGIR G.AHMEDbe D u-positive,the test must be carried out with caution under rigorously controlled laboratory and reagent conditions so as to avoid the possibility of false-positive results that may lead to wrongful administration of RhD-positive blood to RhD-negative patients.1,19RhD-negative patients who require transfusion and are neither eligible for autologous transfusion nor D u-positive must eventually be given alloge-neic RhD-negative blood,the sourcing of which may be associated with considerable difficulty.SOURCING ALLOGENEICRhD-NEGATIVE BLOODInter–Blood Bank Transfer of RhD-Negative Blood Most RhD-negative patients that require RBC transfusions would not qualify for autologous transfusion.Moreover,clinical experience had shown that most requests for RhD-negative blood are for emergency cases that need blood urgently, and only a few,0.95%to8%,of such patients would be D u-positive.4,14,15We must therefore find ways of dealing with requests for RhD-negative patients that are neither eligible for autologous transfusions nor D u-positive.However,the hard reality in Nigeria is that RhD-negative blood is usually not available in the blood bank at the time of request.It is only on rare occasions that a unit or two may be found,a quantity that is often grossly inadequate.In such circumstances,it is reasonable to solicit RhD-negative blood from neighboring hospital blood banks.It is therefore important for individual blood bank consultants to create a reliable communication network for emergency situations.Personal experience has shown that units of RhD-negative blood might occasionally and unexpectedly be found in a neighboring blood bank in the absence of any needy RhD-negative patient in that institution.Such units could thus be quickly transferred to be transfused to acutely needy RhD-negative patients.Failure to locate RhD-negative blood within the network of neighboring blood banks should immediately prompt the call of registered RhD-negative donors.Recall of Accredited VoluntaryRhD-Negative DonorsVoluntary blood donors are generally scarce in Nigeria.8Moreover,the voluntary donor base appears to be shrinking as a result of rising donor default generally attributable to the worsening economic hardships and fear of predonation HIV testing within the general population.20Nonethe-less,it is important that every hospital blood bank keep a comprehensive register of its available voluntary donors,particularly those with a clearly identifiable RhD-negative donor type that can be contacted in cases of urgent need.Such donors should be appropriately counseled regarding the significance of their blood type and should be made to understand the need for them to respond positively to urgent calls for blood donation. Voluntary donors in Nigeria usually donate no more than once every6months in accordance with standard recommendation.2Therefore,1foresee-able impediment is that RhD-negative blood donors may decline to respond if called upon to redonate any time less than the traditional interval of6 months after the last blood donation.However,it is safe to donate blood any time after8weeks from the date of last donation without the risk of significant iron depletion,and donors should be counseled accordingly.21Nonetheless,persons who donate more frequently than usual should probably be given iron supplementation to prevent the depletion of their iron stores.2Consistent with its level of underdevelopment, Nigeria is bedeviled by inadequate street and house numbering,erratic communication services,and a poor public transportation network,all of which mitigate easy tracing of registered donors.If the search for registered donors is not fruitful,blood bank officials must be prepared to solicit blood donations from a patient's relatives.Family Members as the Source ofRhD-Negative BloodFamily ties are particularly strong in Nigerians as it is in the rest of Africa.Patients in Nigeria are usually looked after by many family members who keep close contact with the patient during hospital admissions.Thus,family blood donations are commonly requested to supplement the scarce voluntary donor blood base.8Therefore,family members of RhD-negative patients should be contacted with regards the possibility of finding persons who are of the correct blood group that could donate for a particular patient.The blood bank may apply a method of mass blood group testing of a patient's relatives in general,but it should be noted that the chances of getting an RhD-143RHD NEGATIVE BLOOD IN NIGERIAnegative individual is higher in first degree than in distant relatives of the patient who requires the transfusion.The genetics of RhD antigen inheri-tance would suggest that the biological parents of an RhD-negative patient must be genotypically D/d or d/d with several possible combinations of D/d vs d/D,D/d vs d/d or d/d vs d/d.22However,in view of the rarity of the RhD-negative phenotype in Nigerians,the parental genotypic combination for couples is more likely to be D/d vs d/D than D/d vs d/d,whereas the combination d/d vs d/d would be quite unusual.23Thus,in the family of any given RhD-negative patient,the probability of a first-degree sibling being RhD-negative(genotype d/d) would be25%if the parents are both D/d or50%if 1parent is D/d and the other parent is d/d.22Hence, it is always worthwhile to search for donors within family members of any RhD-negative patient.Such a search may even be extended to distant relatives because personal experience had shown that RhD-negative individuals were sometimes found in cousins of RhD-negative patients.It must be appreciated that family donor blood transfusions have certain problems that must be addressed in the interest of the patient.For example, in patients with diseases such as SCA,leukemia, and aplastic anemia for whom bone marrow transplantation is being contemplated,multiple transfusions with the blood from a first-degree relative could lead to alloimmunization against a number of HLA antigens,a situation that would disqualify such a relative as a prospective bone marrow donor for the patient.24Hence,family donor blood should only be used as a last resort in patients scheduled for bone marrow transplant. Conversely,multiple transfusions with family donor blood would be beneficial if the patient has end-stage renal disease and the blood donor is the prospective kidney donor because pretransplant donor-specific transfusions maybe associated with enhanced allograft survival.25Nigeria,like many other sub-Saharan African nations,carries a heavy disease burden due to HIV/AIDS,which is also strongly associated with high transfusion require-ments for affected patients.18Caution must be exercised while transfusing such immunocompro-mised patients because of the risk of donor lymphocyte engraftment and graft-vs-host disease, the risk of which is higher with the use of blood from first-degree relatives.26,27Although the risk can be abolished by pretransfusionγ-irradiation of the donor blood unit,such facilities are not readily available in Nigeria.28One important consideration for patients with SCA is that many of their apparently healthy siblings would also be carriers of the sickle cell gene and their RBCs would contain both hemoglobins A and S.Because the parents of patients with SCA are obligate sickle cell carriers,the probability of a first-degree sibling being a sickle cell carrier(HbAS)is50%,with only a25%probability of having a normal genotype (HbAA).29Hemoglobin S constitutes20%to40% of the total hemoglobin in the RBCs of sickle cell carriers.30Therefore,blood from sickle cell carriers is not recommended for transfusion to patients with SCA.31,32This situation makes family donor selection for patients with SCA particularly restric-tive and difficult.Therefore,care must be taken to ensure that all prospective family donors of patients with SCA are screened by hemoglobin electropho-resis so as to select only those individuals that are free from the sickle cell trait.31,32One major disadvantage of family donation that potentially impacts on safety is the fact such donors may be under covert family pressures and as such may go ahead to donate even if they know they belong to high-risk groups for HIV infection.8This could potentially jeopardize blood safety in a country where blood testing in hospital blood banks is usually done using rapid test kits,which vary in quality.33The virtual absence of viral nucleic acid tests for window period detection in Nigerian blood banks makes any donations from high-risk donors particularly dangerous.33It is obvious that RhD-negative blood transfusion in Nigeria is a major challenge for the blood bank staff,registered donors,and patients and their relatives.Nonetheless,there is the need to consider RhD-negative as a rare blood group in Nigeria and to strategically aim at raising RBC stock levels through the process of cryopreservation.CRYOPRESERVATION OFRhD-NEGATIVE BLOODThe frequency of RhD negativity among Niger-ian blood donors ranges from less than1%to about 6%.3-6Therefore,a similar proportion of voluntary donor blood that is donated in Nigeria would be RhD-negative.However,it must be appreciated that such RhD-negative blood donations come random-ly,sporadically,and in single units that are usually interspersed by several weeks.Blood banking144SAGIR G.AHMEDexperience in Nigeria had shown that on several occasions over the period of a year,such randomly donated RhD-negative units could be found unused in some blood banks in the absence of any needy RhD-negative patient.Such units are eventually used,in a rather less effective way,to transfuse RhD-positive patients in order prevent wastage due to expiry.The best way of handling such redundant units of RhD-negative blood is to store them in the frozen state(cryopreservation),which would allow donor RBCs to be stored for a period of up to10 years,rather than for5weeks in liquid state.21This is an established procedure in countries with developed blood transfusion services.The main indications for RBC cryopreservation includes storage of rare blood groups,extended storage for autologous units,prevention of alloimmunization to HLA antigens in potential bone marrow transplant patients,and prevention of nonhemolytic febrile transfusion reactions.21,34It is therefore possible to continually salvage any redundant RhD-negative RBC units in Nigerian blood banks and cryopre-serve them to create a sustainable reserve that can be thawed for use whenever the need arises. Cryopreservation techniques are being developed in many developing Asian countries such as India, with the long-term objective of offsetting the problems of RhD-negative RBCs and that of other rare blood groups.35,36There is therefore an urgent need for the introduction of RBC cryopreservation techniques in the Nigerian national blood transfu-sion service.THE NIGERIAN NATIONAL BLOODTRANSFUSION SERVICEThe decision to establish a sustainable National Blood Transfusion Service in Nigeria was con-ceived in1975at the World Health Assembly.37 However,since the signing and adoption of the World Health Assembly resolution in1975,very little has been done by successive Nigerian governments to achieve the objectives of establish-ing a National Blood Transfusion Service that could be comparable to what is available in the developed countries of the world.Consequently,the Nigerian Blood Transfusion Service has virtually remained as a hospital-based transfusion service provided by individual hospital blood banks and is characterized by voluntary donor scarcity with predominance of commercial and family donors.8,16,20Nonetheless, the federal government had recently rekindled its commitment by setting up the first blood transfu-sion center in the federal capital,Abuja,in2004.38 This was followed by the establishment of several zonal and state blood transfusion centers across the country.38The Nigerian National Blood Transfu-sion Service,which is administratively under the federal ministry of health,is currently facing many challenges including voluntary donor inertia due to ignorance,economic hardships,and fear of HIV screening in the general population.8,16,20In similarity to many other blood transfusion services in developing countries,inadequate funding is a major problem that militates against optimal performance of the Nigerian National Blood Transfusion Service.33Meanwhile,the Nigerian National Blood transfusion service has gone into partnership with nongovernmental organizations including Safe Blood for Africa Foundation,Center for Disease Control,President's Emergency Plan for AIDS Relief,and the World Health Organiza-tion with the aim of optimizing its services.38CONCLUSIONSThe solution to the problems of RhD-negative donor blood scarcity in Nigeria should be through a multifaceted approach that includes autologous donations,D u testing,inter–blood bank transfers, voluntary RhD-negative donor recall,family dona-tions,and cryopreservation.In addition,there is an urgent need for upgrading and optimizing the capabilities of the Nigerian National Blood Trans-fusion Service.REFERENCES1.Contreras M,Lubenko A:Antigens in human blood.In: Hoffbrand AV,Lewis SM,Tuddenham EGD,editors:Post-graduate haematology.Ed 4.London:Heinemann,2001, pp182-2142.Contreras M,Hewitt PE:Clinical blood transfusion.In: Hoffbrand AV,Lewis SM,Tuddenham EGD,editors:Post-graduate haematology.Ed 4.London:Heinemann,2001, pp215-2343.Enosolease ME,Bazuaye GN:Distribution of ABO and RhD blood groups in the Benin area of Niger-Delta:Implication for regional blood n J Transf Sci2:3-5,20084.Worlledge S,Ogiemudia SE,Thomas CO,et al:Blood group antigens and antibodies in Nigeria.Ann Trop Med Parasitol68:249-264,19745.Ahmed SG,Obi SO:The incidence of ABO and rhesus-D blood groups in northeast Nigeria.Nig J Med7:68-70,1998145RHD NEGATIVE BLOOD IN NIGERIA6.Ahmed SG,Umar BA,Saidu AT,et al:Pattern and clinical significance of ABO and rhesus-D red cell phenotypes among blood donors in Birnin Kudu,Nigeria.Borno Med J 1:1-6,20047.Onwukeme KE:Blood group distribution in blood donors in a Nigerian population.Nig J Physiol Sci6:67-70,19908.Ahmed SG,Ibrahim UA,Hassan AW:Adequacy and pattern of blood donations in northeast Nigeria:The implications for blood safety.Ann Trop Med Parasitol101:725-731,20079.Brozovic B,Brozovic M:Special problems in blood transfusion.In:Brozovic B,Brozovic M,editors:Manual of clinical blood transfusion.Ed1.London:Churchill Livingstone, 1986,pp31-4410.Kruskall MS,Leonard S,Klapholz H:Autologous blood donation during pregnancy:Analysis of safety and blood use. Obstet Gynecol70:938-940,198711.McVay PA,Hoag RW,Hoag MS,et al:Safety and use of autologous donation during the third trimester of pregnancy.Am J Obstet Gynecol160:1479-1488,198912.Ahmed SG:Laboratory strategic defense initiatives against transmission of human immune deficiency virus in blood and blood products.Niger Postgrad Med J10:254-259,200313.Ministerial Task Force on the National Blood Transfusion Sevice:Guidelines on appropriate use of blood and blood products for gos:Federal Ministry of Health;199114.Nwauche CA,Ejele OA:The prevalence of D u phenotype among rhesus D negative females in Port Harcourt,Nigeria.Afr J Reprod Health7:27-31,200315.Kagu MB,Ahmed SG,Olasoji TA:The Prevalence and clinical significance of D u phenotype in rhesus-D negative pregnant women in Maiduguri,Nigeria.Nig J Health Biomed Sci 4:180-182,200516.Egbewale EE,Ogunro PS Muhibi MA:Knowledge, attitude and practice of blood donation in south west Nigeria.Nig Hosp Pract2:132-136,200817.Akinkugbe OO:Sickle cell disease.In:Akinkugbe OO, editor.Non-communicable diseases in gos: Federal Ministry of Health,1992,pp36-4818.Ahmed SG,Ibrahim UA,Kagu MB:The burden of HIV and AIDS on blood bank reserve in northeast Nigeria.Transac Roy Soc Trop Med Hyg101:618-620,200719.Walters AH,Lloyd EE:Laboratory aspects of blood transfusion.In:Dacie JV,Lewis SM,editors:Practical haematology.Ed7.London:Churchill Livingstone,1991, pp455-47620.Ahmed SG,Gamas MG,Kagu MB:Declining frequency of blood donation among elites in Maiduguri,Nigeria.Afr J Med Med Sci35:359-363,200621.Grindon AJ:Blood collection.In:McClatchey KD, editor.Clinical laboratory medicine.Ed1.Baltimore:Williams &Wilkins,1994,pp1687-170022.Cartron JP:Defining the Rh blood group antigens: Biochemistry and molecular genetics.Blood Rev8:199-212, 199423.Kulkarni AG,Ibazebo RO,Dunn DT,et al:Some red cell antigens in the Hausa population of northern Nigeria.Hum Hered35:283-287,198524.Vilmarie R,Heslop HE,Brenner MK,et al:Antigens bone marrow transplantation.In:Hoffbrand AV,Lewis SM, Tuddenham EGD,editors:Postgraduate haematology.Ed4. London:Heinemann,2001,pp530-54925.Brozovic B,Brozovic M:Blood transfusion in transplan-tation.In:Brozovic B,Brozovic M,editors:Manual of clinical blood transfusion.Ed1.London:Churchill Livingstone,1986, pp162-16626.Menitove JE:Complications of blood transfusion.In: McClatchey KD,editor.Clinical laboratory medicine.Ed1. Baltimore:Williams&Wilkins,1994,pp1687-170027.Ruhl H,Bein G,Sachs UJH:Transfusion-associated graft-versus-host disease.Tranfus Med Rev23:62-71,200928.Brozovic B,Brozovic M:Non-haemolytic immune transfusion reactions.In:Brozovic B,Brozovic M,editors: Manual of clinical blood transfusion.Ed1.London:Churchill Livingstone,1986,pp95-10129.Flint J,Harding RM,Boyce AJ,et al:The population genetics of the haemoglobinopathies.Bailliere's Clin Haematol 6:215-222,199330.Ahmed SG,Ibrahim UA:Haemoglobin-S in sickle cell trait with papillary necrosis.Br J Haematol135:415-416,200631.Davies SC,Oni L:Management of sickle cell disease. Br Med J315:656-660,199732.Ahmed SG,Hassan AW,Ibrahim UA:Frequency and clinical significance of structural haemoglobin variants in donor blood at University of Maiduguri Teaching Hospital.Nig J Surg Res2:127-130,200033.Field SP,Allain JP:Transfusion in sub-Saharan Africa:Does a Western model fit?J Clin Pathol60: 1073-1075,200734.Brozovic B,Brozovic M:Whole blood and preparations of red cells.In:Brozovic B,Brozovic M,editors:Manual of clinical blood transfusion.Ed1.London:Churchill Livingstone, 1986,pp20-3035.Nanu A,Lal M:Cryopreservation of Rh negative blood for improved storage and utilisation by means of indigenous freezing bags and solutions and manual deglycerolisation.Indian J Med Res113:151-155,200136.Chaudhari CN:Frozen red blood cells in transfusion. MJAFI65:55-58,200937.World Health Assembly Resolution28.72,1975.38.The Nigerian National Blood Policy:National Blood Transfusion Service.Abuja:Federal Ministry of Health; 2006146SAGIR G.AHMED。
