糖尿病全英文
糖尿病
糖尿病疾病常识英文名称:diabetes mellitus, DM别称:消渴症临床症状:多饮、多食、多尿、乏力并发疾病:肾盂肾炎、膀胱炎、糖尿病酮症酸中毒好发人群:肥胖者、长期高糖、高脂饮食者、直系亲属有糖尿病病史者就诊指南就诊科室:内分泌科治疗周期:需要终身间歇性治疗常用药品:磺酰脲类、二甲双胍、α-葡萄糖苷酶抑制剂、胰岛素增敏常用检查:尿糖测定、口服葡萄糖耐量试验、糖化血红蛋白测定是否医保:是概览定义糖尿病是一组由多病因引起以慢性高血糖为特征的代谢性疾病,是由于膜岛素分泌和(或)利用缺陷所引起。
长期碳水化合物以及脂肪、蛋白质代谢紊乱可引起多系统损害,导致眼、肾、神经、心脏、血管等组织器官慢性进行性病变、功能减退及衰竭;病情严重或应激时可发生急性严重代谢紊乱,如糖尿病酣症酸中毒(DKA)、高渗高血糖综合征。
流行病学糖尿病是常见病、多发病,目前在全球范围内,糖尿病的患病率与发病率极攀升。
1.以2型糖尿病为例,2013年全国调查中2型糖尿病患病率为10.4%,男性高于女性(11.1%比9.6%)。
2.各民族间的糖尿病患病率存在较大差异:满族15.0%、汉族14.7%、维吾尔族12.2%、壮族12.0%、回族10.6%、藏族4.3%。
3.未诊断糖尿病比例较高。
2013年全国调查中,未诊断的糖尿病患者占总数的63%。
4.肥胖和超重人群糖尿病患病率显著增加,肥胖人群糖尿病患病率升高了2倍。
2013年按体质指数(BMI)分层显示,BMI<25 kg/m^2者糖尿病患病率为7.8%、25 kg/m2≤BMI<30 kg/m^2者患病率为15.4%,BMI≥30 kg/m^2者患病率为21.2%。
疾病分类我国目前采用WHO1999年的病因学分型体系,将糖尿病分为以下四大类:1.1型糖尿病:胰岛B细胞破坏,导致胰岛素绝对缺乏。
又分为免疫介导性和特发性(无自身免疫证据)。
2.2型糖尿病:以胰岛素抵抗为主伴胰岛素进行性分泌不足和以胰岛素进行性分泌不足为主伴胰岛素抵抗。
糖尿病英文简介

Diabetes mellitusDiabetes mellitus (DM), commonly referred to as diabetes, is a group of metabolic diseas es in which there are high blood sugar levels over a prolonged period.Symptoms of high blood sugar include frequent urination, increased thirst, and increased hunger. If left untreated, diabetes can cause many complications. Acute complications ca n include diabetic ketoacidosis(酮症酸中毒), nonketotic hyperosmolar coma(高糖昏迷), or death. Serious long-term complications include heart disease, stroke, chronic kidney f ailure, foot ulcers, and damage to the eyes.Diabetes is due to either the pancreas not producing enough insulin or the cells of the body not responding properly to the insulin produced.There are three main types of diab etes mellitus:Type 1 DM results from the pancreas's failure to produce enough insulin.Type 2 DM begins with insulin resistanceGestational diabetes is the third main form and occurs when pregnant women without a previous history of diabetes develop high blood-sugar levels.Prevention and treatment involve maintaining a healthy diet, regular physical exercise, a normal body weight, and avoiding use of tobacco. Control of blood pressure and maintai ning proper foot care are important for people with the disease. Type 1 DM must be m anaged with insulin injections.Type 2 DM may be treated with medications with or witho ut insulin.Insulin and some oral medications can cause low blood sugar.Weight loss surger y in those with obesity is sometimes an effective measure in those with type 2 DM.Gest ational diabetes usually resolves after the birth of the baby.。
英文糖尿病
Etiologic classification of diabetes mellitus(3)
G. Uncommon forms of immune- mediated diabetes 1. “Stiff-man” syndrome 2. Anti-insulin receptor antibodies 3. Others
IFG -FPG≥6.1mmol/L and <7.0mmol/L
Laboratory Findings
Urinary glucose Urinary ketone Blood glucose (FPG and 2-hPG) HbA1c and FA(fructosamine) OGTT Insulin / CP releasing test
•Foot Ulcers •Angina •Heart Attack •Coronary Bypass •Surgery •Stroke •Blindness •Amputation •Dialysis •Kidney Transplant
Diabetes Mellitus
Zhao-xiaojuan
Introduction
Diabetes mellitus is a heterogeneous group of
metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both.
Ranging from predominantly insulin resistance with relative insulin deficiency to predominantly an insulin secretory defect with insulin resistance
糖尿病简介英文版
糖尿病简介英文版Diabetes Mellitus: An OverviewIntroduction:Diabetes Mellitus, commonly known as diabetes, is a chronic metabolic disorder characterized by high blood sugar levels. It affects millions of individuals worldwide and poses a significant healthcare challenge. In this article, we will provide a comprehensive overview of diabetes, its types, causes, symptoms, diagnosis, and management.Types of Diabetes:There are three main types of diabetes: type 1 diabetes, type 2 diabetes, and gestational diabetes.1. Type 1 Diabetes:Type 1 diabetes, also known as insulin-dependent diabetes, typically occurs in children and young adults. It is an autoimmune disease where the body's immune system attacks and destroys the insulin-producing cells in the pancreas. Individuals with type 1 diabetes require lifelong insulin therapy.2. Type 2 Diabetes:Type 2 diabetes, the most common form, occurs when the body becomes resistant to insulin or fails to produce enough insulin to regulate blood sugar levels effectively. It is often associated with obesity, sedentary lifestyle, and poor dietary habits. Initially, it can be managed with lifestyle modifications, including a healthy diet, regular exercise, and possibly oral medications. In severe cases, insulin therapy may be required.3. Gestational Diabetes:Gestational diabetes develops during pregnancy and usually resolves after childbirth. It occurs when hormonal changes during pregnancy lead to insulin resistance. If left uncontrolled, it can pose risks for both the mother and the baby. Proper monitoring and management are crucial to prevent complications.Causes of Diabetes:The causes of diabetes vary depending on the type:1. Type 1 Diabetes:The exact cause of type 1 diabetes is unknown, but it is believed to be a combination of genetic and environmental factors. Certain genes make individuals more susceptible to developing type 1 diabetes, and environmental triggers, such as viral infections, may initiate the autoimmune response.2. Type 2 Diabetes:Type 2 diabetes is primarily attributed to lifestyle factors, including obesity, physical inactivity, unhealthy eating habits, and genetic predisposition. Excessive body weight and abdominal fat accumulation increase insulin resistance, leading to elevated blood sugar levels.3. Gestational Diabetes:The hormonal changes during pregnancy are the main cause of gestational diabetes. These hormones can obstruct the action of insulin, resulting in high blood sugar levels.Symptoms of Diabetes:The symptoms of diabetes can vary, but some common signs include:1. Frequent urination2. Excessive thirst3. Unexplained weight loss4. Fatigue5. Blurred vision6. Slow healing of wounds7. Tingling sensation or numbness in the hands and feetDiagnosis of Diabetes:Diabetes can be diagnosed through various tests, including:1. Fasting Plasma Glucose Test: Measures blood sugar levels after fasting for at least 8 hours.2. Oral Glucose Tolerance Test: Measures blood sugar levels before and 2 hours after consuming a glucose-rich drink.3. Glycated Hemoglobin (HbA1c) Test: Measures average blood sugar levels over the past three months.Management of Diabetes:Diabetes management aims to keep blood sugar levels within the target range to prevent complications. It primarily involves:1. Healthy Eating: A well-balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is essential. Avoiding sugary foods and drinks helps control blood sugar levels.2. Regular Exercise: Engaging in physical activity for at least 150 minutes per week helps improve insulin sensitivity and regulate blood sugar levels.3. Medications: Depending on the type and severity of diabetes, oral medications, injectable drugs, or insulin may be prescribed to manage blood sugar levels effectively.4. Regular Monitoring: Regular monitoring of blood sugar levels and periodic check-ups with healthcare professionals are crucial for adjusting treatment plans and preventing complications.Conclusion:Diabetes Mellitus is a chronic condition requiring lifelong management. Understanding the types, causes, symptoms, diagnosis, and management strategies is crucial in effectively controlling blood sugar levels and preventing complications. By adopting a healthy lifestyle and working closely with healthcare professionals, individuals with diabetes can lead fulfilling lives and minimize the risks associated with the disease.。
糖尿病相关英文词汇

DM相关英文词汇小结1、Diabetes mellitus糖尿病2、hyperglycemia高血糖3、abnormalities异常4、insulin secretion胰岛素分泌5、insulin sensitivity胰岛素敏感性6、microvascular complications微血管并发症7、macrovascular complications大血管并发症8、neuropathic complications神经并发症9、ensue出现、发生10、immune-mediated destruction of pancreatic β -cells免疫介导的胰岛β细胞损伤11、long preclinical period亚临床期长12、transient remission疾病短暂好转13、honeymoon phase蜜月期14、autoantibodies自身抗体15、islet cell antibody胰岛细胞抗体17、insulin antibodies胰岛素抗体18、lipolysis脂肪分解19、free fatty acid production游离脂肪酸生成20、increased hepatic glucose production 肝糖生成增加21、decreased skeletal muscle uptake of glucose肌肉组织对葡萄糖摄取下降22、a diabetogenic lifestyle (excessive calories, inadequate exercise, and obesity)易导致糖尿病的生活方式(能量过度摄入、锻炼不足、肥胖)23、superimposed upon协同24、a susceptible genotype易感基因25、glucocorticoids糖皮质激素26、pentamidine喷她脒27、niacin烟酸28、α-interferonα-干扰素29、Impaired fasting glucose,IFG空腹血糖受损(5、6–6、9 mmol/L)30、impaired glucose tolerance,IGT糖耐量受损(7、8–11、0 mmol/L)31、retinopathyDM视网膜病变32、neuropathyDM神经病变33、nephropathyDM肾病34、coronary heart disease冠心病35、stroke中风36、peripheral vascular disease外周血管病变37、prone to develop diabetic ketoacidosis 自发酮症倾向38、severe stress严重应激39、insulin counterregulatory hormones胰岛素对抗激素40、asymptomatic无症状41、unrelated blood testing随机血糖42、Lethargy无精打采43、polyuria多尿44、nocturia夜尿45、polydipsia烦渴46、Hemoglobin A1C(glycosylated hemoglobin)糖化血红蛋白(≥6、5%为诊断标准) 46、Fasting plasma glucose空腹血糖(≥126 mg/dL (7、0 mmol/L)为诊断标准)47、oral glucose tolerance test (OGTT)口服糖耐量检测48、75 g anhydrous glucose75g无水葡萄糖(折合82、5g一水葡萄糖) 49、Two-hour plasma glucose2小时血糖(≥200 mg/dL (111、1 mmol/L)为诊断标准)50、 A random plasma glucose concentration 随机血糖(≥200 mg/dL (111、1 mmol/L)为诊断标准)51、hyperglycemic crisis高血糖危象52、positive family history家族史阳性53、ameliorate symptoms of hyperglycemia 控制高血糖症状54、Glycemic Goals血糖控制目标55、Preprandial plasma glucose餐前血糖56、Postprandial plasma glucose餐后血糖57、American Association of Clinical Endocrinologists美国临床内分泌医师学会AACE58、American College of Endocrinology 美国内分泌学会ACE59、American Diabetes Association美国糖尿病协会ADA60、aggressive management 强化控制61、smoking cessation戒烟62、treatment of dyslipidemia调节血脂异常63、intensive blood pressure强化血压控制64、antiplatelet therapy抗血小板治疗65、dietary and exercise modifications 改变饮食锻炼习惯66、self-monitoring of blood glucose (SMBG)自我血糖监测67、low in saturated fat饱与脂肪限量68、caloric restriction控制热量69、Bedtime and between meal snacks 睡前及餐间零食70、Aerobic exercise有氧锻炼71、sedentary patients既往运动较少的病人72、atherosclerotic disease动脉粥样硬化疾病73、subcutaneously皮下注射74、Humalog (insulin lispro)赖脯胰岛素(优泌乐®)75、NovoLog (insulin aspart)门冬胰岛素(诺与锐®)76、Apidra (insulin glulisine)赖谷胰岛素(Apidra®,目前还没有中文名) 77、Rapid-acting insulins速效胰岛素78、Short-acting insulins短效胰岛素79、Humulin R (regular)优泌林®R80、Novolin R (regular)诺与灵®R81、Intermediate-acting insulins (neutral protamine Hagedorn)120、Dipeptidyl peptidase-4 (DPP-4) inhibitors二肽基转肽酶-4抑制剂121、Sitagliptin西格列汀(捷诺维®,Januvia®)122、Saxagliptin沙格列汀(安立泽®,Onglyza®)123、Glyburide/metformin格列本脲/二甲双胍(Glucovance®)124、Glipizide/metformin (N) Metaglip格列吡嗪/二甲双胍(Metaglip®)125、Rosiglitazone/metformin罗格列酮/二甲双胍(文达敏®,Avandamet®) 126、long half-life drugs长半衰期药物127、skip meals,误餐128、exercise vigorously高强度锻炼129、skin rash皮疹130、hemolytic anemia溶血性贫血131、GI upset胃肠道不适132、cholestasis胆汁淤积133、Hyponatremia低钠血症134、glucose dependent insulin release葡萄糖依赖的胰岛素释放(格列奈类) 135、the medication should also be skipped 误餐,当餐药物也无需服用136、insulin-sensitive tissues胰岛素敏感组织137、hepatic and peripheral (muscle) tissues肝脏及外周(肌肉)组织138、basal-bolus therapy基础联合餐时胰岛素方案136、glycemic lability、血糖不稳定137、preprandial SMBG level餐前血糖监测水平138、upcoming activity level未来运动量139、anticipated carbohydrate intake预计摄食水平140、Carbohydrate counting碳水化合物计量141、diminish aggregation减少聚集142、greater glycemic control严格控制血糖143、erratic postprandial control餐后血糖控制不佳144、judiciously titrated based on GI adverse effects and postprandial glycemic goals根据胃肠道不良反应及血糖控制水平调整剂量145、Symptomatic patients有症状的患者146、worsen insulin resistance加重胰岛素抵抗147、therapeutic lifestyle measures治疗性生活方式改善148、Obese patients (>120% ideal body weight)肥胖患者(标准体重120%)149、Near-normal-weight patients体重基本正常的患者150、disease progresses on metformin therapy应用二甲双胍期间病情进展151、on multiple therapies正在应用多种治疗方案152、bedtime injection晚间(胰岛素)注射153、Intensify management强化治疗方案154、Less intensive management非强化治疗方案155、intact hypoglycemia awareness有低血糖症状(未受损伤)156、used at the discretion of the clinician 在医师的监护下用药157、ophthalmologist201、fibrate贝特类药物202、polyuria多尿203、polydipsia多饮,烦渴204、Finer insulin adjustments更为精细的血糖调节205、nocturnal sweating夜汗206、palpitations心悸207、microalbuminuria微量白蛋白尿208、albuminuria白蛋白尿209、dilated ophthalmologic exams散瞳查眼底210、influenza and pneumococcal vaccine 流感及肺炎疫苗。
糖尿病英文文章
Diabetes mellitus type 2 (formerly noninsulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes) is a metabolic disorderthat is characterized by high blooglucose in the context of insulin resistance and relative insulin deficiency.[2] This is in contrast todiabetes mellitus type 1, in which there is an absolute insulin deficiency due to destruction of islet cells in t he pancreas.[3] The classic symptoms are excess thirst, frequent urination, and constant hunger. T ype 2 diabetes makes up about 90% of cases of diabetes with the other 10% due primarily to diabe tes mellitus type 1 and gestational diabetes. Obesity is thought to be the primary cause of type 2 di abetes in people who are genetically predisposed to the disease.Type 2 diabetes is initially managed by increasing exercise and dietary modification. If blood glu cose levels are not adequately lowered by these measures, medications suchas metformin or insulin may be needed. In those on insulin, there is typically the requirement to ro utinely check blood sugar levels.Rates of type 2 diabetes have increased markedly over the last 50 years in parallel with obesity: As of 2010 there are approximately 285 million people with the disease compared to around 30 milli on in 1985.[4][5]Long-term complications from high blood sugar can include heart disease,strokes, diabetic retinopathy where eyesight is affected, kidney failurewhich may require d ialysis, and poor circulation of limbs leading toamputations. The acute complication of ketoacidosi s, a feature of type 1 diabetes, is uncommon.[6] However, nonketotic hyperosmolar coma may occ ur.Signs and symptomsOverview of the most significant symptoms of diabetes.The classic symptoms of diabetes are polyuria (frequent urination), polydipsia (increased thirst), p olyphagia (increased hunger), and weight loss.[7] Other symptoms that are commonly present at d iagnosis include: a history of blurred vision,itchiness, peripheral neuropathy,recurrent vaginal infections, and fatigue. Many people, however, have no symptoms during the firs t few years and are diagnosed on routine testing. People with type 2 diabetes mellitus may rarely p resent with nonketotic hyperosmolar coma (a condition of very high blood sugar associated with a decreased level of consciousness and low blood pressure).10 References11 External linksSigns and symptomsOverview of the most significant symptoms of diabetes.The classic symptoms of diabetes are polyuria (frequentComplicationsMain article: Complications of diabetes mellitusType 2 diabetes is typically a chronic disease associated with a ten-year-shorter life expectancy.[4] This is partly due to a number of complications with which it is associated, includi ng: two to four times the risk of cardiovascular disease, includingischemic heart disease and stroke ; a 20-fold increase in lower limb amputations, and increased rates of hospitalizations.[4] In the de veloped world, and increasingly elsewhere, type 2 diabetes is the largest cause of nontraumatic blindnessand kidney failure.[8] It has also been associated with an increased risk of cognitive dysfunction and dementiathrough disease processes such as Alzheimer'disease and vascu lar dementia.[9] Other complications include:acanthosis nigricans, sexual dysfunction, and freque nt infections.[7]causeThe development of type 2 diabetes is caused by a combination of lifestyle and genetic factors.[8][ 10] While some are under personal control, such as diet and obesity, others, such as increasing age , female gender, and genetics, are not.[4] A lack of sleep has been linked to type 2 diabetes.[11] Th is is believed to act through its effect on metabolism.[11] The nutritional status of a mother during fetal development may also play a role, with one proposed mechanism being that of altered DNA methylationgeneticThere are a number of rare cases of diabetes that arise due to an abnormality in a single gen e (known asmonogenic forms of diabetes or "other specific types of diabetes").[3][4] These in clude maturity onset diabetes of the young (MODY), Donohue syndrome,and Rabson-Mendenhall syndrome, among others.[4] Maturity onset diabetes of the young c onstitute 1–5% of all cases of diabetes in young people.[18]Medical conditionsThere are a number of medications and other health problems that can predispose to diabetes.[19] Some of the medications include: glucocorticoids, thiazides, beta blockers, atyp ical antipsychotics,[20] andstatins.[21]Those who have previously had gestational diabetes ar e at a higher risk of developing type 2 diabetes.[7] Other health problems that are associated include: acromegaly, Cushing's syndrome, hyperthyroidism,pheochromocytoma, and certain cancers such as glucagonomas.[19] Testosterone deficiency is also associated with typ e 2 diabetes.[22][23]PathophysiologyType 2 diabetes is due to insufficient insulin production from beta cells in the setting of insuli n resistance.[3] Insulin resistance, which is the inability of cells to respond adequately to nor mal levels of insulin, occurs primarily within the muscles, liver, and fat tissue.[24] In the liver , insulin normally suppresses glucose release. However, in the setting of insulin resistance, th e liver inappropriately releases glucose into the blood.[4] The proportion of insulin resistance versus beta cell dysfunction differs among individuals, with some having primarily insulin resistance and only a minor defect in insulin secretion and others with slight insulin resistance and primarily a lack of insulin secretion.[3] Other potentially important mechanisms associ ated with type 2 diabetes and insulin resistance include: increased breakdown of lipids withi n fat cells, resistance to and lack of incretin, high glucagon levels in the blood, increased rete ntion of salt and water by the kidneys, and inappropriate regulation of metabolism by thecen tral nervous system.[4] However, not all people with insulin resistance develop diabetes, sinc e an impairment of insulin secretion by pancreatic beta cells is also required.[3] DiagnosisThe World Health Organizationdefinition of diabetes (both type 1 and type 2) is for a single raised glucose reading with symptoms, otherwise raised values on two occasions, of either:[2 7]fasting plasma glucose ≥ 7.0 mmol/l (126 mg/dl) orwith a glucose tolerance test, two hours after the oral dose a plasma glucose ≥ 11.1 mmol/ l(200 mg/dl)A random blood sugar of greater than 11.1 mmol/l (200 mg/dL) in association with typical sy mptoms[7] or aglycated hemoglobin (HbA1c) of greater than 6.5% is another method of diag nosing diabetes.[4] In 2009 an International Expert Committee that included representatives of the American Diabetes Association (ADA), the International Diabetes Federation (IDF), a nd the European Association for the Study of Diabetes (EASD) recommended that a threshold of ≥6.5% HbA1c should be used to diagnose diabetes. This recommendation was adopted by the American Diabetes Association in 2010.[28] Positive tests should be repeated unless the perso n presents with typical symptoms and blood sugars >11.1 mmol/l (>200 mg/dl).[29] Threshold for diagnosis of diabetes is based on the relationship between results of glucose tol erance tests, fasting glucose or HbA1c and complications such as retinal problems.[4] A fasti ng or random blood sugar is preferred over the glucose tolerance test, as they are more conv enient for people.[4] HbA1c has the advantages that fasting is not required and results are m ore stable but has the disadvantage that the test is more costly than measurement of blood gl ucose.[30] It is estimated that 20% of people with diabetes in the United States do not realize that they have the disease.[4]Diabetes mellitus type 2 is characterized by high blood glucose in the context of insulin resist ance and relative insulin deficiency.[2] This is in contrast to diabetes mellitus type 1 in which there is an absolute insulin deficiency due to destruction of islet cells inthe pancreas and gestational diabetes mellitus that is a new onset of high blood sugars in ass ociated with pregnancy.[3] Type 1 and type 2 diabetes can typically be distinguished based o n the presenting circumstances.[29] If the diagnosis is in doubt antibody testing may be useful to confirm type 1 diabetes and C-peptide levels may be useful to confirm type 2 diabetes,[31] with C-peptide levels normal or high in type 2 diabetes, but low in type 1 diabet es.ScreeningNo major organization recommends universal screening for diabetes as there is no evidence t hat such a program would improve outcomes.[32] Screening is recommended by the United States Preventive Services Task Force in adults without symptoms whose blood pressure is gr eater than 135/80 mmHg.[33] For those whose blood pressure is less, the evidence is insuffici ent to recommend for or against screening.[33] The World Health Organizationrecommends only testing those groups at high risk.[32] High-risk groups in the United States include: those over 45 years old; those with a first degree relative with diabetes ; some ethnic groups, including Hispanics, African-Americans, and Native-Americans; a hist oryof gestational diabetes; polycystic ovary syndrome; excess weight; and conditions associated with metabolic syndrome.[7]PreventionMain article: Prevention of diabetes mellitus type 2Onset of type 2 diabetes can be delayed or prevented through proper nutrition and regular e xercise.[34][35]Intensive lifestyle measures may reduce the risk by over half.[8] The benefit o f exercise occurs regardless of the person's initial weight or subsequent weight loss.[36] Evid ence for the benefit of dietary changes alone, however, is limited,[37] with some evidence for a diet high in green leafy vegetables[38] and some for limiting the intake of sugary drinks.[13 ] In those with impaired glucose tolerance, diet and exercise either alone or in combination w ith metformin or acarbose may decrease the risk of developing diabetes.[8][39] Lifestyle inte rventions are more effective than metformin.[8]entionMain article: Prevention of diabetes mellitus type 2Onset of type 2 diabetes can be delayed or prevented through proper nutrition and regular exercise .[34][35]Intensive lifestyle measures may reduce the risk by over half.[8] The benefit of exercise o ccurs regardless of the person's initial weight or subsequent weight loss.[36] Evidence for the bene fit of dietary changes alone, however, is limited,[37] with some evidence for a diet high in green le afy vegetables[38] and some for limiting the intake of sugary drinks.[13] In those with impaired gl ucose tolerance, diet and exercise either alone or in combination with metformin or acarbose may decrease the risk of developing diabetes.[8][39] Lifestyle interventions are more effective than met formin.[8]ManagementFurther information: Diabetes managementManagement of type 2 diabetes focuses on lifestyle interventions, lowering other cardiovascularrisk factors, and maintaining blood glucose levels in the normalrange.[8] Self-monitoring of blood glucose for people with newly diagnosed type 2 diabetes was r ecommended by the British National Health Service in 2008,[40] however the benefit of self moni toring in those not using multi-dose insulin is questionable.[8][41] Managing other cardiovascular risk factors, such as hypertension, high cholesterol, and microalbuminuria, improves a person's lif e expectancy.[8] Intensive blood pressure management (less than 130/80 mmHg) as opposed to sta ndard blood pressure management (less than140–160/85–100 mmHg) results in a slight decrease in stroke risk but no effect on overall risk of death.[42] Intensive blood sugar lowering (HbA1c<6%) as opposed to standard blood sugar lowering (HbA1c of 7–7.9%) does not appear to change mortality.[43][44] The goal of treatment is typically an HbA1c of less than 7% or a fasting glucose of less than 6.7 mmol/L (120 mg/dL) however these goals may b e changed after professional clinical consultation, taking into account particular risks of hypoglyce mia and life expectancy.[7] It is recommended that all people with type 2 diabetes get regular opht halmology examination.[3]LifestyleA proper diet and exercise are the foundations of diabetic care,[7] with a greater amount of e xercise yielding better results.[45] Aerobic exercise leads to a decrease in HbA1c and improv ed insulin sensitivity.[45]Resistance training is also useful and the combination of both types ofexercise may be most effective.[45] Adiabetic diet that promotes weight loss is important.[46] While the best diet type to achieve this is controversial[46] a low glycemic index diet has been found to improve blood sugar control.[47] Culturally appropriate education may help people with type 2 diabetes control their blood sugar levels, for up to six months at least.[48] If ch anges in lifestyle in those with mild diabetes has not resulted in improved blood sugars within six weeks, medications should then be considered.[7]MedicationsMetformin 500mg tabletsThere are several classes of anti-diabetic medications available. Metforminis generally recommen ded as a first line treatment as there is some evidence that it decreases mortality.[8] A second oral agent of another class may be used if metformin is not sufficient.[49] Other classes of medications include: sulfonylureas, nonsulfonylurea secretagogues, alpha glucosidase inhibitors, thiazolidined iones, glucagon-like peptide-1 analog, anddipeptidyl peptidase-4 inhibitors.[8][50] Metformin sho uld not be used in those with severe kidney or liver problems.[7] Injections of insulin may either be added to oral medication or used alone.[8]Most people do not initially need insulin.[3] When it is used, a long-acting formulation is typically added at night, with oral medications being continued.[7][8] Doses are then increased to effect (bl ood sugar levels being well controlled).[8] When nightly insulin is insufficient twice daily insulin may achieve better control.[7] The long acting insulins, glargine and detemir, do not appear much better than neutral protamine Hagedorn (NPH) insulin but have a significantly greater cost making them, as of 2010, not cost effective.[51] In those who are pregnant insulin is generally the treatme nt of choice.[7]SurgeryWeight loss surgery in those who are obese is an effective measure to treat diabetes.[52] Many are able to maintain normal blood sugar levels with little or no medications followingsurgery[53] and long term mortality is decreased.[54] There however is some short term mortality risk of less than 1% from the surgery.[55] The body mass index cutoffs for when surgery is approp riate are not yet clear.[54] It however is recommended that this option be considered in those who are unable to get both their weight and blood sugar under control.[56]Prevalence of diabetes worldwide in 2000 (per 1000 inhabitants). World average was 2.8%. Globally as of 2010 it was estimated that there were 285 million people with type 2 diabetes maki ng up about 90% of diabetes cases.[4] This is equivalent to about 6% of the world's adult populati on.[57] Diabetes is common both in the developed and the developing world.[4] It remains uncom mon, however, in the underdeveloped world.[3]Women seem to be at a greater risk as do certain ethnic groups,[4][58] such as South Asians, Pacif ic Islanders, Latinos, and Native Americans.[7] This may be due to enhanced sensitivity to a Weste rn lifestyle in certain ethnic groups.[59] Traditionally considered a disease of adults, type 2 diabete s is increasingly diagnosed in children in parallel withrising obesity rates.[4]Type 2 diabetes is now diagnosed as frequently as type 1 diabetes in teenage rs in the United States.[3]Rates of diabetes in 1985 were estimated at 30 million, increasing to 135 million in 1995 and 217 million in 2005.[5] This increase is believed to be primarily due to the global population aging, a d ecrease in exercise, and increasing rates of obesity.[5] The five countries with the greatest number of people with diabetes as of 2000 are India having 31.7 million, China 20.8 million, the United St ates 17.7 million, Indonesia 8.4 million, and Japan 6.8 million.[60] It is recognized as a global epi demic by the World Health Organization.[61]后面的这个比较简单大白话,-----What is DiabetesIf you have found your way to this page it is probably because you are searching for everything th ere is to know about diabetes. Knowledge is power. You have questions and you need answers to h ave power over this chronic disease.The diseases which are listed under Diabetes Mellitus are many with the most common being Typ e-1 diabetes and Type-2 diabetes. These are diseases of the metabolic system and involve the body 's ability in metabolizing sugar using the hormone insulin. Insulin helps the cells use the simple su gar glucose which is needed for repair, growth and energy.In Type-1 diabetes, the body produces little or no insulin so those with this type of diabetes need t o be on insulin therapy for their entire lives. Before 1924 Type-1 diabetes usually ended with dead after a couple of years but with the advent of insulin those who have this disease are now able to manage this chronic condition. Type-1 diabetes is also known as juvenile diabetes because those w ho have this type of diabetes are usually diagnosed with it between the ages of 9 and 15 years of a ge.With Type-2 diabetes, the body produces plenty of insulin but cells are unable to use it. This type of diabetes is the most common form of diabetes and although it used to normally develop in olde r adults, Type 2 diabetes is now developing at all ages. Major risk factors for Type-2 diabetes are u nhealthy diets, little or no exercise and being overweight or obese. There is currently a world wide epidemic of Type-2 diabetes which researchers believe is being driven in many areas because of s edentary life styles revolving around computers, video games, television and fast foods. Fast food restaurants are now in every corner of ourworld.Diabetes in the USCurrently in the United States 7.8% of the population or around 23.6 million people have diabetes with 5.7 million being undiagnosed. Most of those diagnosed have Type-2 diabetes and are usually 45 years of age or older. But this snapshot is changing as more children and adolescents are increa singly being diagnosed with this type of diabetes.Studies show that the most common complication of Type-2 diabetes is cardiovascular and it is als o the most costly complication at a cost of approximately $7 billion of the $44 billion annual direct medical costs for diabetes. This figure is from 1997 and many estimate that these figures could h ave doubled by now.Diabetes in IndiaAs of 2000 it was estimated that 171 million people globally suffered from diabetes or 2.8% of the population. Type-2 diabetes is the most common type worldwide.Figures for the year 2007 show that the 5 countries with the largest amount of people diagnosed w ith diabetes were India (40.9 million), China (38.9 million), US (19.2 million), Russia (9.6 million ), and Germany (7.4 million).Currently, India is the diabetes capital of the world. It is estimated that over 40 million of those wit h diabetes are currently in India and that by 2025 that number will grow to 70 million. In other wo rds, 1 in every 5 diabetics in the world will live in India. Diabetes is the number one cause of kidn ey failure, is responsible for 5% of blindness in adults and 1 million limb amputations. Because of the chronic nature of diabetes, the relentlessness of its complications and the means re quired to control both diabetes and its complications; this disease is very costly, not only for affect ed individuals and families but also for the healthcare systems. Studies done in India estimate that for a low income family with an adult having diabetes, as much as 25% of the family's income ma y need to be devoted to diabetes care.Stress also seems to be a greater risk factor in India for diabetes. It is important to de-stress accord ing to each one's disposition - for example spending quality time with friends and family, Yoga, br eathing exercises, walking, meditation, aerobics and other fitness regimen can ward off diabetes.Preliminary findings of a recent study in India among school children in the higher socio-economi c group in Chennai showed child obesity is growing higher and girlswere found to be disproportionately "heavier" than boys.Stopping the EpidemicIt is really fairly simple - medical professionals believe that turning off the TV and computer and g oing outside to walk or exercise will go a long way to stopping this epidemic. Other suggestions in clude cutting calories in diets, snacking on whole grain and high-fiber foods, avoiding smoking an d alcohol, exercising regularly and getting stress levels under control are pro-active ways to keep t his diabetic epidemic from continuing to grow.。
diabetes mellitus 翻译

diabetes mellitus 翻译关于糖尿病的介绍糖尿病(diabetes mellitus)是由胰岛素分泌不足或者胰岛素作用异常所导致的一类慢性代谢紊乱疾病。
它的发生机制主要是由于胰岛素分泌不足或作用异常导致人体内的葡萄糖无法被很好的利用,从而导致人体内部的代谢紊乱以及机体的损伤。
糖尿病的分类根据糖尿病的发生机制以及发生时间不同,糖尿病根据其临床表现可以分为1型糖尿病、2型糖尿病以及妊娠期糖尿病等3种类型。
1型糖尿病1型糖尿病,也叫做胰岛素依赖型糖尿病(英文缩写为IDDM),主要是由于免疫系统对胰岛β细胞的破坏导致的胰岛素分泌不足。
患者需要持续注射胰岛素进行控制。
2型糖尿病2型糖尿病,也叫做非胰岛素依赖型糖尿病(英文缩写为NIDDM),主要是由于胰岛素分泌不足以及胰岛素作用异常导致的糖代谢紊乱。
患者可以通过调整饮食、运动以及药物控制血糖。
妊娠期糖尿病妊娠期糖尿病是指孕期发生的糖代谢紊乱,妊娠期糖尿病的特点是妊娠后期症状较明显,出现频率较高,但是大多数患者在产后都会痊愈。
糖尿病的症状表现糖尿病患者会出现头痛、口渴、口干、多饮、多食等症状,还有特别的是尿多、尿频、尿糖、夜尿增多等表现。
如果没有及时有效的治疗,糖尿病会引起严重的健康问题,比如心脏病、脑卒中、肾功能不全、失明、足部坏疽等。
糖尿病的预防和治疗糖尿病的预防和治疗都需要患者保持良好的生活习惯,比如要保持饮食均衡、正常体重、适当运动、不吸烟等。
如果患者已经发生了糖尿病,需要及时的接受医学治疗。
根据不同型号的糖尿病,医生会制定不同的治疗方案,包括饮食调整、运动锻炼和药物治疗等。
总之,糖尿病是一种很危险的疾病,患者需要做好自我管理,加强自我监测和药物治疗,才能够控制病情。
如果出现了糖尿病所引发的严重并发症,那么患者就需要通过手术治疗等手段进行治疗。
因此,及早预防和治疗糖尿病尤为关键。
糖尿病英文文献rd 文档
Jarmuzewska EA,Rocchi R,Mangoni AA.Predictors of impaired blood pressure homeostasis during acute and sustained orthostasis in patients with type 2 diabetes.[J].Panminerva medica,2006,48(1)AIM: Sympathetic failure with acute postural hypotension is a common feature of advanced autonomic neuropathy in type 2 diabetes. It is unknown, however, whether: a) the presence of sympathetic autonomic neuropathy is also a powerful predictor of postural blood pressure changes during sustained orthostasis and b) other factors affecting baroreceptor and neuro-hormonal control might play a role. METHODS: Systolic blood pressure (SBP) was measured during supine rest and after 2, 5, and 20 min of active orthostasis in 45 males with type 2 diabetes (age 56.4+/-8.2 years, mean+/-SD) and different degrees of autonomic neuropathy (absence of neuropathy, n=26, parasympathetic neuropathy, n=9, and sympathetic neuropathy, n=10). Eight healthy subjects (50.1+/-11.6 years) served as controls. A multiple backward regression analysis was performed to identify independent predictors of SBP changes during orthostasis. The regression model included presence/absence of sympathetic autonomic neuropathy, age, diabetes duration, presence/absence of hypertension, baseline SBP and neuro-hormonal parameters (plasma adrenaline, noradrenaline, plasma renin activity, and aldosterone). RESULTS: Sympathetic autonomic neuropathy (P=0.005), baseline SBP (P=0.001), and adrenaline (P=0.003)independently predicted SBP changes after 2 min (R2=0.64); sympathetic autonomic neuropathy (P<0.001), baseline adrenaline (P=0.008), and plasma renin activity (P=0.006) predicted SBP changes after 5 min (R2=0.58); whereas sympathetic autonomic neuropathy (P<0.001) and baseline SBP (P<0.001) predicted SBP changes after 20 min orthostasis (R2=0.65). CONCLUSIONS: The presence of sympathetic autonomic neuropathy and higher supine SBP values remain strong and independent predictors of SBP fall not only during the acute transition from supine to standing position but also during sustained orthostasis in type 2 diabetes. Lower baseline plasma adrenaline concentrations and plasma renin activity are also involv。
糖尿病相关英文词汇

胃排空
103.Sulfonylureas
磺脲类
104.equipotent doses
等效剂量
105.Glipizide
格列吡嗪(普通片,控释片(XL)瑞易宁®)
106.glyburide
格列本脲(普通片:Diabeta®,优降糖®;微乳制剂:Micronase®)
(70% aspart protamine
suspension, 30% aspart)阿福特罗
诺和锐®MIX70/30(70%鱼精蛋白门冬胰岛素;30%门冬胰岛素)
91.NPH-regular combinations
中效-短效组合
92.Humulin 70/30
优泌林®70/30
93.Novolin 70/30
糖化血红蛋白(≥6.5%为诊断标准)
46.Fasting plasma glucose
空腹血糖(≥126 mg/dL (7.0 mmol/L)为诊断标准)
47.oralglucose tolerance test (OGTT)
口服糖耐量检测
48.75 g anhydrous glucose
75g无水葡萄糖(折合82.5g一水葡萄糖)
格列吡嗪/二甲双胍(Metaglip®)
125.Rosiglitazone/metformin
罗格列酮/二甲双胍(文达敏®,Avandamet®)
126.long half-life drugs
长半衰期药物
127.skip meals,
误餐
128.exercise vigorously
高强度锻炼
129.skin rash
易导致糖尿病的生活方式(能量过度摄入、锻炼不足、肥胖)
糖尿病全英文
Postural hypotension
Impotence
Ⅰ、Definition and Types Ⅱ、Signs and symptoms Ⅲ、Diagnosis and Treatment
Time of Check Plasma blood glucose
Range (mmol/l)
Diabetes in Adults )
Ⅱ、Signs and symptoms
About Type 2 diabetes
insufficient insulin Insulin resistance/hyperinsulinemia X Syndrome
insulin resistance hyperlipidimia hypertension obesity(apple figure) coronary heart disease
Ⅱ、Signs and symptoms
Differences between type1 and type2
feature
Type 1
Type 2
Insulin production Age at onset
Physical appearance Symptoms
Treatment
absent
normal or abnormal
insulin
Diabetes complications
Acute decompensation
Hyperosmolar coma
ketoacidosis
chronic complications
nerve damage
Macrovascular disease
医学课件:糖尿病(英文版)

医学课件:糖尿病(英文版) xx年xx月xx日CATALOGUE 目录•糖尿病简介•糖尿病的病因•糖尿病的诊断•糖尿病的治疗•糖尿病的并发症•糖尿病的预防01糖尿病简介Diabetes Mellitus一种慢性、代谢性疾病,由于体内胰岛素绝对或相对不足,导致血糖过高,尿糖排出增加。
发病机制胰岛素抵抗、胰岛素分泌不足、葡萄糖利用障碍糖尿病的定义Type 1 diabetes胰岛素依赖型,由于自身免疫或不明原因导致胰岛素分泌不足。
Type 2 diabetes非胰岛素依赖型,由于生活方式、环境因素导致胰岛素抵抗或分泌不足。
糖尿病的分类糖尿病的症状高血糖、高血脂、高血压多尿、多饮、多食、体重减轻神经病变、心脑血管病变、糖尿病足等视力模糊、伤口愈合缓慢02糖尿病的病因遗传因素类型1糖尿病是一种自身免疫性疾病,受遗传因素的影响,易感人群在病毒感染、化学物质等多种因素的作用下,诱发机体免疫反应,导致胰岛细胞的损伤和破坏。
环境因素环境因素在类型1糖尿病的发病中也起到重要作用,如病毒感染、化学物质等。
类型1糖尿病的病因类型2糖尿病的发生与遗传有关,家族中有患病史的人群患病风险较高。
遗传因素环境因素是类型2糖尿病发病的重要诱因,主要包括缺乏运动、饮食不合理、肥胖、吸烟、饮酒等。
环境因素类型2糖尿病的病因遗传因素妊娠期糖尿病与遗传有关,家族中有糖尿病史的女性患病风险较高。
环境因素妊娠期糖尿病的发生还与多种环境因素有关,如孕期饮食不合理、缺乏运动、肥胖、妊娠期年龄过大等。
妊娠期糖尿病的病因03糖尿病的诊断针对高危人群,如家族遗传史、肥胖、高血压、血脂异常等,应定期进行糖尿病筛查。
糖尿病的筛查常规筛查出现多饮、多尿、多食和不明原因的体重减轻等典型症状,应尽早就医,接受糖尿病筛查。
临床筛查针对妊娠期、老年人、有慢性肾脏疾病或心血管疾病史等特定人群,应根据医生建议进行筛查。
特殊筛查空腹血糖空腹血糖≥7.0 mmol/L,或OGTT试验2小时血糖≥11.1 mmol/L,或随机血糖≥11.1mmol/L,同时伴有典型症状,即可诊断为糖尿病。
关于糖尿病的英文文章
关于糖尿病的英文文章1糖尿病英文简介-What is diabetesDiabetes is a chronic condition that affects over 150 million people inthe world today.The precentage of people suffering from diabetes is increasing rapidly, to the point where many medical authorities are referring to it as an epidemic.So what is diabetes?Diabetes prevents your body from turning your food into energy. Instead glucose stays in your bloodstream, and left untreated can result in a range of complications.If you have recently been diagnosed as diabetic, don't worry. With proper treatment and care, you will lead a normal and happy life. You may need to make a few changes in your lifestyle - but then, if you are like me, you probably had plans to do that anyway and just never got round to it.Now is the time to kick yourself into action. You cannot leave this up to your doctor alone - it needs you to take responsibility for your own treatment, and that starts with understanding what you are dealing with.There are three types of Diabetes:Type 1 Diabetes, sometimes called Juvenile Diabetes is usually found in young children and teenagers, but can also occur later in life.In Type 1 Diabetes, your body is not producing insulin, a hormone neededto convert blood sugar into energy. Normally this hormone is produced by cells in your pancreas, but for some reason this is not happening as it should.As the glucose in your blood can't be converted into energy and absorbedby your cells, it builds up causing high blood sugar.Left untreated, high blood sugar can cause serious long-term health problems.The normal treatment for people with type 1 diabetes is daily injections of insulin which keeps the blood sugar level within normal ranges.Finding out you have diabetes can be upsetting, but it should not prevent you from living a long and happy life.If you think this condition will prevent you leading an active life, consider Sir Steve Redgrave, one of the World's greatest Olympic athletes.Sir Steve battled type 1 diabetes to win his record-breaking fifth Olympic Gold medal at the Sydney games in the coxless fours rowing event!Type 2 diabetes sometimes called mature onset diabetes is the most common form of diabetes.As with Type 1 Diabetes, the problem is related to insulin, a hormone needed to convert sugar into energy.With Type 2 diabetes your body might be producing too little insulin, or it might not be reacting to the insulin correctly. Either way, the end result is that glucose builds up in the bloodstream instead of going into the cells. Left untreated, high blood sugar can cause serious long-term health problems.Type 2 diabetes usually appears later in life, often between the ages of 35-45 years. As it often develops slowly, many people may not recognise the symptoms, and may have diabetes without knowing it.If you have recently been diagnosed with type 2 diabetes, you are one of the lucky ones. Many people have diabetes without knowing it, and are at much greater risk of long term medical complications.Finding out you have diabetes can be upsetting, but it should not prevent you from living a long and happy life. You may need to make a few changes in your lifestyle, but these changes are also good advice for non-diabetics, so probably a good idea anyway.Gestational diabetes is a type of diabetes, that is only suffered by pregnant women.In Ge stational diabetes, a woman’s blood sugar is higher than normal because of the other hormones pridcued during preganancy interfere with the insulin that is produced naturally.Gestational diabetes usually becomes apparent during the 24th to 28th weeks of pregnancy, and, in most cases, disappears of its own accord once the baby is born.Women with gestational diabetes usually do NOT have an increased risk of having a baby with birth defects.Generally, sufferers of gestational diabetes have normal blood sugar levels during the critical first stages of the preganancy.Whilst there can be complications caused by gestational diabetes, these can usually be managed by careful attention to nutrition and blood sugar levels.Approximately 3 to 5 percent of all pregnant women in the developed world suffer from gestational diabetes.2医学英语糖尿病专业词汇A1C –Hemoglobin A1c 醣化血色素A-II receptor antagonist/blockers-ARA [ARB]血管张力素II 接受体拮抗剂/阻断剂A chain,insulin, 胰岛素α链Acanthosis nigrans, 皮肤棘状黑色素瘤Acarbose,一种α-葡萄苷酶抑制剂 ,Acarbose [Glucobay-Bayer]Accountability measures 质量改善度评量ACCU-Check Compact-Roche Diabetes Monitoring Kit 一种携带型血糖机Accupril --Quinapril [Acupril-Parke Davis]之商品名ACEI=ACE inhibitor 血管张力素转化酶抑制剂 [ACEI 非正式名词]ACE inhibitors 血管张力素转化酶抑制剂ACE-K煮甜甜--Acesulfame Potassium [煮甜甜—益富]一种Sweatener 甜味矫味剂Aceon--Perindopril [Aceon-Solvay] [Acertil-Servier]一种血管张力素转换酶抑制剂Acertil--Perindopril [Aceon-Solvay] [Acertil-Servier]一种血管张力素转换酶抑制剂Acesulfame Potassium =ACE-K [煮甜甜—益富]- 一种Sweatener 甜味矫味剂,Adalat--Nifedipine [Adalat-Bayer] [Adalat OROS-Bayer] 一种钙离子径路阻断剂Adalat OROS--Nifedipine[Adalat OROS-Bayer]一种钙离子径路阻断剂长效型Adhesion molecule 黏着分子与动脉硬化形成有关,可被HDL抑制Acertil --Perinodopril [Acertil-Servier]商品名,属于ACE inhibitor用于糖尿肾病变Acetoacetate 乙酰乙酸盐乙酰醋酸Acetohexamide 口服降糖药物 Acetohexamide [Dymelor-Lilly]Acetone 丙酮Acetylsalicylic acid: [Aspirin-Bayer],乙酰水杨酸,阿司匹林Acidosis 酸血症Acipimox [Olbetam-Pharmacia] 烟碱酸类降脂剂Acromegaly肢端肥大症Action--Insulin 胰岛素之作用Actos –Pioglitazone,Insulin sensitizer胰岛素敏感度反应性增强剂新降血糖药物Actrapid Human Insulin-Novo Regular, Human insulin快速作用型人体胰岛素Acute myocardial infarction急性心肌梗塞ADA=American Diabetes Association 美国糖尿病学会Additive--Insulin胰岛素制剂之添加剂ADDQOL=Adult of Diabetes Dependent QOL成人糖尿病相应生活质量Adhesion--Insulin 胰岛素沾粘性Adrenergic blockers交感神经阻断剂Aducut--Delapril [Adecut-武田] 一种血管张力素转换酶抑制剂Adult of Diabetes Dependent QOL=ADDQOL成人糖尿病相应生活质量Adult Treatment Panel III , National Cholesterol education Program =NCEP ATP IIIAER Albumin excretion rate尿液白蛋白排出率感谢您的阅读,祝您生活愉快。
糖尿病相关英文词汇
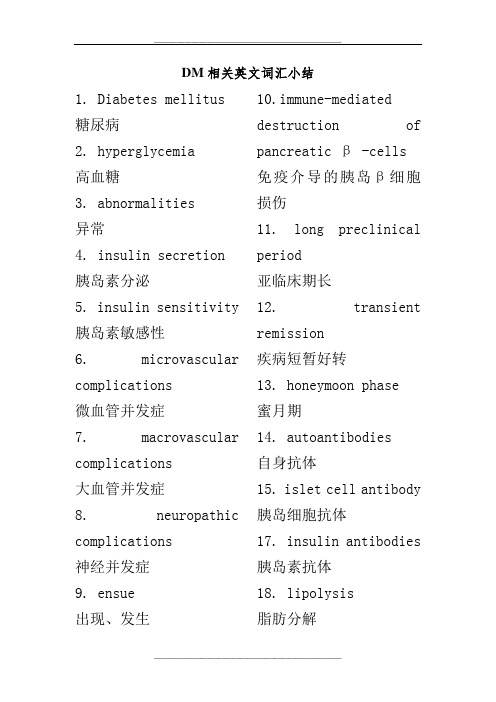
DM相关英文词汇小结1. Diabetes mellitus 糖尿病2. hyperglycemia高血糖3. abnormalities异常4. insulin secretion胰岛素分泌5. insulin sensitivity 胰岛素敏感性6. microvascular complications微血管并发症7. macrovascular complications大血管并发症8. neuropathic complications神经并发症9. ensue出现、发生10.immune-mediated destruction of pancreatic β -cells免疫介导的胰岛β细胞损伤11. long preclinical period亚临床期长12. transient remission疾病短暂好转13. honeymoon phase蜜月期14. autoantibodies自身抗体15. islet cell antibody 胰岛细胞抗体17. insulin antibodies 胰岛素抗体18. lipolysis脂肪分解19. free fatty acid production游离脂肪酸生成20. increased hepatic glucose production肝糖生成增加21.decreased skeletal muscle uptake of glucose肌肉组织对葡萄糖摄取下降22. a diabetogenic lifestyle (excessive calories, inadequate exercise, and obesity)易导致糖尿病的生活方式(能量过度摄入、锻炼不足、肥胖)23. superimposed upon 协同24. a susceptible genotype 易感基因25. glucocorticoids糖皮质激素26. pentamidine喷他脒27. niacin烟酸28. α-interferonα-干扰素29. Impaired fasting glucose,IFG空腹血糖受损(5.6–6.9 mmol/L)30. impaired glucose tolerance,IGT糖耐量受损(7.8–11.0 mmol/L)31. retinopathyDM视网膜病变32. neuropathyDM神经病变33. nephropathyDM肾病34. coronary heart disease冠心病35. stroke中风36. peripheral vascular disease外周血管病变37. prone to develop diabetic ketoacidosis 自发酮症倾向38. severe stress严重应激39. insulin counterregulatory hormones胰岛素对抗激素40. asymptomatic无症状41. unrelated blood testing 随机血糖42. Lethargy无精打采43. polyuria多尿44. nocturia夜尿45. polydipsia烦渴46. Hemoglobin A1C (glycosylated hemoglobin)糖化血红蛋白(≥6.5%为诊断标准)46. Fasting plasma glucose空腹血糖(≥126 mg/dL (7.0 mmol/L)为诊断标准)47. oral glucose tolerance test (OGTT)口服糖耐量检测48. 75 g anhydrous glucose75g无水葡萄糖(折合82.5g一水葡萄糖)49. Two-hour plasma glucose2小时血糖(≥200 mg/dL (111.1 mmol/L)为诊断标准)50. A random plasma glucose concentration 随机血糖(≥200 mg/dL (111.1 mmol/L)为诊断标准)51. hyperglycemic crisis高血糖危象52. positive family history家族史阳性53. ameliorate symptoms of hyperglycemia控制高血糖症状54. Glycemic Goals血糖控制目标55. Preprandial plasma glucose餐前血糖56. Postprandial plasma glucose餐后血糖57. American Association of Clinical Endocrinologists美国临床内分泌医师学会AACE58. American College of Endocrinology美国内分泌学会ACE59. American Diabetes Association美国糖尿病协会ADA60. aggressive management强化控制61. smoking cessation 戒烟62. treatment of dyslipidemia调节血脂异常63. intensive blood pressure强化血压控制64. antiplatelet therapy抗血小板治疗65. dietary and exercise modifications 改变饮食锻炼习惯66. self-monitoring of blood glucose (SMBG)自我血糖监测67. low in saturated fat 饱和脂肪限量68. caloricrestriction控制热量69. Bedtime and between meal snacks睡前及餐间零食70. Aerobic exercise有氧锻炼71. sedentary patients 既往运动较少的病人72. atherosclerotic disease动脉粥样硬化疾病73. subcutaneously皮下注射74. Humalog (insulin lispro)赖脯胰岛素(优泌乐®)75. NovoLog (insulin aspart)门冬胰岛素(诺和锐®)76. Apidra (insulin glulisine)赖谷胰岛素(Apidra®,目前还没有中文名)77. Rapid-acting insulins速效胰岛素78. Short-acting insulins短效胰岛素79. Humulin R (regular)优泌林®R80. Novolin R (regular)诺和灵®R81.Intermediate-acting insulins (neutral protamine Hagedorn)中效胰岛素(中性鱼精蛋白胰岛素,NPH)Hagedorn为发明者名字82. Humulin N 优泌林®N83. Novolin N诺和灵®N84. Long-acting insulins长效胰岛素85. Lantus (insulin glargine)来得时®(甘精胰岛素)86. Levemir (insulin detemir)诺和平®(地特胰岛素)87. Premixed insulins 预混胰岛素88. Humalog Mix 75/25 (75% neutral protamine lispro,25% lispro)优泌乐®MIX75/25(75%鱼精蛋白赖脯胰岛素;25%赖脯胰岛素)89. Humalog Mix 50/50 (50% neutral protaminelispro,50% lispro)优泌乐®MIX50/50(50%中性鱼精蛋白赖脯胰岛素;50%赖脯胰岛素)90. Novolog Mix 70/30 (70% aspart protamine suspension, 30% aspart)阿福特罗诺和锐®MIX70/30(70%鱼精蛋白门冬胰岛素;30%门冬胰岛素)91.NPH-regular combinations中效-短效组合92. Humulin 70/30优泌林®70/3093. Novolin 70/30诺和灵®70/3094. Exenatide (Byetta)艾塞那肽(百泌达)GLP-1 95. Liraglutide (Victoza)利拉鲁肽(诺和力)96. Pramlintide (Symlin)普兰林肽(人胰淀素类似物)97. delayed postmeal hypoglycemia迟发性餐后低血糖98. nocturnal hypoglycemia夜间低血糖99. fasting hyperglycemia空腹高血糖100. Glucagon (1 g intramuscularly)胰高血糖素(肌肉注射)101. Glucagon-like Peptide 1 (GLP-1) Agonists胰高血糖素样肽1激动剂102. gastric emptying胃排空103. Sulfonylureas磺脲类104. equipotent doses 等效剂量105. Glipizide格列吡嗪(普通片,控释片(XL)瑞易宁®)106. glyburide格列本脲(普通片:Diabeta®,优降糖®;微乳制剂:Micron ase®)107. Glimepiride格列美脲(Amaryl®,亚莫利®)108. Short-acting insulin secretagogues 短效胰岛素促泌剂(餐时促泌剂)109. Nateglinide那格列奈(Starlix®,唐力®)110. Repaglinide瑞格列奈(Prandin®,孚来迪®)111. Biguanides双胍类112. Metformin二甲双胍(格华止®,Glucophage®)113. Metformin extended release二甲双胍缓释片(格华止®,Glucophage XR ®)114. Thiazolidinediones噻唑烷二酮类115. Pioglitazone吡格列酮(艾可拓®,Actos®)116. Rosiglitazone 罗格列酮(文迪雅®,Avandia®)117. α-Glucosidaseinhibitorsα-糖苷酶抑制剂118. Acarbose阿卡波糖(拜糖平®,Precose®)119. Miglitol米格列酮(Glyset®)120. Dipeptidyl peptidase-4 (DPP-4) inhibitors二肽基转肽酶-4抑制剂121. Sitagliptin西格列汀(捷诺维®,Januvia®)122. Saxagliptin沙格列汀(安立泽®,Onglyza®)123.Glyburide/metformin 格列本脲/二甲双胍(Glucovance®)124. Glipizide/metformin (N) Metaglip格列吡嗪/二甲双胍(Metaglip®)125.Rosiglitazone/metformin罗格列酮/二甲双胍(文达敏®,Avandamet®)126. long half-life drugs长半衰期药物127. skip meals,误餐128. exercise vigorously高强度锻炼129. skin rash皮疹130. hemolytic anemia溶血性贫血131. GI upset胃肠道不适132. cholestasis胆汁淤积133. Hyponatremia低钠血症134. glucose dependent insulin release葡萄糖依赖的胰岛素释放(格列奈类)135. the medication should also be skipped 误餐,当餐药物也无需服用136. insulin-sensitive tissues胰岛素敏感组织137. hepatic and peripheral (muscle) tissues肝脏及外周(肌肉)组织138. basal-bolus therapy 基础联合餐时胰岛素方案136. glycemiclability.血糖不稳定137. preprandial SMBG level餐前血糖监测水平138. upcoming activity level未来运动量139. anticipated carbohydrate intake预计摄食水平140. Carbohydrate counting碳水化合物计量141. diminish aggregation减少聚集142. greater glycemic control严格控制血糖143. erratic postprandial control 餐后血糖控制不佳144. judiciously titrated based on GI adverse effects and postprandial glycemic goals根据胃肠道不良反应及血糖控制水平调整剂量145. Symptomatic patients有症状的患者146. worsen insulin resistance加重胰岛素抵抗147. therapeutic lifestyle measures治疗性生活方式改善148. Obese patients (>120% ideal body weight)肥胖患者(标准体重120%)149.Near-normal-weight patients体重基本正常的患者150. disease progresses on metformin therapy应用二甲双胍期间病情进展151. on multiple therapies正在应用多种治疗方案152. bedtime injection 晚间(胰岛素)注射153. Intensify management强化治疗方案154. Less intensive management非强化治疗方案155. intact hypoglycemia awareness 有低血糖症状(未受损伤)156. used at the discretion of the clinician在医师的监护下用药157. ophthalmologist 眼科医生158. regress恢复159. Laser photocoagulation激光光凝治疗160. Paresthesias感觉异常161. numbness麻木162. predominant symptoms 主要症状163. tricyclic antidepressants,三环类抗抑郁药物164. anticonvulsants 抗惊厥的药165. gabapentin加巴喷丁166. pregabalin普瑞巴林167. carbamazepine卡巴咪嗪168. topiramate托吡酯169. duloxetine,度洛西汀170. venlafaxine,文拉法辛171. topical capsaicin 辣椒素(表面应用)172. analgesics止痛药173. tramadol曲马多174. Gastroparesis胃瘫175. Erythromycin红霉素176. debilitating使人虚弱的177. metoclopramide甲氧氯普胺178. orthostatic hypotension体位性低血压179. mineralocorticoids盐皮质激素180. Diabetic diarrhea 糖尿病腹泻181. nocturnal夜间(五更泻)182. doxycycline多西环素183. metronidazole甲硝唑184. Octreotide奥曲肽185. Erectile dysfunction勃起功能障碍186. sildenafil西地那非187. vardenafil伐地那非188. tadalafil他达那非189. retarding the progression of established nephropathy延缓神经病变进程190. Diuretics利尿剂191. volume-expanded states容量增加状态192. Claudication跛行193. correction of dyslipidemia纠正血脂异常194. antiplatelet therapy抗血小板治疗195. Cilostazol西洛他唑(Pletal®) 196. select patients 选定的病人197. Local debridement 去死皮198. The National Cholesterol Education Program Adult Treatment Panel III Guidelines国际胆固醇教育项目成人治疗专家指南200. Niacin烟酸201.fibrate贝特类药物202. polyuria多尿203.polydipsia多饮,烦渴204. Finer insulin adjustments更为精细的血糖调节205. nocturnal sweating夜汗206.palpitations心悸207. microalbuminuria 微量白蛋白尿208. albuminuria白蛋白尿209. dilated ophthalmologic exams散瞳查眼底210. influenza and pneumococcal vaccine 流感及肺炎疫苗。
