英文版病例汇报
病历汇报英文演讲稿范文
Good morning. Today, I am honored to present a case report on a patient who recently visited our medical facility. This case highlights a complex medical condition that required a multidisciplinary approach for diagnosis and treatment. I will discuss the patient's history, physical examination findings, laboratory and imaging results, and the subsequent management plan.Patient Information:- Name: John Smith- Age: 45 years- Gender: Male- Date of admission: March 15, 2023- Date of discharge: March 30, 2023Medical History:John Smith presented to our emergency department with a chief complaint of progressive shortness of breath and fatigue over the past two weeks. He reported a history of hypertension and type 2 diabetes mellitus,which were well-controlled on medication. He denied any recent illnesses, fever, cough, or weight loss.Physical Examination:On admission, Mr. Smith was found to have a blood pressure of 160/95 mmHg, heart rate of 110 bpm, respiratory rate of 22 breaths per minute, and tempera ture of 37.2°C. His general appearance was anxious, and he had significant edema in both lower extremities. Cardiovascular examination revealed a grade II/VI systolic ejection murmur at the left sternal border, and pulmonary examination was notable for bilateral wheezing and rales.Laboratory and Imaging Results:- Complete blood count (CBC): Mild anemia with hemoglobin of 10.2 g/dL, white blood cell count of 12,000/µL, and platelet count of 150,000/µL.- Electrolytes, renal function tests, and liver function tests were within normal limits.- Serologic tests for HIV, hepatitis B, and hepatitis C were negative.- Chest X-ray: Bilateral pulmonary edema and cardiomegaly.- Echocardiogram: Severe left ventricular dysfunction with an ejection fraction of 25%.- CT scan of the chest: Pulmonary embolism involving the left main pulmonary artery.Diagnosis:Based on the clinical presentation, laboratory findings, and imaging results, the patient was diagnosed with acute pulmonary embolism (PE) with secondary pulmonary hypertension and left ventricular dysfunction.Management Plan:- Anticoagulation therapy with heparin and apixaban was initiated to prevent further thromboembolic events.- Mechanical ventilation was required due to severe respiratory distress.- Inotropic support was provided to manage hypotension and improve cardiac output.- Treatment for secondary pulmonary hypertension included diuretics, nitrates, and inhaled bronchodilators.- Antibiotics were prescribed for a suspected lower respiratory tract infection.- The patient was also started on a low-sodium diet and received education on fluid management.Outcome:After a week of intensive care, Mr. Smith's clinical status improved significantly. His respiratory distress resolved, and he was able to beweaned off mechanical ventilation. His blood pressure stabilized, and the inotropic support was discontinued. By the time of discharge, his ejection fraction had improved to 30%, and he was discharged on apixaban and hydrochlorothiazide to manage his hypertension and diabetes.Conclusion:This case report illustrates the importance of early diagnosis and treatment of pulmonary embolism, which can be a life-threatening condition. The multidisciplinary approach, including emergency medicine, cardiology, pulmonology, and critical care, was crucial in managing this complex case. Mr. Smith's recovery demonstrates the potential for successful outcomes with appropriate medical intervention.Thank you for your attention, and I would be happy to answer any questions you may have.。
班上学生感冒,头痛等生病情报告英语作文
班上学生感冒,头痛等生病情报告英语作文全文共3篇示例,供读者参考篇1A Wave of Illness Sweeps Through Our ClassroomThe last few weeks have been tough in Mrs. Smith's 4th grade class. It seems like every day another student is out sick with some sort of nasty bug. At first it was just a few kids with the sniffles, but before we knew it, full-blown colds and even cases of the flu started spreading through the classroom like wildfire.It all started about a month ago when Billy came to school with a runny nose and crusty eyes. We didn't think much of it at first - kids get colds all the time, right? But within a couple days, half the class had runny noses, scratchy throats, and were sneezing and coughing up a storm. Mrs. Smith went through box after box of tissues trying to keep up with our drippy noses.I was one of the first to catch the cold from Billy. I remember feeling perfectly fine one day, and then wham! The next morning I woke up with my head completely stuffed up and a raw, tickly throat. My mom made me stay home from school for a few days until the worst of it passed. When I finally went back, it was like ascene from one of those zombie apocalypse movies - half my classmates looked like extras with their glassy eyes, pale faces, and hoarse voices calling out answers.Just when we thought the cold was starting to wind down, the fevers and body aches set in. Jenna was the first to get hit with that terrible flu virus that's been going around. One minute she was her normal bubbly self, and the next she had her head down on her desk, drenched in sweat and shivering like a leaf. Mrs. Smith had to call Jenna's mom to come pick her up. After that, it was like dominoes - kid after kid started calling out sick with the same nasty symptoms.I'll never forget the day when I was one of the only kids left who hadn't gotten the flu. Seven out of the 22 students were home sick! Even Mrs. Smith was feeling under the weather, sniffling and looking drained as she tried to teach the handful of us still healthy enough to make it to class. Let me tell you, it was NOT fun being one of the last "well" ones because that just meant I was next in line to get taken down by the virus. Sure enough, two days later I woke up burning with fever and throwing up. My mom kept me home for almost a week, sipping sprite and sleeping for what felt like days.Finally, after what seemed like months but was really just a few weeks, the sickness started to subside. First Jacob made his way back, then Samantha, then a few others each day until we were almost full force again. You could cut the tension with a knife anytime someone so much as coughed or sniffed - we were all on high alert, afraid that one little sniffle might mean the start of another massive outbreak. Mrs. Smith has been hosing down the classroom with Lysol wipes and bleach every night, desperate to kill any lingering germs.As I look around today at my weary classmates, you can still see the effects of the brutal sickness: dark circles under puffy eyes, pale faces, and a few lingering coughs here and there.We've all vowed to be more diligent about washing our hands and covering coughs and sneezes, having learned our lesson after this harrowing experience. While I'm certainly not eager for a repeat of the last month of illnesses, it has made me more appreciative of my health when I'm feeling good. I'll never take feeling normal for granted again! At least the silver lining is we're all caught up on our Ab Circumfrence division after doing SO many worksheets during our sick days at home. Here's to staying healthy, 4th grade class!篇2Illness Report: Colds, Headaches, and Sick Students in Our ClassIt all started a few weeks ago when Jimmy came to school sniffling and coughing. At first, we didn't think much of it - kids get colds sometimes, no big deal. But then Samantha missed a couple days, saying she had a pounding headache and body aches. Peter was out sick too with the same complaints. That's when we realized something was going around.By the end of that week, it seemed like half the class was out with some kind of nasty bug. I was one of the unlucky ones. It hit me hard - I woke up Thursday morning with my head throbbing, my throat feeling like I had swallowed a cheese grater, and my body so achy I could barely get out of bed. Mom made me stay home and pumped me full of medicine, but it was three miserable days before I finally turned the corner.When I returned to school on Monday, the classroom looked like a ghost town. Only about a third of the students were there. Mrs. Johnson said the attendance office had counted 18 absences just in our class alone that day! She spent the first hour letting those of us who were back go around and share our illness stories. It was pretty crazy to hear how this bug had swept through and taken almost everyone out.Jessica said she lost her voice completely for two days from all the coughing. Jake had missed the big soccer tournament finals because he was running a high fever. Even Mrs. Johnson admitted she had gotten hit with it over the weekend! No wonder she looked worn out.As the week went on, more and more kids filtered back to class looking pretty rough still - pale, bags under their eyes, nasally voices. You could hear the constant chorus of coughing, sniffling, and clearing throats all around the room. The recycling bin overflowed with used tissue boxes.By Thursday, I was one of the only kids who seemed to have fully recovered. I almost didn't recognize some of my classmates who had been so sick - they looked like they had aged 10 years! Sarah's mom actually sent her to school wearing a mask because her cough was so bad. Not going to lie, it was pretty funny to see her muffled voice coming through that thing.Despite everyone being under the weather, we all still had to power through and take the big Math test on Friday. I spent most of the week helping my friend Chris catch up since he had missed so much content while home sick. Poor guy looked completely lost during the test, madly flipping through his notestrying to figure out how to solve the problems. Can't say I envied him having to make all that up.In the end, I'm just glad I'm feeling better and that the worst seems to be over. Although I do keep hearing rumblings about some stomach bug possibly making its way through the upper grades now... Better start stocking up on ginger ale and saltines, just in case! Being stuck at home sick is bad enough without having your head stuck in a toilet all day.This has definitely been one to remember in terms of illness outbreaks at our school. I'll be sure to pack some extra hand sanitizer and vitamin C for a while! Hopefully this was just a weird blip and not a preview of another long flu season. My body can only take so many bugs and missed class time. We've got finals coming up after all - no room for slacking, even if you don't feel well!So there you have it, the full scoop straight from a student's perspective. My advice? If you've managed to stay healthy so far, count your blessings! And maybe invest in one of those full-body anti-germ plastic bubbles to be extra safe...篇3The Classroom Health ReportIt has been a rough few weeks in our classroom lately. A nasty bug seems to be going around, leaving a trail of sniffles, coughs, and misery in its wake. As the designated class health monitor, I've been keeping a close eye on the situation, tracking who is out sick and what symptoms they are experiencing. Let me give you the full rundown.It started about three weeks ago when Tommy caught the first signs of the bug. He came into class looking absolutely dreadful – pale, with bags under his eyes and a persistent cough that had him doubling over every few minutes. The teacher sent him straight to the nurse's office, concerned it might be something serious like bronchitis or pneumonia. Fortunately, the nurse determined it was just a nasty cold and sent him home with instructions to get plenty of rest and fluids.Two days later, Sarah was the next victim. She spent most of the day with her head on her desk, struggling through waves of dizziness, body aches, and a pounding headache. I overheard her describing it as "the worst headache of my life" to our friend Jessica. The nurse suspected Sarah was coming down with a fever and had her picked up to go home and recover.By the end of that first week, Jessica herself had fallen ill with similar symptoms to Sarah – severe headache, fever, chills, andfatigue. She toughed it out and tried to stay for afternoon classes, but ended up getting sent home early when she nearly fainted during math period. Not a good combo with all those numbers to crunch!The following week saw Aiden, Sophia, and Miguel consecutively call out sick with what seemed to be an intense stomach bug. They complained of awful nausea, vomiting, and cramp-like abdomen pains. Definitely a crummy way to spend a few days at home, being stuck next to the toilet. I kept my distance to avoid catching that particular strain!Just when we thought the worst was over, the bug morphed into some sort of hybrid super-cold. First Jake started swearing like a sailor because his throat was so inflamed and scratchy that it hurt to swallow. Then Connor showed up with a fire truck red nose, completely stuffed up and sounding like a trombone player with how much he was having to blow his nose. To top it off, Emma soldiered into class with a raspy voice after losing it completely, only able to communicate in hoarse whispers and written notes.I have to give everyone credit for their resilience in trying to push through and attend class when possible, despite feeling so lousy. Though maybe they shouldn't have, considering howrapidly the sickness starting spreading to even more students. It was like a wasteland of crumpled tissue boxes and emptied cough drop bags littering every classroom by the third week of this plague.Somehow, by the grace of my immune system, I have managed to stay healthy through this entire medical mess so far. My parents always insisted that routinely taking my daily vitamins would pay off, and it seems they were right! While I've felt a little run down from lack of sleep, having to constantly remind sick classmates to cover their coughs and sneezes is a small price to pay. I'll take recess monitor duty for the next month to make up for it!At this point, over half of our class of twenty-five students has missed at least a couple days of school to recover from this sickness that has cycled through colds, fevers, stomach issues, and every kind of symptom in between. Even Mr. Clark, our usually energetic teacher, spent three days out after losing his voice to the plague. We had a substitute rambling on about the Pythagorean Theorem for what felt like an eternity.Hopefully, the worst is behind us. With summer break just a few weeks away, the last thing any of us wants is to spread these bugs to our families over vacation. I've been making sure to wipedown desks and surfaces with disinfectant each day. I also instituted mandatory hand sanitizing stations at the door because let's face it, we all know how bad kids this age can be about washing their hands properly.I just hope my prevention tactics have helped keep the sickness somewhat contained to our classroom. I would feel terrible if I was the one responsible for starting a school-wide outbreak! My anti-bacterial wipe supply is dwindling so I may need to call in reinforcements from the school nurse. Or maybe Mr. Clark can place an emergency supply order from the chemistry stockroom.For now, I'll continue monitoring the situation and reporting back any new developments or worrisome symptoms. Thankfully, it seems the plague has been slowing its relentless march through our classroom in recent days. Fingers crossed we can make it through the remainder of the school year without any other health catastrophes! My little bottle of hand sanitizer and I are certainly ready for summer vacation.。
英语病例报告作文

英语病例报告作文Title: Case Report in English。
Introduction:A case report is an important tool in medical research that documents the clinical presentation, diagnosis, and treatment of a patient. It is a detailed description of a patient's medical history, symptoms, physical examination, laboratory tests, and imaging studies. Case reports are often used to share rare or unusual cases, to describe new diseases or treatments, and to highlight diagnostic challenges or successes. In this article, we will discuss the key components of a case report and provide examples of how they are used in medical research.Case Presentation:The case presentation is the first section of a case report and provides an overview of the patient's medicalhistory, symptoms, and physical examination findings. It should include a brief summary of the patient's demographic information, medical history, and presenting symptoms. For example:A 45-year-old male with a history of hypertension and hyperlipidemia presented to the emergency department with chest pain and shortness of breath. He reported a sudden onset of severe chest pain that radiated to his left arm and jaw. He also complained of difficulty breathing and sweating profusely. On physical examination, he was found to have an elevated blood pressure and heart rate, and crackles were heard in his lungs.Diagnostic Studies:The second section of a case report is the diagnostic studies, which describe the laboratory tests, imaging studies, and other diagnostic procedures used to diagnose the patient's condition. It should include the results of any relevant laboratory tests, such as blood tests, urine tests, or imaging studies, such as X-rays, CT scans, orMRIs. For example:The patient's initial electrocardiogram (ECG) showedST-segment elevation in leads II, III, and aVF, consistent with an acute inferior myocardial infarction. A chest X-ray revealed bilateral pulmonary edema. Blood tests showed elevated troponin levels, indicating myocardial injury.Treatment and Outcome:The third section of a case report is the treatment and outcome, which describes the patient's response totreatment and their overall outcome. It should include a description of the treatment plan, any complications or adverse effects of treatment, and the patient's overall clinical course. For example:The patient was diagnosed with an acute inferior myocardial infarction and was treated with aspirin, heparin, and nitroglycerin. He underwent a cardiac catheterization, which revealed a 90% stenosis in the right coronary artery. The stenosis was successfully treated with percutaneouscoronary intervention (PCI) and a stent was placed. The patient's symptoms improved and he was discharged from the hospital on the third day after admission. He was prescribed antiplatelet and lipid-lowering medications and referred to cardiac rehabilitation.Discussion:The final section of a case report is the discussion, which provides an interpretation of the case and a review of the relevant literature. It should include a discussion of the diagnosis, treatment, and outcome of the case, as well as any relevant differential diagnoses, pathophysiology, or epidemiology. For example:Acute myocardial infarction is a common cause of chest pain and shortness of breath in middle-aged and elderly patients. The classic presentation of myocardial infarction is chest pain, which is often described as pressure or tightness and may radiate to the left arm, jaw, or back. The diagnosis of myocardial infarction is based on clinical presentation, electrocardiogram findings, and cardiacbiomarker levels. The treatment of myocardial infarction includes reperfusion therapy, which can be achieved with either PCI or thrombolytic therapy. The prognosis of myocardial infarction depends on the extent and severity of the myocardial damage and the presence of comorbidities.Conclusion:Case reports are an important tool in medical research that provide valuable insights into the diagnosis, treatment, and outcome of patients with rare or unusual conditions. They can also highlight diagnostic challenges or successes and contribute to the development of new treatments or diagnostic criteria. Writing a case report requires careful attention to detail and adherence to a standardized format. By following the key components of a case report, researchers can effectively communicate their findings and contribute to the advancement of medical knowledge.。
英文病例汇报实用句型
英文病例汇报实用句型1. 一般情况(完全套话)Mr./Ms. **(family name), a **(age) year-old **(profession), was admitted on**(admission date).2. 病史He complains that...He complains of one-month history of palpitation and short of breathness after exertion.He complained about epigastric pain which has lasted for 3 months.He noticed a hardened lump on the left neck 3 months ago.Pancytopenia was found a month ago.He presented with dyspnea since 10 days ago.His chief complaint was ...既往诊疗~~~~~~~~He was confirmed as / definitely diagnosed as ...(确诊为)To make a definite diagnosis, bone marrow aspiration was performed.He was suspected as...(疑似)The discomfort tended to worsening, which urged him to seek for medical care.He has been given 3 cycles of DA regimen for chemotherapy and complete remission was achieved only after the first cycle.He was given the thyroidectomy of the left lobe in local hospital.He was treated with antibiotics (details unknown), which didn't take effect as expected.The general condition is good at present.He was pain free now and hemodynamically stable.3. 查体Nothing noteworthy was found in the physical examination.There was nothing remarkable in the physical examination except for…The physical examination was otherwise normal except that…(上点小菜~~~血液科常见体征)皮肤粘膜generalized pallor,scattered petechiae,oral mucosal hematoma淋巴结enlarged lymph nodes头部yellow eyes (yellow-stained sclera)胸部tenderness in sternum,coarse breath sound, cardiac murmur, arrhythmia腹部enlargement of liver,splenomegaly4.辅助检查The laboratory findings suggested/indicated/demonstrated/showed that…Bone marrow film was performed, which confirmed the diagnosis of ALL.The results of blood routine showed that WBC count was 4,000 /cm3, while NEU count 2,500/cm3, hemoglobin 100 g/L, PLT count 100,000 /cm3.(/cm3 is pronounced as per cubic millimeter)Chest CT scan supported the diagnosis of NHL.Welcome To Download !!!欢迎您的下载,资料仅供参考!。
英文病例写作范文阅读带翻译
英文病例写作范文阅读带翻译病例写作是医生日常的工作,英文的病例该如何写呢,接下来店铺为大家整理英文病例写作范文,希望对你有帮助哦!英文病例写作范文篇一Name: Joe Bloggs (姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Onset: 4 hours of “crushing tight” retrosternal chest pain, radiating to neck and both arms, gradual onset over 5-10 minutes.(起病特征:胸骨后压榨性疼痛4小时,向颈与双臂放射,5-10分钟内渐起病)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
英文病例范文
英文病例范文(中英文版)English Sample Medical Case:John Doe, a 35-year-old male, presented to the emergency department with a chief complaint of severe abdominal pain. The pain started suddenly two hours prior to his arrival and was described as sharp and radiating to his back. Upon examination, his vital signs were stable, but he appeared pale and diaphoretic. The abdomen was tender to palpation, particularly in the upper right quadrant. Laboratory investigations revealed an elevated white blood cell count and increased liver function tests. A diagnosis of acute cholecystitis was suspected, and an ultrasound was ordered to confirm the presence of gallstones.张三,35岁男性,因剧烈腹痛到急诊科就诊。
疼痛在就诊前两小时突然开始,表现为尖锐并向背部放射。
检查时,他的生命体征稳定,但面色苍白且出汗。
腹部触诊时,尤其右上象限区域明显疼痛。
实验室检查显示白细胞计数升高和肝功能测试异常。
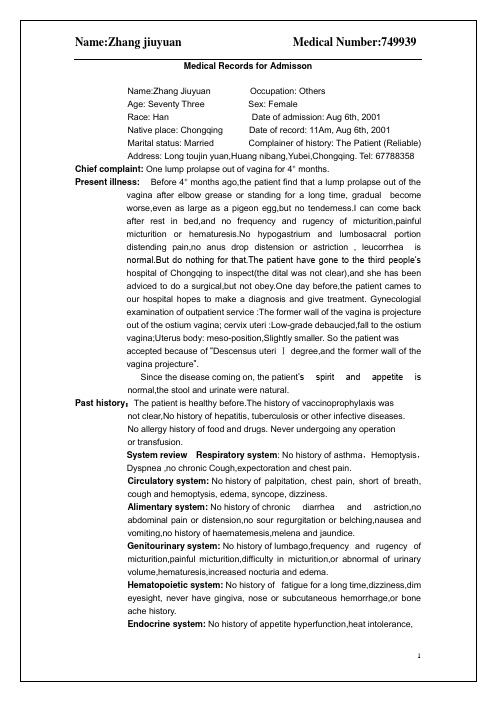
英文完全病历模板-详细版
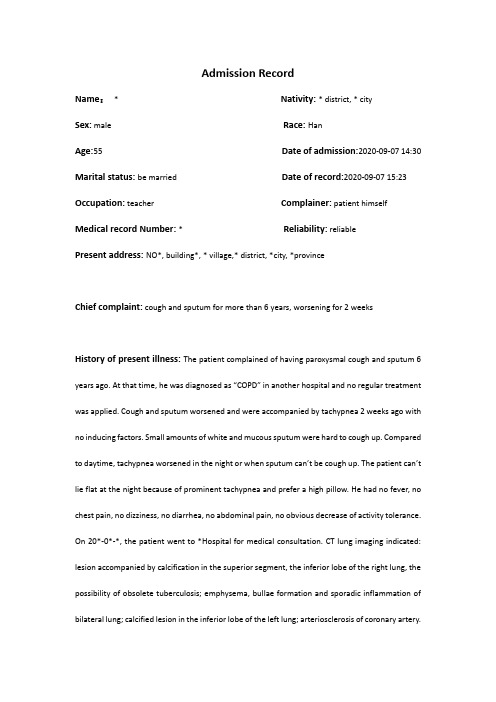
Admission RecordName:* Nativity: * district, * citySex:male Race: HanAge:55 Date of admission:2020-09-07 14:30 Marital status: be married Date of record:2020-09-07 15:23 Occupation:teacher Complainer:patient himself Medical record Number: * Reliability: reliablePresent address: NO*, building*, * village,* district, *city, *provinceChief complaint: cough and sputum for more than 6 years, worsening for 2 weeksHistory of present illness: The patient complained of having paroxysmal cough and sputum 6 years ago. At that time, he was diagnosed as “COPD” in another hospital and no regular treatment was applied. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago with no inducing factors. Small amounts of white and mucous sputum were hard to cough up. Compared to daytime, tachypnea worsened in the night or when sputum can’t be cough up. The patient can’t lie flat at the night because of prominent tachypnea and prefer a high pillow. He had no fever, no chest pain, no dizziness, no diarrhea, no abdominal pain, no obvious decrease of activity tolerance. On 20*-0*-*, the patient went to *Hospital for medical consultation. CT lung imaging indicated: lesion accompanied by calcification in the superior segment, the inferior lobe of the right lung, the possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in the inferior lobe of the left lung; arteriosclerosis of coronary artery.Pulmonary function tests indicated:d obstructive ventilation dysfunction; bronchial dilation test was negative2.moderate decrease of diffusion function, lung volume, residual volume and the ratio of lungvolume; residual volume were normalThe patient was diagnosed as “AECOPD” and prescribed cefoxitin to anti-infection for a week, Budesonide and Formoterol to relieve bronchial muscular spasm and asthma,amb roxol to dilute sputum, and traditional Chinese medicine (specific doses were unknown).The patient was discharged from the hospital after symptoms of cough and sputum slightly relieved with a prescription of using Moxifloxacin outside the hospital for 1 week. Cough and sputum were still existing, thus the patient came to our hospital for further treatment and the outpatient department admitted him in the hospital with “COPD”. His mental status, appetite, sleep, voiding, and stool were normal. No obvious decrease or increase of weight.Past history: The patient was diagnosed as type 2 diabetes 1 years ago and take Saxagliptin (5mg po qd) without regularly monitoring the levels of blood sugar. The patient denies hepatitis, tuberculosis, malaria, hypertension, mental illness, and cardiovascular diseases. Denies surgical procedures, trauma, transfusion, food allergy and drug allergy. The history of preventive inoculation is not quite clear.Personal history: The patient was born in *district, * city and have lived in * since birth. He denies water contact in the schistosome epidemic area. Smoking 10 cigarettes a day for 20 years and have stopped for half a month. Denies excessive drinking and contact with toxics.Marital history: Married at age of 27 and have two daughters. Both the mate and daughters are healthy.Family history: Denies familial hereditary diseases.Physical ExaminationT: 36.5℃ P:77bpm R: 21 breaths/min BP:148/85mmHgGeneral condition:normally developed, well-nourished, normal facies, alert, active position, cooperation is goodSkin and mucosa: no jaundiceSuperficial lymph nodes: no enlargementHead organs: normal shape of headEyes:no edema of eyelids; no exophthalmos; eyeballs move freely; no bleeding spots of conjunctiva; no sclera jaundice; cornea clear; pupils round, symmetrical in size and acutely reactive to light.Ears: no deformity of auricle; no purulent secretion of the external canals; no tenderness over mastoidsNose: normal shape; good ventilation;no nasal ale flap; no tenderness over nasal sinus; Mouth: no cyanosis of lips; no bleeding spots of mouth mucosa; no tremor of tongue; glossy tongue in midline; no pharynx hyperemia; no enlarged tonsils seen and no suppurative excretions; Neck: supple without rigidity, symmetrical; no cervical venous distension; Hepatojugular reflux is negative; no vascular murmur; trachea in midline; no enlargement of thyroid glandChest: symmetrical; no deformity of thoraxLung:Inspection:equal breathing movement on two sidesPalpation: no difference of vocal fremitus over two sides;Percussion: resonance over both lungs;Auscultation: decreased breath sounds over both lungs; no dry or moist rales audible; no pleural friction rubsHeart:Inspection: no pericardial protuberance; Apex beat seen 0.5cm within left mid-clavicular at fifth intercostal space;Palpation: no thrill felt;Percussion: normal dullness of heart bordersAuscultation: heart rate 78bpm; rhythm regular; normal intensity of heart sounds; no murmurs or pericardial friction sound audiblePeripheral vascular sign: no water-hammer pulse; no pistol shot sound; no Duroziez’s murmur; no capillary pulsation sign; no visible pulsation of carotid arteryAbdomen:Inspection: no dilated veins; no abnormal intestinal and peristaltic waves seenPalpation: no tenderness or rebounding tenderness; abdominal wall flat and soft; liver and spleen not palpable; Murphy's sign is negativePercussion: no shifting dullness; no percussion tenderness over the liver and kidney regionAuscultation: normal bowel sounds.External genitalia: uncheckedSpine: normal spinal curvature without deformities; normal movementsExtremities: no clubbed fingers(toes); no redness and swelling of joints; no edema over both legs; no pigmentation of skins of legsNeurological system: normal muscle tone and myodynamia; normal abdominal and bicipital muscular reflex; normal patellar and heel-tap reflex; Babinski sign(-);Kerning sign(-) ; Brudzinski sign(-)Laboratory DataKey Laboratory results including CT imaging and pulmonary function test have been detailed in the part of history of present illness.Abstract*, male, 55 years old. Admitted to our hospital with the chief complaint of cough and sputum for more than 6 years, worsening for 2 weeks. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago. The patient can’t lie flat in the night because of prominent tachypnea and prefer a high pillow.Physical Examination: T: 36.5℃,P: 77bpm, R: 21 breaths per minute, BP:148/85mmHg. Decreased breath sounds over both lungs; no dry or moist rales audible.Laboratory data: CT lung imaging indicates: lesion accompanied by calcification in superior segment, inferior lobe of right lung, possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in inferior lobe of left lung. Pulmonary function tests indicate: mild obstructive ventilation dysfunction, bronchial dilation test was negative moderate decrease of diffusion function.Primary Diagnosis:1.AECOPD2.Type 2 Diabetes3.Primary Hypertension Doctor’s Signature:。
英文病例模版
discharges were found invetibulum nasi. Septum nasi was in midline. No
nares flaring. No tenderness in nasal sinuses.
Superficial lymph nodes:Superficial lymph nodes were not found enlarged.
Head:Cranium:Hair was black and white, well distributed.No deformities. No scars.No pain when we press on. No masses.No tenderness.
Kinetic system:No history of joint pain, numbness,red and swollen,
metallaxis,myalgia or myophagism.
Neural system:No history of long-term headache,dizziness and vertigo,
atage 46.
Marital history:She’s marriedat 28,her husband is heslth,and the relationship
between them were concord.
Childbearing history:G4P2,induced abortion twice,natural labourtwice,and they are heathy.
英文版病例汇报

Chest CT
Chest CT
2015.05.28 Pelvic CT
2015.05.28 Pelvic CT
Present diagnosis
Rectal cancer after resection pT4aN0M0 ⅡB
Liver metastasis
Harbin Medical University cancer hospital
Present history
Tumor marker after Chemotherapy
CEA CA199
2015.05.29
Before chemotherapy
113.2
168.2
135.3
157.7
CEA:0-5ng/ml CA199:0-37U/ml
2015.06.23
1 course later
Harbin Medical University cancer hospital
Present history
Recurrence
• 2015-06-01 Left liver lesion biopsy: Poorly differentiated carcinoma, consistent with metastatic carcinoma.
Harbin Medical University cancer hospital
Present history
Clinical diagnosis based on the pathologic
stage Rectal adenocarcinoma after resection pT4aN0M0 ⅡB
Harbin Medical University cancer hospital
关于三个病人病历的报告英语作文
关于三个病人病历的报告英语作文英文回答:Case 1:A 65-year-old male with a history of hypertension and hyperlipidemia presents with a chief complaint of progressive shortness of breath and fatigue. He has been experiencing exertional dyspnea for the past 6 months, which has gradually worsened over the past few weeks. He now has difficulty walking up a flight of stairs without stopping to rest. He also complains of fatigue and decreased exercise tolerance.Physical examination reveals an obese male with a blood pressure of 150/90 mmHg, a heart rate of 90 bpm, and a respiratory rate of 20 breaths per minute. Auscultation of the chest reveals bibasilar crackles.Chest X-ray shows cardiomegaly and interstitial edema.Echocardiogram demonstrates a left ventricular ejection fraction of 40% and mild mitral regurgitation.Diagnosis:Heart failure with preserved ejection fraction (HFpEF)。
英语病例报告范文

英语病例报告范文I am writing to provide a case report of a patient who presented with symptoms of chest pain and shortness of breath. The patient, a 55-year-old man, arrived at the emergency department complaining of sudden onset chest pain that radiated to his left arm. 本文将介绍一位55岁男性患者的病例报告,该患者出现胸痛和呼吸困难症状。
这位患者突然出现胸痛,疼痛向左臂放射。
Upon arrival, the patient was noted to be diaphoretic and tachypneic, with a blood pressure of 150/90 mmHg and a heart rate of 110 beats per minute. Further assessment revealed he had a history of hypertension and smoking. High-sensitivity troponin levels were elevated, indicating a possible myocardial infarction. 到达医院后,患者被发现出现出汗和呼吸急促的症状,血压为150/90mmHg,心率为每分钟110次。
进一步评估显示他有高血压和吸烟史。
高敏肌钙蛋白水平升高,提示可能发生心肌梗死。
The patient was immediately started on oxygen therapy and given aspirin and nitroglycerin for symptom relief. An ECG showed ST-segment elevations in leads II, III, and aVF, suggestive of an inferiormyocardial infarction. He was promptly taken to the catheterization lab for emergent angiography. 患者立即开始吸氧疗法,并服用阿司匹林和硝化甘油缓解症状。
病人入院报告英文作文
病人入院报告英文作文Patient: Mr. Smith。
Age: 45。
Admission Date: 10/15/2021。
Complaint: Chest pain and shortness of breath。
Physical Examination: 。
Elevated blood pressure。
Rapid heart rate。
Decreased breath sounds in lower right lung。
Swelling in lower extremities。
Diagnostic Tests:EKG: Abnormal ST segment。
Chest X-ray: Right lower lobe pneumonia。
Blood tests: Elevated troponin levels。
Treatment:Oxygen therapy。
IV antibiotics。
Pain management。
Monitoring for cardiac complications。
Prognosis:Guarded due to pneumonia and cardiac involvement。
Close monitoring and aggressive treatment plan in place。
Family Notification:Informed family of patient's condition and treatment plan。
Discharge Planning:Pending improvement in symptoms and stable vital signs。
Education on home care for pneumonia and cardiac monitoring。
Follow-up:Cardiology and pulmonary follow-up appointments scheduled。
case report of XXX(英文病例汇报)

The Third Section of The Department of Gastroenterology
Present illness:
The abdominal CT,MRI and M RCP all showed the dilatation of the bile ducts(both the intrahepatic and extrahepatic bile ducts)and the pancreatic ducts. Besides,the abdominal CT showed the enlargement of pancreas with the probability of pancreatic divisum.Then he was diagnosed as pancreatitis and the sy mptomatic treatment was applie d but the effect was not comfortable.
Sex: Male
Race: Han Nationality: China
father and himself
Reliability: Reliable
Address: XinYang,Henan.
Occupation: Excavator driver
The Third Section of The Department of Gastroenterology
amination report of the duodenal wall showed he was diagnosed T lymphoma.
The Third Section of The Department of Gastroenterology
病理诊断报告单英文模板

病理诊断报告单英文模板Sichuan Provincial People’s HospitalDiagnostic Report on Pathologic Tissues (or Humor)Date when the sample was received:Report No: Surgical xxxx-xx Name of patient : xxxPathologic Findings & Diagnosis Diagnostic conclusion (for the 1st time): chronic cystitis Double-checked the pathologic section of xxxx-xx and found that the wall of the small vessel on the bladder membrana propria thickens, indicating that vasculitis has changed. Inflammatory infiltration of the interstitial tissue is obvious; there are many oxyphil cells. Based on the above changes, I assume that the symptom is resulted from the reaction of illness on connective tissue.Doctor: xxxDate: August xx, xxxxSex : x Age : xHospitalName of department or ward :Out-patient DepartmentHospital bed No .Outpatient or hospitalization No .:Tissue sent for examination :Doctor proposing the examination :Date when the sample was tested:(To be filled by the person sending the sample) Doctor: xxxx Report date: July xx, xxxxFany yi gong si Lian xi fang shi: 6623-7530 2280-118465Sichuan Provincial People’s HospitalDiagnostic Report on Pathologic Tissues (or Humor)Date when the sample was received:Report No: Surgical xxxx-xx Name of patient : xxxPathologic Findings & Diagnosis Diagnostic conclusion : polypous cystitis on the wall of bladder. (There is sub inflammatory reaction close to the intramural area, some lymphocytic infiltration and dropsy; there is no fibroplasias, no obvious intramural inflammation, so the evidence for diagnostic conclusion of interstitial cystitis is not sufficient.)Sex : x Age : xHospital :The present hospitalName of department or ward :Urinary Surgical DepartmentHospital bed No .Outpatient or hospitalization No .:Tissue sent for examination :Doctor proposing the examination :Date when the sample was tested:(To be filled by the person sending the sample) Doctor: xxx Report date: June xx, xxxx。
北大口腔牙周科-英文病例汇报

Name: Niu XXGender: MaleAge: 27 yrBirth: 1989.10Occupation: office staffDate of first visit: 2016.08.02 Case record code:XXXXGum bleeding on brushing occasionally ,for over 6 years⏹Gum bleeding on brushing occasionally⏹mild hypersensitivity to cold⏹No swelling gum⏹No occlusal discomfort⏹Supragingival scaling in other clinic 3weeks agoBrushing teeth twice per day, 3 mins per time, vertical method Using dental flossNon-smokerDental filling treatment of 36systemically healthyNo history of drug allergy No special in family history11 after supragingival scallingAggressive periodontitis(generalized) MalocclusionLingual fossa deformity(#22)Post pulp therapy (#36)?Impacted teeth (#48) and caries(#46 ) Supernumerary tooth✓Favourable factors▪Age▪Compliance —good▪Non-smoker▪Systemically healthy▪Less stress▪Economic status —Fair ▪BMI:21.3✗Adverse factors▪Gingival inflammation (BOP: 100%)▪Deep pocket depth▪Poor bone morphology ▪MalocclusionDeep pocket depthIntrabony defect ——46 Furcation involvement8765432112345678 8765432112345678Excellentpoor/questionableGood/Fair Hopeless /ExtractedControl plaqueElimination of gingival inflammationRestore physiological morphology of the soft and hard tissue Promote the regeneration of periodontal tissueAchieve long-term periodontal health•Periodontal initial therapy•OHI•SRP•Extract (#48)•Endodontic treatment(#22、36、46)•Re-evaluation•Periodontal surgical therapy•surgical treatment•Restorative /Orthodontic PhaseOrthodontic treatment: 3 months intervals •Maintenance Phase2016.08.~2016.09 periodontal initial therapy 2016.11.06 Re-evaluationBeforeBefore6weekslater BOP(+)100%100% PD≧6mm11.9% 1.79% BI≧3100%30.4%OHI reinforcementExtract 48Endodontic treatment(#22、36、46) bone graft +GTR for 46Orthodontic treatmentSupportive periodontal therapy (SPT)2017.01.06-1.20 extracted 48Endodontic treatment(#22、36、46) 2016.03.10bone graft +GTR for 462017.10.12 Orthodontic treatmentbefore Three months laterbeforeBefore3monthslater BOP(+)67.9%53.6% PD≧6mm 1.19% 1.19% BI≧3 5.36%8.93%Three months laterBefore 7months3months8months9months7 months before 9 monthsimmediatelyOHI reinforcementOrthodontic treatment SPT(#47)Before the start of the orthodontic therapy ,the patient needs to demonstrate excellent oral hygiene and gingival and periodontal health.Orthodontic treatment might be terminated if the lack of adequate infection control poses a significant risk of periodontal breakdown.Lang NP,Lindhe J. Clinical periodontology and implantdentistry, 6th ed. 2 Volume-set[M]// Clinical periodontologyand implant dentistry /. Blackwell Munksgaard, 2015.Proposed decision tree for the management of patients with periodontal disease.Geisinger M L, Abou-Arraj R V, Souccar N M, et al. Decision making in the treatment ofThe timing of these procedures is widely varied in the literature, occurring from 10days to 6 months prior to initiation of orthodontic forces Geisinger M L, Abou-Arraj R V, Souccar N M, et al. Decision making in the treatment of patients with malocclusion and chronic periodontitis: Scientific evidence and clinical experience[J]. Seminars in Orthodontics, 2014, 20(3):170-176.。
英文康复病例汇报材料
英文康复病例汇报材料Patient's Information:Name: [Patient's Full Name]Age: [Patient's Age]Gender: [Patient's Gender]Date of Admission: [Admission Date]Date of Discharge: [Discharge Date]Medical Record Number: [Patient's ID/Number]Presenting Complaint:The patient was admitted with complaints of [presenting complaint].Medical History:[Briefly summarize the patient's relevant medical history, including any previous surgeries, chronic conditions, or relevant medications.]Physical Examination Findings:Upon admission, the patient presented with the following physical examination findings:- [List relevant physical examination findings, such as vital signs, general appearance, neurological examination results, etc.] Diagnosis:Based on the patient's medical history, physical examination findings, and relevant investigations, the following diagnosis was made:- [State the primary diagnosis]- [If applicable, mention any secondary diagnoses]Treatment Plan:The patient received the following treatment plan:1. Medications:- [List medications prescribed to the patient]2. Physiotherapy:- [Describe the physiotherapy interventions provided to the patient, including exercises, techniques, and frequency]3. Occupational Therapy:- [Describe the occupational therapy interventions provided to the patient, including activities, adaptations, and frequency]4. Speech Therapy:- [Describe the speech therapy interventions provided to the patient, including exercises, techniques, and frequency]Progress and Outcomes:Throughout the course of treatment, the patient showed the following progress and outcomes:- [Summarize significant improvements or changes observed in the patient's condition]- [Describe any challenges or setbacks encountered during the rehabilitation process]- [Discuss the patient's functional abilities and quality of life at the time of discharge]Patient's Perspective:[If available, include any relevant quotes or remarks from the patient or their family regarding their experience and satisfaction with the rehabilitation process.]Conclusion:In conclusion, the patient presented with [presenting complaint] and received appropriate medical care, including physiotherapy, occupational therapy, and speech therapy. Throughout the rehabilitation process, the patient made progress in terms of [specific improvements]. The patient's functional abilities and quality of life were improved, leading to their eventual discharge. Note: It is important to tailor the above template to the specific details and requirements of the individual case study.。
英语作文一段病人报告
英语作文一段病人报告Patient Report。
Name: [Patient's Name]Age: [Patient's Age]Date: [Date of Report]Chief Complaint:The patient presents with symptoms of persistent cough, accompanied by intermittent fever and fatigue for the past two weeks.History of Present Illness:The patient reports experiencing a gradual onset of symptoms, starting with a mild cough and progressing to a persistent, dry cough. The cough is often worse at nightand is sometimes accompanied by yellowish sputum. Thepatient also complains of intermittent low-grade fever, ranging from 99°F to 100.5°F, which responds temporarilyto over-the-counter antipyretics. Additionally, the patient describes feelings of fatigue and malaise, which have been interfering with daily activities.Past Medical History:The patient has a history of asthma, diagnosed five years ago, for which they use an inhaler as needed. Thereis no history of hospitalizations or surgeries. The patient reports seasonal allergies but denies any other chronic medical conditions.Medications:1. Albuterol inhaler (as needed for asthma symptoms)。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
Harbin Medical University cancer hospital
Present history
Recurrence
• 2015-06-01 Colonoscopy and Chest CT was Tumor Free.
Harbin Medical University cancer hospital
Resection of rectal cancer before 6 years ,with liver metastasis for 1 month.
Harbin Medical University cancer hospital
Present history
Extended radical resection for rectal cancer (Miles ) was performed before 6 years in this hospital. The tumor was located under the peritoneal fold ,with a size of 6*5*7cm, invading wall of intestine.
Present history
Tumor marker after Chemotherapy
CEA CA199
2015.05.29
Before chemotherapy
113.2
168.2
135.3
157.7
CEA:0-5ng/ml CA199:0-37U/ml
2015.06.23
1 course later
Chest CT
Chest CT
2015.05.28 Pelvic CT
2015.05.28 Pelvic CT
Present diagnosis
Rectal cancer after resection pT4aN0M0 ⅡB
Liver metastasis
Harbin Medical University cancer hospital
Harbin Medical University cancer hospital
Following treatment
Resection? Chemotherapy ? Portal vein embolization therapy? Chemotherapy combination with HAI (Hepatic Arterial infusion)?
Portal Phase
Hepatic arterial phase
Present history
Recurrence
• Tumor markers:
CEA 113.2ng/ml(0-5)
CA199 135.3U/ml(0-37)
NSE 23.77ng/ml(0-15.2)
AFP 4.24ng/ml(0-7)
Harbin Medical University cancer hospital
Present history
Recurrence
• 2015-06-01 Left liver lesion biopsy: Poorly differentiated carcinoma, consistent with metastatic carcinoma.
Harbin Medical University cancer hospital
Personal profile
Name:Xing XX
Gender:male Age:63 years old
ECOG:0
Harbin Medical University cancer hospital
Chief complaint
Harbin Medical University cancer hospital
Present history
The pathologic diagnosis • Rectal: moderately differentiated adenocarcinoma and mucinous adenocarcinoma with disc protrude type • Invading wall of intestine • A negative upper margin of resection • Number of positive lymph nodes 0/22
RAS Gene Test
2015-6-11 KRAS/NRAS WT
Harbin Medical University cancer hospital
临床诊断: 直肠癌术后pT4N0M0 ⅡB期 肝转移
Present history
Chemotherapy after Recurrence
Байду номын сангаас
• 肝转移病灶
A metastases with a maximum diameter of 14 cm diameter) was observed in the left lobe of the liver
Harbin Medical University cancer hospital
2015.05.23Plain CT
Harbin Medical University cancer hospital
Present history
Follow up
• 2009.08-2014.05 CEA and CA199 monitoring and routine CT scanning were conducted every 3 month within 2 years and 6 months within 5 years after the surgery. Colonoscopy was performed every year.
Harbin Medical University cancer hospital
Present history
Recurrence
• 2015-05-23 Upper Abdominal Enhancement CT : Liver Metastasis .
Harbin Medical University cancer hospital
Harbin Medical University cancer hospital
Harbin Medical University cancer hospital
Harbin Medical University cancer hospital
Present history
Adjuvant Chemotherapy after surgery
• FOLFOX *8 Cycles Oxaliplatin 200mg d1 ivgtt; Leucovorin 300mg d1-5 ivgtt; 5-Fu 1g d1-5 ivgtt; Repeated every 2weeks
Case Case Report report
Harbin Medical University cancer hospital
A case consultation : Liver metastasis after resection of rectal cancer
HeiLongJiang tumor hospital.China
Harbin Medical University cancer hospital
Present history
Clinical diagnosis based on the pathologic
stage Rectal adenocarcinoma after resection pT4aN0M0 ⅡB
• XELOX *1 Cycles Oxaliplatin 200mg d1 ivgtt; Capecitabine 1500mg am 2000mg pm d1-14 po; Repeated every 3 weeks
Harbin Medical University cancer hospital
