2015美国心肺复苏指南中文版
【7A版】2015美国心肺复苏指南中文版.docx

7A版优质实用文档2015 AMERICAN HEART ASSOCIATION摘要心肺复苏及心血管急救指南更新目录简介 (1)伦理学问题 (2)急救系统和持续质量改进 (3)成人基础生命支持和心肺复苏质量:非专业施救者心肺复苏 ..5 成人基础生命支持和心肺复苏质量:医护人员BLS (7)心肺复苏的替代技术和辅助装置 (11)成人高级心血管生命支持 (13)心脏骤停后救治 (14)急性冠脉综合征 (16)特殊复苏环境 (18)儿科基础生命支持和心肺复苏质量 (20)儿童高级生命支持 (23)新生儿复苏 (25)培训 (27)急救 (29)参考文献 (32)致谢The American Heart Association thanks the following people for their contributions to the development of this publication: Mary Fran Hazinski, RN, MSN; Michael Shuster, MD; Michael W. Donnino, MD; Andrew H. Travers, MD, MSc; Ricardo A. Samson, MD; Steven M. ScheGnayder, MD; Elizabeth H. Sinz, MD; Jeff A. Woodin, NREMT-P; DianneL. Atkins, MD; Farhan Bhanji, MD; Steven C. Brooks, MHSc, MD; Clifton W. Callaway, MD, PhD; Allan R. de Caen, MD; Monica E. Kleinman, MD; Steven L. Kronick, MD, MS; Eric J. Lavonas, MD; Mark S. Link, MD; Mary E. Mancini, RN, PhD; Laurie J. Morrison, MD, MSc; Robert W. Neumar, MD, PhD; Robert E. O’Connor, MD, MPH; Eunice M. Singletary,MD; Myra H. Wyckoff, MD; 和AHA《指南摘要》项目组。
2015心肺复苏指南解

2015更新一
生存链「一分为二」
AHA 成人生存链分为两链:一链为院内急救体系,另
一链为院外急救体系。
2010CPR生存链:早期识别、求救;早期CPR; 早期电除颤;早期高级生命支持
2015更新二
2015更新三
2015更新四
2015更新五 机械胸外按压装置
2015更新六 成人高级心血管生命支持
• 强调按压放松期间的胸壁充分回弹 • 强调AED到场后对可除颤心律立即进行除颤
2015更新七 心脏骤停后救治
BLS人员进行高质量CPR要点总结
更新小结
• 生命链由一变二
• 倡导快速反应体系的建立 • 确定为阿片类中毒时可使用纳洛酮
• 人工气道建立后每6秒1次呼吸
• 强调胸外按压的中断时间10秒内 • 胸外按压的频率次/分
• 胸外按压的深度5-6cm
2015心肺复苏指南解读
急诊科
10月15日,美国心脏协会(AHA)在官方网站及杂志
(Circulation)上公布了《2015心肺复苏指南(CPR)和 心血管急救(ECC)指南更新》。本次更新共包括执行 摘要、证据评价与利益冲突管理、伦理学问题、急救系 统和持续质量改进、成人基础生命支持和心肺复苏质量 (非专业施救者心肺复苏)、成人基础生命支持和心肺 复苏质量(医护人员BLS)、成人高级心血管生命支持、 儿童高级生命支持等15部分文件。
2015 AHA心肺复苏指南

IntroductionPublication of the 2015 American Heart Association (AHA) Guidelines Update for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC) marks 49 years since the first CPR guidelines were published in 1966 by an Ad Hoc Committee on Cardiopulmonary Resuscitation estab-lished by the National Academy of Sciences of the National Research Council.1 Since that time, periodic revisions to the Guidelines have been published by the AHA in 1974,2 1980,3 1986,4 1992,5 2000,6 2005,7 2010,8 and now 2015. The 2010 AHA Guidelines for CPR and ECC provided a comprehensive review of evidence-based recommendations for resuscitation, ECC, and first aid. The 2015 AHA Guidelines Update for CPR and ECC focuses on topics with significant new science or ongoing controversy, and so serves as an update to the 2010 AHA Guidelines for CPR and ECC rather than a complete revision of the Guidelines.The purpose of this Executive Summary is to provide an overview of the new or revised recommendations contained in the 2015 Guidelines Update. This document does not contain extensive reference citations; the reader is referred to Parts 3 through 9 for more detailed review of the scientific evidence and the recommendations on which they are based.There have been several changes to the organization of the 2015 Guidelines Update compared with 2010. “Part 4: Systems of Care and Continuous Quality I mprovement” is an important new Part that focuses on the integrated struc-tures and processes that are necessary to create systems of care for both in-hospital and out-of-hospital resuscitation capable of measuring and improving quality and patient out-comes. This Part replaces the “CPR Overview” Part of the 2010 Guidelines.Another new Part of the 2015 Guidelines Update is “Part 14: Education,” which focuses on evidence-based recommen-dations to facilitate widespread, consistent, efficient and effec-tive implementation of the AHA Guidelines for CPR and ECC into practice. These recommendations will target resuscitationeducation of both lay rescuers and healthcare providers. This Part replaces the 2010 Part titled “Education, Implementation, and Teams.” The 2015 Guidelines Update does not include a separate Part on adult stroke because the content would rep-licate that already offered in the most recent AHA/American Stroke Association guidelines for the management of acute stroke.9,10Finally, the 2015 Guidelines Update marks the begin-ning of a new era for the AHA Guidelines for CPR and ECC, because the Guidelines will transition from a 5-year cycle of periodic revisions and updates to a Web-based format that is continuously updated. The first release of the Web-based inte-grated Guidelines, now available online at is based on the comprehensive 2010 Guidelines plus the 2015 Guidelines Update. Moving forward, these Guidelines will be updated by using a continuous evidence evaluation process to facilitate more rapid translation of new scientific discoveries into daily patient care.Creation of practice guidelines is only 1 link in the chain of knowledge translation that starts with laboratory and clini-cal science and culminates in improved patient outcomes. The AHA ECC Committee has set an impact goal of doubling bystander CPR rates and doubling cardiac arrest survival by 2020. Much work will be needed across the entire spectrum of knowledge translation to reach this important goal.Evidence Review and GuidelinesDevelopment ProcessThe process used to generate the 2015 AHA Guidelines Update for CPR and ECC was significantly different from the process used in prior releases of the Guidelines, and marks the planned transition from a 5-year cycle of evidence review to a continuous evidence evaluation process. The AHA con-tinues to partner with the I nternational Liaison Committee on Resuscitation (I LCOR) in the evidence review process. However, for 2015, ILCOR prioritized topics for systematic review based on clinical significance and availability of new© 2015 American Heart Association, Inc.Circulation is available at DOI: 10.1161/CIR.0000000000000252The American Heart Association requests that this document be cited as follows: Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JME, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Sampson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF. Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation . 2015;132(suppl 2):S315–S367.(Circulation. 2015;132[suppl 2]:S315–S367. DOI: 10.1161/CIR.0000000000000252.)Part 1: Executive Summary2015 American Heart Association Guidelines Update for CardiopulmonaryResuscitation and Emergency Cardiovascular CareRobert W. Neumar, Chair; Michael Shuster; Clifton W. Callaway; Lana M. Gent; Dianne L. Atkins; Farhan Bhanji; Steven C. Brooks; Allan R. de Caen; Michael W. Donnino; Jose Maria E. Ferrer; Monica E. Kleinman; Steven L. Kronick; Eric J. Lavonas; Mark S. Link; Mary E. Mancini; Laurie J. Morrison; Robert E. O’Connor; Ricardo A. Samson; Steven M. Schexnayder;Eunice M. Singletary; Elizabeth H. Sinz; Andrew H. Travers; Myra H. Wyckoff; Mary Fran HazinskiS316 Circulation November 3, 2015evidence. Each priority topic was defined as a question in PICO (population, intervention, comparator, outcome) format. Many of the topics reviewed in 2010 did not have new pub-lished evidence or controversial aspects, so they were not rere-viewed in 2015. In 2015, 165 PICO questions were addressed by systematic reviews, whereas in 2010, 274 PICO questions were addressed by evidence evaluation. In addition, ILCOR adopted the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process for evidence evaluation and expanded the opportunity for public comment. The output of the GRADE process was used to generate the 2015 International Consensus on CPR and ECC Science With Treatment Recommendations (CoSTR).11,12The recommendations of the I LCOR 2015 CoSTR were used to inform the recommendations in the 2015 AHA Guidelines Update for CPR and ECC. The wording of these recommendations is based on the AHA classification system for evidentiary review (see “Part 2: Evidence Evaluation and Management of Conflicts of Interest”).The 2015 AHA Guidelines Update for CPR and ECC con-tains 315 classified recommendations. There are 78 Class I rec-ommendations (25%), 217 Class II recommendations (68%), and 20 Class III recommendations (7%). Overall, 3 (1%) are based on Level of Evidence (LOE) A, 50 (15%) are based on LOE B-R (randomized studies), 46 (15%) are based on LOE B-NR (non-randomized studies), 145 (46%) are based on LOE C-LD (lim-ited data), and 73 (23%) are based on LOE C-EO (consensus of expert opinion). These results highlight the persistent knowledge gap in resuscitation science that needs to be addressed through expanded research initiatives and funding opportunities.As noted above, the transition from a 5-year cycle to a continuous evidence evaluation and Guidelines update process will be initiated by the 2015 online publication of the AHA I ntegrated Guidelines for CPR and ECC at ECCguidelines. . The initial content will be a compilation of the 2010 Guidelines and the 2015 Guidelines Update. In the future, the Scientific Evidence Evaluation and Review System (SEERS) Web-based resource will also be periodically updated with results of the ILCOR continuous evidence evaluation process at /seers.Part 3: Ethical IssuesAs resuscitation practice evolves, ethical considerations must also evolve. Managing the multiple decisions associated with resuscitation is challenging from many perspectives, espe-cially when healthcare providers are dealing with the ethics surrounding decisions to provide or withhold emergency car-diovascular interventions.Ethical issues surrounding resuscitation are complex and vary across settings (in or out of hospital), providers (basic or advanced), patient population (neonatal, pediatric, or adult), and whether to start or when to terminate CPR. Although the ethical principles involved have not changed dramatically since the 2010 Guidelines were published, the data that inform many ethical discussions have been updated through the evi-dence review process. The 2015 ILCOR evidence review pro-cess and resultant 2015 Guidelines Update include several recommendations that have implications for ethical decision making in these challenging areas.Significant New and Updated Recommendations That May Inform Ethical Decisions• The use of extracorporeal CPR (ECPR) for cardiac arrest • Intra-arrest prognostic factors for infants, children, and adults• Prognostication for newborns, infants, children, and adults after cardiac arrest• Function of transplanted organs recovered after cardiac arrestNew resuscitation strategies, such as ECPR, have made the decision to discontinue cardiac arrest measures more complicated (see “Part 6: Alternative Techniques and Ancillary Devices for Cardiopulmonary Resuscitation” and “Part 7: Adult Advanced Cardiovascular Life Support”). Understanding the appropriate use, implications, and likely benefits related to such new treat-ments will have an impact on decision making. There is new information regarding prognostication for newborns, infants, children, and adults with cardiac arrest and/or after cardiac arrest (see “Part 13: Neonatal Resuscitation,” “Part 12: Pediatric Advanced Life Support,” and “Part 8: Post–Cardiac Arrest Care”). The increased use of targeted temperature management has led to new challenges for predicting neurologic outcomes in comatose post–cardiac arrest patients, and the latest data about the accuracy of particular tests and studies should be used to guide decisions about goals of care and limiting interventions.With new information about the success rate for trans-planted organs obtained from victims of cardiac arrest, there is ongoing discussion about the ethical implications around organ donation in an emergency setting. Some of the different view-points on important ethical concerns are summarized in “Part 3: Ethical I ssues.” There is also an enhanced awareness that although children and adolescents cannot make legally bind-ing decisions, information should be shared with them to the extent possible, using appropriate language and information for their level of development. Finally, the phrase “limitations of care” has been changed to “limitations of interventions,” and there is increasing availability of the Physician Orders for Life-Sustaining Treatment (POLST) form, a new method of legally identifying people who wish to have specific limits on interven-tions at the end of life, both in and out of healthcare facilities.Part 4: Systems of Care andContinuous Quality ImprovementAlmost all aspects of resuscitation, from recognition of cardio-pulmonary compromise, through cardiac arrest and resuscita-tion and post–cardiac arrest care, to the return to productive life, can be discussed in terms of a system or systems of care. Systems of care consist of multiple working parts that are interdependent, each having an effect on every other aspect of the care within that system. To bring about any improvement, providers must recognize the interdependency of the various parts of the system. There is also increasing recognition that out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA) systems of care must function differently. “Part 4: Systems of Care and Continuous Quality I mprovement” in this 2015 Guidelines Update makes a clear distinction between the two systems, noting that OHCA frequently is the result of an unexpected event with a reactive element, whereasNeumar et al Part 1: Executive Summary S317the focus on IHCA is shifting from reactive resuscitation to prevention. New Chains of Survival are suggested for in-hospital and out-of-hospital systems of care, with relatively recent in-hospital focus on prevention of arrests. Additional emphasis should be on continuous quality improvement by identifying the problem that is limiting survival, and then by setting goals, measuring progress toward those goals, creating accountability, and having a method to effect change in order to improve outcomes.This new Part of the AHA Guidelines for CPR and ECC summarizes the evidence reviewed in 2015 with a focus on the systems of care for both I HCA and OHCA, and it lays the framework for future efforts to improve these systems of care. A universal taxonomy of systems of care is proposed for stakeholders. There are evidence-based recommendations on how to improve these systems.Significant New and Updated RecommendationsI n a randomized trial, social media was used by dispatch-ers to notify nearby potential rescuers of a possible cardiac arrest. Although few patients ultimately received CPR from volunteers dispatched by the notification system, there was a higher rate of bystander-initiated CPR (62% versus 48% in the control group).13 Given the low risk of harm and the poten-tial benefit of such notifications, municipalities could consider incorporating these technologies into their OHCA system of care. I t may be reasonable for communities to incorporate, where available, social media technologies that summon res-cuers who are willing and able to perform CPR and are in close proximity to a suspected victim of OHCA (Class I I b, LOE B-R).Specialized cardiac arrest centers can provide comprehen-sive care to patients after resuscitation from cardiac arrest. These specialized centers have been proposed, and new evi-dence suggests that a regionalized approach to OHCA resus-citation may be considered that includes the use of cardiac resuscitation centers.A variety of early warning scores are available to help identify adult and pediatric patients at risk for deterioration. Medical emergency teams or rapid response teams have been developed to help respond to patients who are deteriorating. Use of scoring systems to identify these patients and creation of teams to respond to those scores or other indicators of deterioration may be considered, particularly on general care wards for adults and for children with high-risk illnesses, and may help reduce the incidence of cardiac arrest.Evidence regarding the use of public access defibrillation was reviewed, and the use of automated external defibril-lators (AEDs) by laypersons continues to improve survival from OHCA. We continue to recommend implementation of public access defibrillation programs for treatment of patients with OHCA in communities who have persons at risk for cardiac arrest.Knowledge Gaps• What is the optimal model for rapid response teams in the prevention of IHCA, and is there evidence that rapid response teams improve outcomes?• What are the most effective methods for increasing bystander CPR for OHCA?• What is the best composition for a team that responds to IHCA, and what is the most appropriate training for that team?Part 5: Adult Basic Life Support andCardiopulmonary Resuscitation Quality New Developments in Basic Life Support Science Since 2010The 2010 Guidelines were most notable for the reorientation of the universal sequence from A-B-C (Airway, Breathing, Compressions) to C-A-B (Compressions, Airway, Breathing) to minimize time to initiation of chest compressions. Since 2010, the importance of high-quality chest compressions has been reemphasized, and targets for compression rate and depth have been further refined by relevant evidence. For the untrained lay rescuer, dispatchers play a key role in the recognition of abnor-mal breathing or agonal gasps as signs of cardiac arrest, with recommendations for chest compression–only CPR.This section presents the updated recommendations for the 2015 adult basic life support (BLS) guidelines for lay res-cuers and healthcare providers. Key changes and continued points of emphasis in this 2015 Guidelines Update include the following: The crucial links in the adult Chain of Survival for OHCA are unchanged from 2010; however, there is increased emphasis on the rapid identification of potential cardiac arrest by dispatchers, with immediate provision of CPR instructions to the caller. These Guidelines take into consideration the ubiq-uitous presence of mobile phones that can allow the rescuer to activate the emergency response system without leaving the victim’s side. For healthcare providers, these recommenda-tions allow flexibility for activation of the emergency response to better match the provider’s clinical setting. More data are available indicating that high-quality CPR improves survival from cardiac arrest. Components of high-quality CPR include • Ensuring chest compressions of adequate rate• Ensuring chest compressions of adequate depth• Allowing full chest recoil between compressions• Minimizing interruptions in chest compressions• Avoiding excessive ventilationRecommendations are made for a simultaneous, choreo-graphed approach to performance of chest compressions, airway management, rescue breathing, rhythm detection, and shock delivery (if indicated) by an integrated team of highly trained rescuers in applicable settings.Significant New and Updated Recommendations Many studies have documented that the most common errors of resuscitation are inadequate compression rate and depth; both errors may reduce survival. New to this 2015 Guidelines Update are upper limits of recommended compression rate based on pre-liminary data suggesting that excessive rate may be associated with lower rate of return of spontaneous circulation (ROSC). In addition, an upper limit of compression depth is introducedS318 Circulation November 3, 2015based on a report associating increased non–life-threatening injuries with excessive compression depth.• I n adult victims of cardiac arrest, it is reasonable for rescuers to perform chest compressions at a rate of 100 to 120/min (Class IIa, LOE C-LD). The addition of an upper limit of compression rate is the result of 1 large registry study associating extremely rapid compression rates with inadequate compression depth.• During manual CPR, rescuers should perform chest compressions at a depth of at least 2 inches or 5 cm for an average adult, while avoiding excessive chest com-pression depths (greater than 2.4 inches [6 cm]) (Class I, LOE C-LD). The addition of an upper limit of com-pression depth followed review of 1 publication suggest-ing potential harm from excessive chest compression depth (greater than 6 cm, or 2.4 inches). Compression depth may be difficult to judge without use of feedback devices, and identification of upper limits of compres-sion depth may be challenging.• I n adult cardiac arrest, total preshock and postshock pauses in chest compressions should be as short as pos-sible (Class I, LOE C-LD) because shorter pauses can be associated with greater shock success, ROSC, and, in some studies, higher survival to hospital discharge. The need to reduce such pauses has received greater empha-sis in this 2015 Guidelines Update.• In adult cardiac arrest with an unprotected airway, it may be reasonable to perform CPR with the goal of a chest compression fraction as high as possible, with a target of at least 60% (Class IIb, LOE C-LD). The addition of this target compression fraction to the 2015 Guidelines Update is intended to limit interruptions in compressions and to maximize coronary perfusion and blood flow during CPR.• For patients with known or suspected opioid addic-tion who have a definite pulse but no normal breathing or only gasping (ie, a respiratory arrest), in addition to providing standard BLS care, it is reasonable for appro-priately trained BLS providers to administer intramus-cular or intranasal naloxone (Class IIa, LOE C-LD). It is reasonable to provide opioid overdose response educa-tion with or without naloxone distribution to persons at risk for opioid overdose in any setting (Class IIa, LOE C-LD). For more information, see “Part 10: Special Circumstances of Resuscitation.”• For witnessed OHCA with a shockable rhythm, it may be reasonable for emergency medical service (EMS) systems with priority-based, multi-tiered response to delay positive-pressure ventilation by using a strategy of up to 3 cycles of 200 continuous compressions with passive oxygen insufflation and airway adjuncts (Class IIb, LOE C-LD).• We do not recommend the routine use of passive ven-tilation techniques during conventional CPR for adults, because the usefulness/effectiveness of these techniques is unknown (Class IIb, LOE C-EO). However, in EMS systems that use bundles of care involving continuous chest compressions, the use of passive ventilation tech-niques may be considered as part of that bundle (Class IIb, LOE C-LD).• I t is recommended that emergency dispatchers deter-mine if a patient is unconscious with abnormal breathingafter acquiring the requisite information to determine the location of the event (Class I, LOE C-LD).• I f the patient is unconscious with abnormal or absent breathing, it is reasonable for the emergency dispatcher to assume that the patient is in cardiac arrest (Class IIa, LOE C-LD).• Dispatchers should be educated to identify unconscious-ness with abnormal and agonal gasps across a range of clin-ical presentations and descriptions (Class I, LOE C-LD).• We recommend that dispatchers should provide chest compression–only CPR instructions to callers for adults with suspected OHCA (Class I, LOE C-LD).• It is reasonable for healthcare providers to provide chest compressions and ventilation for all adult patients in cardiacarrest, from either a cardiac or a noncardiac cause (Class IIb, LOE C-LD). When the victim has an advanced airway in place during CPR, rescuers no longer deliver cycles of30 compressions and 2 breaths (ie, they no longer interruptcompressions to deliver 2 breaths). Instead, it may be rea-sonable for the provider to deliver 1 breath every 6 seconds(10 breaths per minute) while continuous chest compres-sions are being performed (Class IIb, LOE C-LD). When the victim has an advanced airway in place during CPR, it may be reasonable for the provider to deliver 1 breath every 6 seconds (10 breaths per minute) while continuous chest compressions are being performed (Class IIb, LOE C-LD). This simple rate, rather than a range of breaths per minute, should be easier to learn, remember, and perform.• There is insufficient evidence to recommend the use of artifact-filtering algorithms for analysis of electrocardio-graphic (ECG) rhythm during CPR. Their use may be con-sidered as part of a research program or if an EMS system has already incorporated ECG artifact-filtering algorithms in its resuscitation protocols (Class IIb, LOE C-EO).• It may be reasonable to use audiovisual feedback devices during CPR for real-time optimization of CPR perfor-mance (Class IIb, LOE B-R).• For victims with suspected spinal injury, rescuers should initially use manual spinal motion restriction (eg, plac-ing 1 hand on either side of the patient’s head to hold it still) rather than immobilization devices, because use of immobilization devices by lay rescuers may be harmful (Class III: Harm, LOE C-LD).Knowledge Gaps• The optimal method for ensuring adequate depth of chest compressions during manual CPR• The duration of chest compressions after which venti-lation should be incorporated when using Hands-Only CPR• The optimal chest compression fraction• Optimal use of CPR feedback devices to increase patient survivalPart 6: Alternative Techniques and Ancillary Devices for Cardiopulmonary Resuscitation High-quality conventional CPR (manual chest compressions with rescue breaths) generates about 25% to 33% of normal cardiac output and oxygen delivery. A variety of alternativesNeumar et al Part 1: Executive Summary S319and adjuncts to conventional CPR have been developed with the aim of enhancing coronary and cerebral perfusion during resuscitation from cardiac arrest. Since the 2010 Guidelines were published, a number of clinical trials have provided new data regarding the effectiveness of these alternatives. Compared with conventional CPR, many of these techniques and devices require specialized equipment and training. Some have been tested in only highly selected subgroups of cardiac arrest patients; this selection must be noted when rescuers or healthcare systems consider implementation of the devices. Significant New and Updated Recommendations• The Resuscitation Outcomes Consortium (ROC) Prehospital Resuscitation mpedance V alve and EarlyV ersus Delayed Analysis (PRI MED) study (n=8718)14failed to demonstrate improved outcomes with the use ofan impedance threshold device (ITD) as an adjunct to con-ventional CPR when compared with use of a sham device.This negative high-quality study prompted a Class III: NoBenefit recommendation regarding routine use of the ITD.• One large randomized controlled trial evaluated the use ofactive compression-decompression CPR plus an ITD.15 Thewriting group found interpretation of the true clinical effectof active compression-decompression CPR plus an I TDchallenging because of wide confidence intervals aroundthe effect estimate and also because of methodological con-cerns. The finding of improved neurologically intact sur-vival in the study, however, supported a recommendationthat this combination may be a reasonable alternative withavailable equipment and properly trained providers.• Three randomized clinical trials comparing the use ofmechanical chest compression devices with conventionalCPR have been published since the 2010 Guidelines.None of these studies demonstrated superiority ofmechanical chest compressions over conventional CPR.Manual chest compressions remain the standard of carefor the treatment of cardiac arrest, but mechanical chestcompression devices may be a reasonable alternativefor use by properly trained personnel. The use of themechanical chest compression devices may be consid-ered in specific settings where the delivery of high-qualitymanual compressions may be challenging or dangerousfor the provider (eg, prolonged CPR during hypothermiccardiac arrest, CPR in a moving ambulance, CPR in theangiography suite, CPR during preparation for ECPR),provided that rescuers strictly limit interruptions in CPRduring deployment and removal of the device (Class IIb,LOE C-EO).• Although several observational studies have been pub-lished documenting the use of ECPR, no randomizedcontrolled trials have evaluated the effect of this therapyon survival.Knowledge Gaps• Are mechanical chest compression devices superior tomanual chest compressions in special situations suchas a moving ambulance, prolonged CPR, or proceduressuch as coronary angiography?• What is the impact of implementing ECPR as part of thesystem of care for OHCA?Part 7: Adult AdvancedCardiovascular Life SupportThe major changes in the 2015 advanced cardiovascular life support (ACLS) guidelines include recommendations regard-ing prognostication during CPR based on end-tidal carbon dioxide measurements, use of vasopressin during resuscita-tion, timing of epinephrine administration stratified by shock-able or nonshockable rhythms, and the possibility of bundling steroids, vasopressin, and epinephrine administration for treatment of IHCA. In addition, vasopressin has been removed from the pulseless arrest algorithm. Recommendations regard-ing physiologic monitoring of CPR were reviewed, although there is little new evidence.Significant New and Updated Recommendations • Based on new data, the recommendation for use of the maximal feasible inspired oxygen during CPR was strengthened. This recommendation applies only while CPR is ongoing and does not apply to care afterROSC.• The new 2015 Guidelines Update continues to state that physiologic monitoring during CPR may be use-ful, but there has yet to be a clinical trial demonstrating that goal-directed CPR based on physiologic parametersimproves outcomes.• Recommendations for ultrasound use during cardiac arrest are largely unchanged, except for the explicit pro-viso that the use of ultrasound should not interfere with provision of high-quality CPR and conventional ACLS therapy.• Continuous waveform capnography remained a Class I recommendation for confirming placement of an endo-tracheal tube. Ultrasound was added as an additional method for confirmation of endotracheal tube placement.• The defibrillation strategies addressed by the 2015 ILCOR review resulted in minimal changes in defibrilla-tion recommendations.• The Class of Recommendation for use of standard dose epinephrine (1 mg every 3 to 5 minutes) was unchangedbut reinforced by a single new prospective randomized clinical trial demonstrating improved ROSC and survivalto hospital admission that was inadequately powered to measure impact on long-term outcomes.• Vasopressin was removed from the ACLS Cardiac ArrestAlgorithm as a vasopressor therapy in recognition of equivalence of effect with other available interventions (eg, epinephrine). This modification valued the simplic-ity of approach toward cardiac arrest when 2 therapies were found to be equivalent.• The recommendations for timing of epinephrine admin-istration were updated and stratified based on the initial presenting rhythm, recognizing the potential difference inpathophysiologic disease. For those with a nonshockablerhythm, it may be reasonable to administer epinephrine as soon as feasible. For those with a shockable rhythm, there is insufficient evidence to make a recommendation。
2015年AHA心肺复苏指南更新

美国心脏学会(AHA)15日在网站上公布了2015版心肺复苏指南,【指南中英文及专家解读专题请点此】以下为该指南的10大更新要点:1、首次规定按压深度的上限:在胸外按压时,按压深度至少5厘米,但应避免超过6厘米。
旧指南仅仅规定了按压深度不低于5厘米。
新指南认为,按压深度不应超过6厘米,超过此深度可能会出现并发症,但指南也指出,大多数胸外按压不是过深,而是过浅。
对于儿童(包括婴儿[小于一岁]至青春期开始的儿童),按压深度胸部前后径的三分之一,大约相当于婴儿4厘米,儿童5厘米。
对于青少年即应采用成人的按压深度,即5~6厘米。
2、按压频率规定为100~120次/分。
原指南仅仅规定了每分钟按压频率不少于100次/分,但一项大样本的注册研究发现,如果按压频率(超过140次/分)过快,按压幅度则不足。
指南也指出,在心肺复苏过程中,施救者应该以适当的速率(100至120次/分)和深度进行有效按压,同时尽可能减少胸部按压中断的次数和持续时间。
新指南规定,胸部按压在整个心肺复苏中的目标比例为至少60%。
指南把心肺复苏与驾车行驶进行了比较。
在驾车行驶时,一天行驶的里程数不仅受行驶速度影响,还受中途停顿的次数和时间影响。
以60英里/小时的速度不中断行驶,则实际行驶距离为一小时60英里。
以60英里每小时的速度行驶,但中途停顿10分钟,则实际行驶距离为―小时的英里。
停顿越频繁,停顿时间越长,则实际行驶里程越少。
3、为保证每次按压后使胸廓充分回弹,施救者在按压间隙,双手应离开患者胸壁。
原指南仅建议,每次按压后,施救者应让胸廓完全回弹,以使心脏在下次按压前完全充盈。
如果在两次按压之间,施救者依靠在患者胸壁上,会妨碍患者的胸壁会弹。
4、无论是否因心脏病所导致的心脏骤停,医护人员都应提供胸外按压和通气。
旧版指南仅指出,急救人员和院内专业救援人员都可为心骤停患者实施胸外按压和人工呼吸。
5、关于先除颤,还是先胸外按压的问题,新指南建议,当可以立即取得体外自动除颤器(AED)时,应尽快使用除颤器。
2015年版心肺复苏

不能“拼命”按压!
2010年的指南一个比较重大的改动就是按压程度,规定了 胸外按压的速度,频率≥100次/分,深度≥5厘米。但这样 就会出现按压过度的问题。这样造成的后果是:患者因为 按压受到伤害(比如胸骨和肋骨的)按压人员会因为长时 间的按压而消耗大量体力,不能保证后续有效的按压(按 压幅度不足与按压频率过快的关)。笔者曾经历过长达50 分钟的CPR,患者的胸骨不仅断了,笔者的体力也消耗殆尽。 患者也当然没救活。今年指南最大的改动就是设定了胸外 按压程度的上限,频率在100~120次/分,深度在5~6厘米。
体征评估从“3步”变成了“2步 ”
相对于2010年的指南“在评估患者意 识之后再分别评估患者呼吸、脉搏” 这样的按部就班,2015年的指南倾向 于评估患者意识后同时评估呼吸和脉 搏,之后再启动应急反应系统(ERS) 或求助。这样有效、同时地评估可减 少ERS的延迟。
心肺复苏程序变化 :C-A-B代替A-B-C
BLS
按压部位:
胸骨下1/2 双侧肋弓的汇合点, 向上两横指
BLS
按压两手手指跷起(扣在一起)离开胸 壁
BLS
按压姿势: 按压时上半身前倾, 腕、肘、肩关节伸直, 以髋关节为轴, 垂直向下用力, 借助上半身的体重 和肩臂部肌肉的 力量进行按压
BLS
按压部位: 以掌跟按压
婴幼儿胸外心脏按压方法
体外技术和有创灌注装置
对于发生心脏骤停,且怀疑心脏骤 停的病因可能可逆的选定患者,可 以考虑以体外心肺复苏(ECPR)替 代传统心肺复苏。
2015新版心肺复苏指南

2015新版心肺复苏指南:儿童基础及高级生命支持要点015年10月15日,美国心脏协会(AHA)公布了最新版的心肺复苏指南。
上周,小编已经对新版指南中“成人基础生命支持和心肺复苏质量(医护人员BLS)”部分与2010版进行了对比,而本文将对此次指南中儿科基础及高级生命支持部分的要点进行总结。
首先是2015 AHA心肺复苏指南儿科基础生命支持心肺复苏(CPR)部分要点:1.院外心脏骤停儿童患者的存活情况不容乐观,各年龄组存活率约为8%。
2.由于窒息性心脏骤停在儿童中更为常见,因此通气设备对儿童患者至关重要。
但儿童心肺复苏中胸部按压、开放气道及人工呼吸顺序与成人治疗内容一致。
3.高质量心肺复苏(CPR)包括:充分的胸部按压频率(100~120 bpm)及深度(胸廓前后径1/3);尽可能减少胸外按压的中断次数;避免过度通气(可见胸廓充分回弹,12~20次/分钟);4.胸部按压/人工呼吸效果优于单纯按压,若施救者不愿进行人工呼吸,也可单纯进行胸部按压。
2015AHA心肺复苏指南儿科高级生命支持的内容要点:1.儿科院内心脏骤停存活率已增加至43%左右。
2.延长CPR并非毫无作用,接受CPR治疗35分钟以上者的存活率达12%,60%患者的神经预后有所改善。
3.心脏骤停前治疗儿科快速反应治疗团队及儿科预警评分可降低非ICU患者及普通患者的死亡率,但研究结论并不一致,这些方案可用于普通病房的高危儿童患者;对于感染性休克患者,可进行输液推注治疗(剂量可达20cc/kg),但后续推治疗注应视个体评估情况而定;存在心脏骤停风险的急性爆发性心膜炎患者可考虑静脉-动脉体外膜肺氧合(ECMO)治疗。
4.骤停期间治疗ECMO心肺复苏(ECPR)可用于心外科诊断异常的患者,此类患者经ECPR治疗后的预后优于其他患者;应用呼气末CO2及介入性血流动力学监测以评估CPR治疗质量,但目前尚无具体参考值;除颤能量:2 J/kg,4 J/kg,>4 J/kg,最大能量10 J/kg或成人剂量;对于电击难治性室颤或无脉室速的患者,考虑胺碘酮或利多卡因治疗。
2015年AHA国际心肺复苏指南详解
对于急性 ST 段升高型心肌梗死( STEMI )的患者,新版 的指南更加推荐 PCI,因其可以减少颅内出血的发生。即 使在不能 PCI 的医院中对 STEMI 患者进行溶栓治疗,患 者也应在溶栓后的最初 3 到 6 h,最多 24 h 内进行常规血 管造影,以防再梗死的发生。
对于 STEMI 患者,入院前可给予普通肝素(UFH)或比 伐卢定;对于正在向 PCI 中心转移的 STEMI 疑似患者, 可以用依诺肝素代替普通肝素。
阿托品
阿托品在指南更新中出现于儿童高级生命支持的部分,新 版指南纠正了旧版关于气管插管术前,给予阿托品存在最 小剂量预防心动过缓的说法。
知识延伸
阿托品用法:麻醉前单次 0.01-0.03 mg/kg,最大剂量 0.6 mg。
纳洛酮
新版指南指出,对于已知或疑似阿片类药物成瘾的患者, 救治同时可以给予患者肌内注射或鼻内给予纳洛酮。同时 给出了纳洛酮的用法,即纳洛酮 2 mg 滴鼻或 0.4 mg 肌注。 并可根据患者反应情况,在 4 分钟后重复给药。
知识延伸
利多卡因用法:起始剂量 1-1.5 mg/kg 静推(一般用 50100 mg),静脉注射 2-3 min。根据患者反应,5-10 min 后可再用 0.5-0.75 mg/kg 静推,1 h 内最大剂量不得超过 300 mg。利多卡因易引起除颤后心脏停搏,使用时应予以 注意。
溶栓治疗
非专业人士该怎么做
1. 继续强调简化后的通用成人基础生命支持(BLS)流程;
2. 施救者在不离开患者的情况下紧急反应(通过手机等电子设备), 未经培训的旁观者应该立即拨打急救电话(中国为 120);
2015年国际心肺复苏指南

四、利用社会媒体呼叫施救者
• 2015 (更新):
对社区来说,利用社会媒体技术,帮助在院外疑似发生心脏骤停的患者呼 叫附近有愿意帮助并有能力实施心肺复苏的施救者是有一定合理性的。
• 理由 :
有限的证据显示调度员利用社会媒体在可能发生心脏骤停的患者附近呼叫 的施救者,但没有证据表明启动社会媒体可以提高院外心脏骤停的存活率。但 是,瑞典最近的一项研究发现,使用手机调度系统时,旁观者启动心肺复苏的 比率显著上升。考虑到这种情况危害较低而有潜在益处,同时电子设备也无处 不在,市政机构可以考虑将这些技术融入到院外心脏骤停救治系统中。
2015(更新):
确定了救治体系 的通用元素,为利益 相关方提供了一个通 用框架,以便其组建 一个综合性复苏系统 (图3)
理由 : 提供医疗服务需要架构(如人员、器材、教育等)与流程(如政策、协议、
程序等),把它们综合起来,就能形成一个系统(如方案、组织、文化等),产生 最佳结果(如患者的存活、安全、质量、满意等)。一套有效的救治体系,能在一 个质量持续改进的框架中融入所有这些元素——架构、流程、系统和患者预后。
最新发布| 2015AHA心肺复苏和心血管急救指南更新
AHA呼吁,迅速采取行动,团队合作实施CPR;指南还强调了 公众的作用。
对于非专业施救者,指南强调识别心脏骤停征象、及时打急 救电话并立即开始徒手CPR(心脏按压频率为100~120次/分)。
对于急救医护人员,指南强调了给予高质量CPR的重要性:以 足够的速率和深度(5~6cm)按压胸部,允许每次按压后胸廓充 分回弹,按压间隙双手应离开患者胸壁,尽可能减少按压中断, 避免过度通气。
• 2010 (旧):
尽管证据存在矛盾,专家共识建议系统性识别有心脏骤停风险的患者, 为这类患者建立有条理的反应系统,并评估患者预后以持续加强质量改进。
2015年AHA国际心肺复苏指南详解
7. 高质量的心肺复苏,足够的速率和按压幅度:按压速率 为 100 - 120 次 / 分钟;幅度至少是 2 英寸(5 厘米)。 不超过 2.4 英寸(6 厘米);
8. 患者有疑似生命危险,或与阿片类药物相关的紧急情况, 应给与纳洛酮:在相关人员指导进行纳洛酮治疗。
美国每年有 20 万例院内心脏骤停发生。CPR 培训是基础 必会的课程。然而,研究显示,这一技能会在接受培训后 数月内逐渐生疏。所以应进行反复、高频的培训来保证院 内持续掌握,并熟悉如何将患者转运到最高质量的心血管 急救部门。
专业人员该怎么做
BLS 中成人高质量心肺复苏的注意事项
BLS 人员进行高质量 CPR 的要点总结
1. 基本原则:施救者应同时进行几个步骤,如同时检查呼 吸和脉搏,以缩短开始首次按压的时间; 由多名施救者形成综合小组,同时完成多个步骤和评估 (分别由施救者实施急救反应系统;胸外按压、进行通气 或取得球囊面罩进行人工呼吸、取回并设置好除颤器同时 进行);
非专业人士该怎么做
1. 继续强调简化后的通用成人基础生命支持(BLS)流程;
2. 施救者在不离开患者的情况下紧急反应(通过手机等电子设备), 未经培训的旁观者应该立即拨打急救电话(中国为 120);
3. 建议在有心脏骤停风险人群社区执行公共场所除颤器(PAD)方案, 可在社区、健身房、运动场等场所配备除颤器; 4. 鼓励非专业人士进行心肺复苏:快速识别心脏骤停,立即向呼叫者 提供心肺复苏指导(调度员指导下的心肺复苏); 5. 单一施救者的施救顺序:应先开始胸外按压再进行人工呼吸(C - A - B),减少首次按压的延时; 非专业人员在指导下自行对心脏骤停的成人患者进行单纯胸外按压 (Hands - Only)式心肺复苏,指导自动体外除颤仪或有参加过训练 的施救者胸外按压;不必进行口对口人工呼吸,仅在胸部中心进行快 速有力的按压,频率为 100-120 次 / 分钟。若有能力,则应按照 30 次按压给与 2 次人工呼吸的比例给予人工呼吸。
2015年美国心肺复苏指南
R:判断评估意识反应
• • • • 1. 拍打双肩双耳呼叫(判断有无反应); 2. 看意识胸廓有无起伏; 3. 无意识无呼吸立即拨打120; 4. 急救医生没有到达之前摆放患者为仰卧 位。 • 总结:一看、二唤、三呼、四摆。 • 由第一目击者实施。
A:启动急救系统
• 立即启动呼叫急救系统,取得帮助和除颤 仪 • 若AED(自动除颤仪)在附近,立即叫人或 自己去取 • 呼叫后,尽快开始CAB的心肺复苏除颤。
心肺复苏成功
• 颈动脉及自主呼吸恢复,复苏抢救成功,继续下一步生命支持,心肺复苏操 作完毕。为患者摆好体位。
心肺复苏有效表现 面色、口唇有苍白、青紫变为红润。 恢复可以探明脉搏搏动、自主呼吸 瞳孔由大变小、对光反射恢复,伤 病员眼球能活动,手脚抽动,呻吟。
成人基础CPR ——2015更新要点
1、生存链一分为二
A:开放气道
• 清除口腔、气道异物,如呕吐物、假牙等 • 用一只手的掌外侧按住伤病员的前额,另一只手 • 提起伤病员的下颏,保持其呼吸道畅通(仰头提 颏法) • 有头部外伤的,医务人员推荐用(推举下颌 法)
B:人工呼吸
人工呼吸两次
• 捏紧患者的鼻翼,吸一口气(500-600ml) 口对口包严患者口唇周围持续将气体吹入 (大约1秒钟),观察胸廓隆起。 • 连续做两次口对口人工呼吸(5秒2次) • 未见明显的胸廓隆起时,重新开放气道, 再做一次人工呼吸。
且侥幸存活者可能已“脑死亡” 心搏骤停10分钟实施CPR成功率几乎为0
白金 时间1分钟内,
黄金时间4分钟, 白银时间4-8分钟, 白布单时间8-10分钟后
心肺复苏(CPR)
• 心肺复苏(CPR),是针对骤停的心脏和呼吸采取的“救 命技术。 • 心脏骤停发生后,全身重要器官将发生缺血缺氧。特别是 脑血流的突然中断,在10秒左右患者即可出现意识丧失, 4~6分钟时脑循环持续缺氧开始引起脑组织的损伤,而超 过10分钟时将发生不可逆的脑损害。 • 心肺复苏的黄金时间为“4~6分钟” • 心肺复苏的3个关键步骤(CAB) • C胸外按压 A开放气道 B人工呼吸
2015 心肺复苏指南 7 大更新要点总结

2015 心肺复苏指南7 大更新要点总结(附中文版下载)2015-10-16 15:07来源:丁香园作者:王妍字体大小-|+2015 年10 月15 日,新版《美国心脏学会CPR 和ECC 指南》隆重登场。
时隔5 年,AHA 会对指南的哪些部分进行更改?是否提出了颠覆性的观点?接下去,丁香园将为你用心分析。
1. 快速反应,团队协作施救者应同时进行几个步骤,如同时检查呼吸和脉搏,以缩短开始首次按压的时间;由多名施救者形成综合小组,同时完成多个步骤和评估(分别由施救者实施急救反应系统;胸外按压、进行通气或取得球囊面罩进行人工呼吸、取回病设置好除颤器同时进行)。
2. 生存链「一分为二」AHA 成人生存链分为两链:一链为院内急救体系,另一链为院外急救体系。
手机时代,充分利用社会媒体呼叫施救者,手机等现代化电子设备能够在院外急救中发挥重要作用;院内急救应以团队形式实施心肺复苏:早期预警系统、快速反应小组(RRT)和紧急医疗团队系统(MET)。
3. 先电击or 先按压10 年的指南中,在AED 就绪时,应先进行1.5 - 3 分钟的CPR, 然后再除颤。
最新版则提出:当施救者可以立即取得AED 时,对于成人心脏骤停患者,应尽快使用除颤器;若不能立刻取得AED,应该在他人前往获取以及转变AED 的时候开始心肺复苏,在设备提供后尽快尝试进行除颤。
4. 别再使劲按了!10 年的指南规定胸外按压的下限:频率≥ 100 次/ 分、深度≥ 5 厘米。
临床上普遍存在按压过度的问题,如胸骨和肋骨骨折,同时,施救者也会消耗大量体力,无法保证接下去的按压质量。
新的指南提出高质量的心肺复苏,应该有足够的速率和按压幅度:按压速率为100 - 120 次/ 分钟;幅度至少是5 厘米,不超过6 厘米。
5. 瘾君子的福音若患者有疑似生命危险、或与阿片类药物相关的紧急情况,应给与纳洛酮。
瘾君子的福音!对于已知或疑似阿片类药物成瘾的患者,如果无反应且呼吸正常,但有脉搏,可由经过正规培训的非专业施救者和BLS 施救者给与肌肉注射或鼻内给予纳洛酮。
2015版心肺复苏术_2015版美国心肺复苏指南-2016.5.26

❤心脏骤停后救治
• 1)对于所有ST段抬高的患者,以及无ST段抬高,但血流 动力学或心电不稳定,疑似心血管病变的患者,建议紧急 冠状动脉皿管造影 • 2)有关目标温度管理的建议有所更新。新的证据表明, 一定范围内的温度都可作为心脏骤停后一定时间段内的目 标温度 • 3)TTM(目标温度管理)结束后,可能会出现发热症状 尽管有关TTM结束后发热危害的观察性证据存在矛盾,但 仍然认为预防发热是有益的,因此应该预防 • 4)在复苏后,建议立即确认并矫正低血压症状 • 5)现在建议必须在TTM结束72小时后才能做预后评估: 对于未采用TTM的患者,应当在恢复自主循环72小时后做 预后评估 • 6)所有初次心脏骤停后发展为脑死亡或循环死亡的患者 都应视为可能的器官
急救系统和持续质量改进
生存链分为两链
成人基础生命支持和心肺复苏质量 (非专业施救者心肺复苏)
• (1)院外成人生存链的关键环节和2010年相同,继续强 调简化后的通用成人基础生命支持(BLS)流程
• (2)成人基础生命支持流程有所改变,反映了施救者可 以在不离开患者身边的情况下启动紧急反应(即通过手机 )的现实情况 • (3)建议在有心脏骤停风险人群的社区执行公共场所除 颤(PAD)方案 • (4)鼓励迅速识别无反应情况,启动紧急反应系统,及 鼓励非专业施救者在发现患者没有反应且没有呼吸或呼吸 不正常(如喘息)时开始心肺复苏的建议得到强化
8、人工呼吸的常见错误
(1)时间过长,气量过大:过多气体会在压
力促使下流入胃内,使胃胀气。这时,会见
到上腹部只起不伏,这是有危险的。胃内气
体过多,能将肺压缩,还容易使胃内食物倒
流入嘴,引起窒息! (2)时间过短,气量不足。 (3)没有打开气道直接吹气
2015 心肺复苏指南
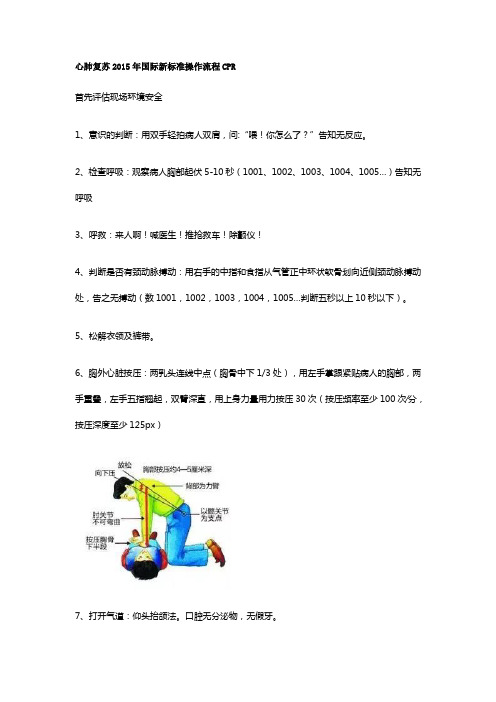
心肺复苏2015年国际新标准操作流程CPR首先评估现场环境安全1、意识的判断:用双手轻拍病人双肩,问:“喂!你怎么了?”告知无反应。
2、检查呼吸:观察病人胸部起伏5-10秒(1001、1002、1003、1004、1005…)告知无呼吸3、呼救:来人啊!喊医生!推抢救车!除颤仪!4、判断是否有颈动脉搏动:用右手的中指和食指从气管正中环状软骨划向近侧颈动脉搏动处,告之无搏动(数1001,1002,1003,1004,1005…判断五秒以上10秒以下)。
5、松解衣领及裤带。
6、胸外心脏按压:两乳头连线中点(胸骨中下1/3处),用左手掌跟紧贴病人的胸部,两手重叠,左手五指翘起,双臂深直,用上身力量用力按压30次(按压频率至少100次∕分,按压深度至少125px)7、打开气道:仰头抬颌法。
口腔无分泌物,无假牙。
8、人工呼吸:应用简易呼吸器,一手以“CE”手法固定,一手挤压简易呼吸器,每次送气400-600ml,频率10-12次/分。
9、持续2分钟的高效率的CPR:以心脏按压:人工呼吸=30:2的比例进行,操作5个周期。
(心脏按压开始送气结束)10、判断复苏是否有效(听是否有呼吸音,同时触摸是否有颈动脉博动)。
11、整理病人,进一步生命支持。
提高抢救成功率的主要因素:1、将重点继续放在高质量的CPR上2、按压频率至少100次/分(区别于大约100次/分)3、胸骨下陷深度至少5 ㎝4、按压后保证胸骨完全回弹5、胸外按压时最大限度地减少中断6、避免过度通气心肺复苏= (清理呼吸道) + 人工呼吸+ 胸外按压+ 后续的专业用药据美国近年统计,每年心血管病人死亡数达百万人,约占总死亡病因1/2。
而因心脏停搏突然死亡者60-70%发生在院前。
因此,美国成年人中约有85%的人有兴趣参加CPR初步训练,结果使40%心脏骤停者复苏成功,每年抢救了约20万人的生命。
心脏跳动停止者,如在4分钟内实施初步的CPR,在8分钟内由专业人员进一步心脏救生,死而复生的可能性最大,因此时间就是生命,速度是关键,初步的CPR按ABC进行。
2015年最新心肺复苏指南
胸外按压速率:100 至 120 次/ 分 钟
2015( 更新): 对于心脏骤停的成年患者,施救者以理。
2010( 旧): 非专业施救者和医务人员以每分钟至少 100 次的按压速率进行胸外按压较为合理。
理由:建议最低的按压频率仍是 100 次/ 分钟。设定120 次每分钟的速率上限,是因为有一项大型的注册系列研究 表明,当按压速率超过 120 次每分钟时,按压深度会由于 剂量依存的原理而减少。例如,当按压速率在100 到119 次每分钟时,按压深度不足的情况约占 35%,而当按压速 率提高到 120 到 139 次每分钟时,按压深度不足的情况占 到 50%,当按压速率超过 140 次每分钟时,按压深度不 足的比例达到 70%。
在心肺复苏中使用高级气道进行通气
2015( 更新): 医护人员可以每 6 秒进行 1 次人 工呼吸(每分钟 10 次),同时进行持续胸部按压 (即在心肺复苏中使用高级气道)。
2010( 旧): 双人复苏时建立了高级气道(例如 气管插管、食管气管导管、喉罩气道 [LMA])后 ,应每6-8 秒给予1 次呼吸,不用保持呼吸按压同 步(这样,人工呼吸频率为每分钟 8 到 10 次)。
先给予电击还是先进行心肺复苏 ?
2015( 更新): 当可以立即取得 AED 时, 对于有目击的成人心脏骤停,应尽快使用 除颤器。若成人在未受监控的情况下发生 心脏骤停,或不能立即取得 AED 时,应该 在他人前往获取以及准备 AED 的时候开始 心肺复苏,而且视患者情况,应在设备可 供使用后尽快尝试进行除颤。
能取得较好结果。尽管有关按压深度是否有上限的证据较 少,但最近一项很小的研究表明,胸部按压深度过深(大 于 2.4 英寸 [6 厘米])会造成损伤(不危及生命)。如不 使用反馈装置,可能难以判断按压深度,并很难确认按压 深度上限。施救者必须认识到,胸部按压深度往往过浅而 不是过深。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
2015 AMERICAN HEART ASSOCIATION摘要心肺复苏及心血管急救指南更新目录简介 (1)伦理学问题 (2)急救系统和持续质量改进 (3)成人基础生命支持和心肺复苏质量:非专业施救者心肺复苏 (5)成人基础生命支持和心肺复苏质量:医护人员BLS (7)心肺复苏的替代技术和辅助装置 (11)成人高级心血管生命支持 (13)心脏骤停后救治 (14)急性冠脉综合征 (16)特殊复苏环境 (18)儿科基础生命支持和心肺复苏质量 (20)儿童高级生命支持 (23)新生儿复苏 (25)培训 (27)急救 (29)参考文献 (32)致谢The American Heart Association thanks the following people for their contributions to the development of this publication: Mary Fran Hazinski, RN, MSN; Michael Shuster, MD; Michael W. Donnino, MD; Andrew H. Travers, MD, MSc; Ricardo A. Samson, MD; Steven M. Schexnayder, MD; Elizabeth H. Sinz, MD; Jeff A. Woodin, NREMT-P; Dianne L. Atkins, MD; Farhan Bhanji, MD; Steven C. Brooks, MHSc, MD; Clifton W. Callaway, MD, PhD; Allan R. de Caen, MD; Monica E. Kleinman, MD; Steven L. Kronick, MD, MS; Eric J. Lavonas, MD; Mark S. Link, MD; Mary E. Mancini, RN, PhD; Laurie J. Morrison, MD, MSc; Robert W. Neumar, MD, PhD; Robert E. O’Connor, MD, MPH; Eunice M. Singletary, MD; Myra H. Wyckoff, MD; 和AHA《指南摘要》项目组。
简体中文版:Neil Huerbin, MD 和AHA Guidelines Highlights International Project Team版权所有© 2015 American Heart Association《2015 AHA 心肺复苏及心血管急救指南更新》摘要 1 简介本《指南摘要》总结了 2015 American Heart Association (AHA) 心肺复苏 (CPR) 及心血管急救 (ECC) 指南更新中的 关键问题和内容变更。
本刊物针对急救人员和 AHA 导师, 旨在帮助他们关注最重要、最有争议性,或会给复苏操作 与复苏培训带来变更的复苏科学和指南建议。
并给出了建 议的依据。
由于本刊物仅作为总结,因此未参考可提供支持的已发 表研究,也未列出建议级别或证据水平。
欲了解更多详 细信息和参考资料,请读者阅读《2015 AHA 心肺复苏及 心血管急救指南更新》,包括发表于《循环》杂志 2015 年 10 月刊的“执行摘要”1,对于复苏学详细总结性信息的相 关咨询,请参阅同时发表于《循环》2 和《复苏》3杂志中 2015 心肺复苏和心血管急救科学及治疗建议的国际共识。
《2015 AHA 心肺复苏及心血管急救指南更新》 是基于国 际证据评估流程,由来自 39 个国家的 250 位证据审查专家共同参与完成。
2015 版国际复苏联络委员会 (ILCOR) 采用的系统性审查流程与 2010 版所用流程有很大不同。
在 2015 版的系统性审查流程中,ILCOR 的人员优先选 择那些具备充分科学研究的或富有争议的主题进行审查。
由于这种优先机制,2015 年完成的审查(166 份)较 2010 年(274 份)要少。
在主题选定以后,2015 年的审查流程本身也增加了两项重要内容。
首先,审查专家采用建议分级评估、开发、评 价的分级系 统(GRADE; ), 这是一个高度结构化和可重复性的证据审查系统,使 2015 版的系统性审查更加一致且质量更高。
其次,来自世界各地的审查专家可以通过系统的证据评估和审查系统 (SEERS) 进行网上协作。
这个系统 (SEERS) 是专门 图 1新 AHA 建议级别和证据水平分级体系 *COR 与 LOE 是独立确定的(COR 和 LOE 可随意匹配)。
如果某建议的证据等级为 LOE C ,并不代表其为弱建议。
本指南中提到的许多重要临床问题缺乏临床试验支持。
尽管没有 RCT ,但可能存在非 常明确的临床共识,认为某一特定检查或治疗是有用的或有效的。
* 干预措施的结果或效果应该具体明确(临床效果改善或诊断精度提高 或预后信息增加)。
† 对于相对有效性建议(COR I 和 2a ;仅 LOE A 和 B ),支持使用比较动 词的研究应该对所评估的几项治疗或策略进行了直接比较。
‡ 评价质量的方法在发生演变,包括对标准化的、广泛使用的、经过验 证的证据评级工具的运用 ;以及在系统性审查中,有了证据审查委员 会的参与。
COR 指建议级别 ;EO ,专家意见 ;LD ,有限数据 ;LOE ,证据水平; NR ,非随机 ;R ,随机 ;RCT ,随机对照试验。
《2015 AHA 心肺复苏及心血管急救指南更新》摘要1建议级别(强度)1 级(强)益处 >>> 风险撰写指南建议时推荐采用的表述 :◾ 是推荐的 ◾ 是有效的 / 有用的 / 有效的 / 有益的 ◾ 应实施 / 执行 / 其他 ◾ 相对有效性的表述 † : • 推荐 / 需要使用治疗方案 / 策略 A 而不是治疗方案 B • 优先选择治疗方案 A 而非治疗方案 B2a 级(中)益处 >> 风险撰写指南建议时推荐采用的表述 :◾ 是合理的◾ 可能是有用的 / 有效的 / 有益的 ◾ 相对有效性的表述 † : • 可能推荐 / 需要使用治疗方案 / 策略 A 而不是 治疗方案 B• 优先选择治疗方案 A 而不是治疗方案 B 是合理的2b 级(弱)益处 ≥ 风险撰写指南建议时推荐采用的表述 :◾ 可能 / 或许是合理的◾ 可能 / 或许可以考虑使用的 ◾ 有用性 / 有效性尚未知 / 不明确 / 不确定或未获公认3 级 :无益(中) 益处 = 风险(通常只用于 LOE A 或 B )撰写指南建议时推荐采用的表述 : ◾ 不建议 ◾ 是无效的 / 无用的 / 无效的 / 无益的 ◾ 不应实施 / 执行 / 其他3 级 :有害(强)风险 > 益处撰写指南建议时推荐采用的表述 : ◾ 可能有害 ◾ 导致危害◾ 与发病率 / 死亡率增加相关 ◾ 不应实施 / 执行 / 其他证据水平(质量)‡ A 级◾ 来自一项以上的 RCT 的高质量证据 ‡ ◾ 高质量 RCT 的元分析◾ 一项或以上由高质量注册研究证实的 RCTB-R 级(随机)◾ 来自一项或以上的 RCT 的中等质量证据 ‡◾ 中等质量 RCT 的元分析B-NR 级 (非随机)◾ 来自一项或以上设计良好、执行良好的非随机研 究、观察性研究或注册研究的中等质量证据 ‡ ◾ 这类研究的元分析C-LD 级 (有限数据)◾ 设计或执行有局限的随机或非随机观察性或注册研究◾ 这类研究的元分析◾ 对人类受试者的生理或机理研究C-EO 级(专家意见)基于临床经验的专家共识为AHA 建立的网络平台,旨在为评估流程中的多个步骤提供支持。
SEERS 网站是用于公开发布ILCOR 编写的2015 心肺复苏和心血管急救科学及治疗建议的国际共识的各版样稿,以供公众评论。
欲了解更多有关SEERS 的信息并查看ILCOR 所有系统性审查的详细列表,请访问/seers。
《2015 AHA 心肺复苏及心血管急救指南更新》与之前各版《AHA 心肺复苏及心血管急救指南》有很多不同。
心血管急救委员会决定,2015 年版是一份“更新”,仅讨论2015 ILCOR 证据审查中涉及的或培训网络所要求的主题。
这确保了我们在证据评估时只有一个标准,即ILCOR 创立的评估流程。
因此,《2015 AHA 心肺复苏及心血管急救指南更新》并非《2010 AHA 心肺复苏及心血管急救指南》的全面修订。
全面修订的集成版本可从 获取。
2015 心肺复苏和心血管急救科学及治疗建议的国际共识的出版为复苏学开启了一个持续的审查过程。
2015 版所审查的主题还会根据需要不断更新,而新的主题也会不断加入。
敬请读者关注SEERS 网站,了解复苏科学的最新资讯及ILCOR 的相关评估。
当有足够的新证据表明《AHA 心肺复苏及心血管急救指南》需要变更时,我们会进行相关变更,并传达给临床医生及培训网络。
2015《指南更新》中使用的建议级别和证据水平,均依据AHA 的最新定义(图1)。
读者将注意到,最新版定义中的 3 级建议有所更改,3 级:无益,当证据显示,有高质量或中等质量研究(证据水平LOE 分别为 A 或B)表明某项策略的效果并不优于对照组时,不常使用。
证据水平也有所更改。
LOE B 现分为LOE B-R(随机研究)和LOE B-NR(非随机研究)。
LOE C 现分为LOE C-LD (有限数据)和C-EO(专家意见)。
正如新近发表的美国医学研究所报告 4 及AHA 心血管急救共识对该项报告的回应5 所指出的,我们还需更加努力,推动复苏科学研究及复苏操作。
过去20 年间,医疗同仁协力支持推动了癌症和中风的相关研究。
同样,我们也需要共同努力,支持心脏骤停复苏的相关研究。
在对2015《指南更新》中的建议进行审查时(图2),这种研究上的不足体现得非常明显。
总的来说,复苏学的证据水平和建议级别都较低,2015 版的所有建议中仅1%(315 条建议中有 3 条)基于最高证据水平(LOE A),仅25% 的建议(315 条建议中有78 条)被认定为 1 级(强建议)。
2015《指南更新》中的大部分建议(69%) 都只有最低证据水平的支持(LOE C-LD 或C-EO),将近一半(315 条建议中有144 条,45%)被定为2b 级(弱建议)。
在整个ILCOR 证据评估流程和2015《指南更新》编写过程中,参与人员均严格遵照AHA 有关利益冲突的申报要求。
AHA 的工作人员审理了1000 多份利益冲突申报表,所有的《指南》编写组主席和至少50% 的编写组成员都被要求不能涉及任何相关利益冲突。
