fenton2013growthchartcolorgirls早产儿生长曲线图女孩.pdf
医师教你看懂生长曲线图
医师教你看懂生长曲线图医师教你看懂生长曲线图宝宝的生长曲线图,应该怎么看?为什么宝宝体重增加的速度会突然变慢?生长曲线图的百分位落在50%最好吗?数值比较低的宝宝,需不需要努力迎头赶上?本文请医师教爸妈简单看懂生长曲线图,并回答相关的常见疑问。
生长曲线图有新旧版本的差别?蔡立仪医师表示,卫生福利部国民健康署所发给家长的儿童健康手册,关于生长曲线的部分以前只有0~5岁,102年以后改版,将年龄延伸至0~7岁,追踪到学龄前的发展。
0~5岁的生长曲线图,是采用世界卫生组织跨国合作所制定的标准图,调查喂食母乳并适时添加副食品、并且在良好环境成长的宝宝的生长情形;至于新增的5~7岁生长曲线图,则是根据国内学者陈伟德教授研究的结果所制定,再衔接到原有0~5岁的生长曲线上。
生长曲线图多久要看一次?配合预防针接种的时程,医师会在健儿门诊时,一并替宝宝确认儿童健康手册上的生长曲线图发展是否正常;平常在家里时,爸妈也可以替宝宝测量头围、身高、体重,并登记在生长曲线图上。
头围用皮尺测量即可(头围要测量头部最宽处),身高则可使用身高尺,体重可使用电子磅秤(当宝宝会站以后,就可以使用一般大人的体重计)。
如果家里没有这些物品,可以等健儿门诊时再测量,随着接种疫苗的时程,医院在每次健儿门诊追踪时都会测量。
怎么看生长曲线图?蔡立仪医师说明,当测量好身高、体重与头围后,先从横轴标定年龄,再从纵轴选测量后所得到的数值,在两条线的交会处画下一个点做记号。
不过要注意,生长曲线为连续性的纪录,不能只以一次的测量结果就断定宝宝的生长发展走势。
一般来说,宝宝通常会沿着自己的生长曲线走。
假如上一次与下一次的测量结果改变的幅度超过两个曲线区间(例如从85%掉到15%),可能是异常的警讯,必须特别留意与追踪。
百分位所代表的意义?生长曲线图上所显示的百分位,如果是50%,表示在100个同年龄的宝宝中,大约平均为第50名,属于中间值(这个数值是根据先前的研究结果所统计出来的)。
中国儿童生长曲线
中国儿童生长曲线
中国儿童生长曲线是根据中国儿童普查数据绘制的图表,用来反
映中国儿童的身高、体重和头围随年龄的变化规律。
根据曲线,我们
可以了解儿童生长发育的情况,判断是否正常生长。
中国儿童生长曲线分为男女两种,每种曲线都分为身高、体重和
头围三个指标。
在曲线上,横坐标表示年龄,纵坐标表示相应的身高、体重或头围数值。
根据年龄的增加,曲线会逐渐上升,并且曲线会逐
渐平缓,说明儿童生长速度逐渐减慢。
根据中国儿童生长曲线,我们可以评估儿童的生长发育情况是否
正常。
如果曲线上的点位于正常曲线范围内,表明儿童的生长发育与
同龄儿童相符合;如果点位于曲线上方,说明儿童生长发育较好;而
如果点位于曲线下方,可能意味着儿童生长发育不够理想。
儿童生长曲线是临床医生、营养师和家长判断儿童生长发育是否
正常的重要参考依据之一。
通过观察儿童的身高、体重和头围等指标
是否与曲线相符,可以及时发现儿童生长发育异常的情况,提供相应
的干预和治疗。
同时,家长也可以通过儿童生长曲线了解儿童的生长
状态,制定合理的营养和保健计划。
总之,中国儿童生长曲线是反映中国儿童生长发育情况的重要工具,对于了解儿童的生长状态、及时发现生长异常具有重要意义。
早产儿生长曲线图
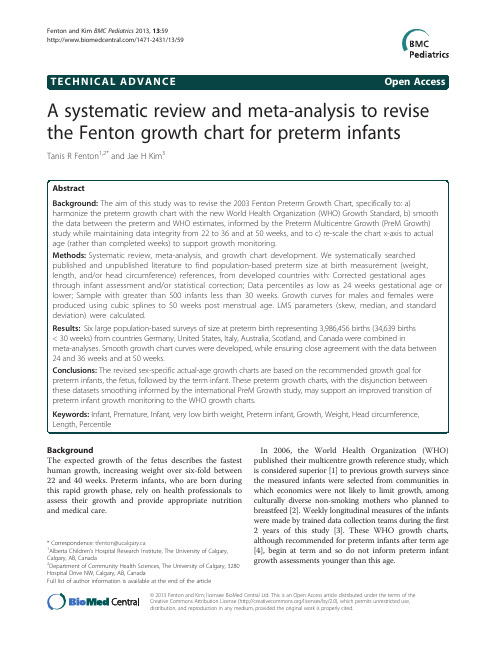
A systematic review and meta-analysis to revise the Fenton growth chart for preterm infantsTanis R Fenton 1,2*and Jae H Kim 3BackgroundThe expected growth of the fetus describes the fastest human growth,increasing weight over six-fold between 22and 40weeks.Preterm infants,who are born during this rapid growth phase,rely on health professionals to assess their growth and provide appropriate nutrition and medical care.In 2006,the World Health Organization (WHO)published their multicentre growth reference study,which is considered superior [1]to previous growth surveys since the measured infants were selected from communities in which economics were not likely to limit growth,among culturally diverse non-smoking mothers who planned to breastfeed [2].Weekly longitudinal measures of the infants were made by trained data collection teams during the first 2years of this study [3].These WHO growth charts,although recommended for preterm infants after term age [4],begin at term and so do not inform preterm infant growth assessments younger than this age.*Correspondence:tfenton@ucalgary.ca 1Alberta Children ’s Hospital Research Institute,The University of Calgary,Calgary,AB,Canada 2Department of Community Health Sciences,The University of Calgary,3280Hospital Drive NW,Calgary,AB,CanadaFull list of author information is available at the end of thearticle©2013Fenton and Kim;licensee BioMed Central Ltd.This is an Open Access article distributed under the terms of the Creative Commons Attribution License (/licenses/by/2.0),which permits unrestricted use,distribution,and reproduction in any medium,provided the original work is properly cited.Fenton and Kim BMC Pediatrics 2013,13:59/1471-2431/13/59Optimum growth of preterm infants is considered to be equivalent to intrauterine rates[5-7]since a superior growth standard has not been defined.Perhaps the best estimate of fetal growth may be obtained from large population-based studies,conducted in developed coun-tries[8],where constraints on fetal growth may be less frequent.A recent multicentre study by our group(the Preterm Multicentre Growth(PreM Growth)Study)revealed that although the pattern of preterm infant growth was gener-ally consistent with intrauterine growth,the biggest devi-ation in weight gain velocity between the preterm infants and the fetus and infant was just before term,between37 and40weeks(Fenton TR,Nasser R,Eliasziw M,Kim JH, Bilan D,Sauve R:Validating the weight gain of preterm in-fants between the reference growth curve of the fetus and the term infant,The Preterm Infant Multicentre Growth Study.Submitted BMC Ped2012).Rather than demon-strating the slowing growth velocity of the term infant during the weeks just before term,the preterm infants had superior,close to linear,growth at this age.This finding has been observed by others as well[9-11].Therefore, there is evidence to support a smooth transition on growth charts between late fetal and early infant ages. Several previous growth charts based on size at birth presented their data as completed age,which affects the interpretation and use of a growth chart[12].The use of completed weeks when plotting a growth chart requires all the measurements to be plotted on the whole week vertical axes.However,the use of completed weeks in a neonatal unit may not be intuitive,as nursery staff and parents think of infants as their exact age,and not age truncated to previous whole weeks.The advent of computers in health care,for clinical care and health recording,allow the use of the computer to plot growth charts,daily and with accuracy.It would make sense to support plotting daily measurements continuously by shifting the data collected as completed weeks to the midpoint of the next week to remove the truncation of the data collection as completed weeks.The objectives of this study were to revise the2003 Fenton Preterm Growth Chart,specifically to:a)use more recent data on size at birth based on an inclusion criteria, b)harmonize the preterm growth chart with the new WHO Growth Standard,c)to smooth the data between the preterm and WHO estimates while maintaining integrity with the data from22to36and at50weeks, d)to derive sex specific growth curves,and to e)re-scale the chart x-axis to actual age rather than completed weeks,to support growth monitoring.MethodsTo revise the growth chart,thorough literature searches were performed to find published and unpublished population-based preterm size at birth(weight,length, and/or head circumference)references.The inclusion criteria,defined a priori,designed to minimize bias by restriction[13],were to locate population-based studies of preterm fetal growth,from developed countries with: a)Corrected gestational ages through fetal ultrasoundand/or infant assessment and/or statisticalcorrection;b)Data percentiles at24weeks gestational age orlower;c)Sample of at least25,000babies,with more than500infants aged less than30weeks;d)Separate data on females and males;e)Data available numerically in published form orfrom authors,f)Data collected within the past25years(1987to2012)to account for any secular trends.A.Data selection and combinationMajor bibliographic databases were searched:MEDLINE (using PubMed)and CINHAL,by both authors back to year1987(given our25year limit),with no language restrictions,and foreign articles were translated.The following search terms as medical subject headings and textwords were used:(“Preterm infant”OR“Premature Birth”[Mesh])OR(“Infant,Premature/classification”[Mesh] OR“Infant,Premature/growth and development”[Mesh] OR“Infant,Premature/statistics and numerical data”[Mesh] OR“Infant,very low birth weight”[Mesh])AND (percentile OR*centile*OR weeks)AND(weight OR head circumference OR length).Grey literature sites including clinical trial websites and Google were searched in February 2012.Reference lists were reviewed for relevant studies.All of the found data was reported as completed weeks except for the German Perinatal Statistics,which were reported as actual daily weights[14].To combine the datasets,the German data was temporarily converted to completed weeks.A final step converted the meta-analyses to actual age.bine the data to produce weighted intrauterine growth curves for each sexThe located data(3rd,10th,50th,90th,and97th percentiles for weight,head circumference,and length)that met the inclusion criteria were extracted by copying and pasting into spreadsheets.The male and female percentile curves from each included data set for weight,head circumference and length were plotted together so they could be examined visually for heterogeneity(Figures1,2, and3).The data for each gender were combined by using the weekly data for the percentiles:3rd,10th,50th,90th, and97th,weighted by the sample sizes.The combined data was represented by relatively smooth curves.C.Develop growth monitoring curvesTo develop the growth monitoring curves that joined the intrauterine meta-analysis data with the WHO Growth Standard(WHOGS)smoothly,the following cubic spline procedure was used to meet two objectives:a)To maintain integrity with the meta-analysis curvesfrom22to36weeks.Integrity of the fit wasassumed to be agreement within3%at each week. b)To ensure fit of the data to the WHO values at50weeks,within0.5%.Procedure:1)Cubic splines were used to interpolate smoothvalues between selected points(22,25,28,32,34,36 and50weeks).Extra points were manually selected at40,43and46weeks in order to produceacceptable fit through the underlying data.ThePreM Growth study(Fenton TR,Nasser R,Eliasziw M,Kim JH,Bilan D,Sauve R:Validating the weight gain of preterm infants between the referencegrowth curve of the fetus and the term infant,The Preterm Infant Multicentre Growth Study.Submitted BMC Ped2012)conducted to inform the transition between the preterm and WHO data,was used to inform this step.The Prem Growth Studyfound that preterm infants growth in weightfollowed approximately a straight line between37and45weeks,as others have also noted[9-11].2)LMS values(measures of skew,the median,and thestandard deviation)[15]were computed from theinterpolated cubic splines at weekly intervals.Cole’sprocedures[15]and an iterative least squares method were used to derive the LMS parameters(L=Box-Cox power,M=median,S=coefficient of variation)fromFigure1Boys birthweight centiles(3rd,50th and97th)from the six included studies,along with the boy’s meta-analysis curves (bold).Figure2Girls head circumference centiles(3rd,50th and97th) centiles from the included studies,along with the girl’smeta-analysis curves(dotted),and after40weeks,the World Health Organization centiles (dashed).Figure3Girls length centiles(3rd,50th and97th)centiles from the included studies,along with the meta-analysis curves (dotted),and after40weeks,the World Health Organization centiles(dashed).Table2Number of infants each week from each studyGestational age Voight,2010Olsen,2010Bertino,2010Kramer,2001Roberts,1999Bonellie,2008 Females Males Females Males Females Males Females Males Females Males Females Males 22188321----80827174--23431560133153381061147995--245757044384512024148156115135120126 257138466037224038184202136180115118 268129687738813558191234188235179172 271073120396610305261188254231284174177 2812761536118712817963287330287361246239 2915161838125415057072299392325397245265 301853221216061992107114390467440571317313 312283295620442460126140461584548743136148 32**300736771651837959978771117193205 33**418650142112401055136812001471239256 34**593672912633492018255320862657374422 35**508269523664183391431434184092644653 36**46907011562665820396487320878810481265 37**43726692129114921730819965161051866020062499 38**57558786352439764751651947478095140446306387 39**597883245295545275068776236884672871869910706 40**55297235567256531107381127371375701415531264414230 *Not reported.the multicentre meta-analyses for weight,headcircumference and length.The LMS splines weresmoothed slightly while maintaining data integrity asnoted above.3)The final percentile curves were produced from thesmoothed LMS values.4)A grid similar to the2003growth chart was used,but the growth curves were re-scaled along thex-axis from completed weeks to allow clinicians toplot infant growth by actual age in weeks,and aslight modification(scaled to60centimeters insteadof65)was made to the y-axis.pared the revised charts with the2003version The revised growth charts were compared graphically with the original2003Fenton preterm growth chart.To makethe differences in chart values more apparent,the2003 chart data was also shifted to actual weeks for these com-parison figures.ResultsSix large population based surveys[14,16-20]of size at preterm birth from countries Germany,United States, Italy,Australia,Scotland,and Canada were located that met the inclusion criteria(Table1).The literature search identified2436papers,of which2373were discarded as being not relevant or duplicates based on the titles (Figure4).Reviewing reference lists identified another 12studies.Seventy-five studies were examined in detail, however27of these did not meet the date criteria.Among the48studies that met the date of birth criteria,some did not meet the other inclusion criteria for the following reasons:Did not meet the criterion for more than25,000 babies[21-35],no low gestational age infants less than25 weeks[31,36-41],insufficient number less than30weeks [34,42-45],no statistical correction for inaccurate gestational ages[46-48],numerical data not available [49-51],number of infants each week were not available [52],number of infants in the subgroups each week were not available[53],was not population based[54-56],no direct measurements[27],some of the data[57]was also in one of the larger included studies[17].Included in the meta-analyses were almost four million (3,986,456)infants at birth(34,639less than30weeks) from six studies for weight(Table2),and173,612infants for head circumference,and151,527for length[16,18]. The World Health Organization data measurements were made longitudinally on882infants.The individual datasets from the literature showed good agreement with each other,especially along the 50th and lower centiles(Figures1,2,and3)and the meta-analysis curves had a close fit with the individual datasets up to36weeks and at50weeks(Figures5,6,7). The final splined weight curves were within3%of the meta-analysis curves for24through36weeks for both gen-ders,except for a3.8%difference for girls at32weeks along the90th centile.None of the length measurements differed by more than1.8%percent between the meta-analysis and the splined curves;all weeks of the head circumference curves were within 1.5%.The meta-analyses for headFigure5Boys meta-analysis weight curves(dotted)with the final smoothed growth chart curves (dashed).Figure6Boys meta-analysis head circumference curves (dotted)with the final smoothed growth chart curves (dashed). Figure7Boys meta-analysis length curves(dotted)with the final smoothed growth chart curves(dashed).circumference and length for girls and boys were close enough to normal distributions that normal distributions were used to summarize the data.The measures at50 weeks were within0.5%of the WHOGS values.Girl and boy charts were prepared(Figure8and9),by shifting the age by0.5weeks to allow plotting by exact age instead of completed weeks.The LMS Parameters [15]were used to develop the exact z-score and percentile calculators for the new growth chart.In the two graphical comparisons between the revised growth charts,one for each sex,with the2003Fenton preterm growth chart revealed that the curves were quite similar(Figures10and11).Generally the new girls’curves were slightly lower(Figure10)and the new boys’slightly higher(Figure11)for all3parameters(weight,head cir-cumference,and length)than the2003curves.The most dramatic visual and numerical difference between the new charts and the2003chart was the higher shift of the boys’weight curves after40weeks compared to the2003chart, reaching a maximum difference at50weeks of650,580, and740grams at the3rd,50th,and97th percentiles,re-spectively.The second biggest visual difference was thegrowth chart for girls.lower pattern of the girls’length curves below37weeks; the difference in length reached a maximum numerical value of1.7centimeters at24weeks along the97th percentile.DiscussionWe used a strict set of inclusion criteria to include only the best data available to convert fetal and infant size data into fetal-infant growth charts for preterm infants.The re-vised sex-specific actual-age(versus completed weeks) growth charts(Figure9and10),are based on birth size in-formation of almost four million births with confirmed or corrected gestational ages,born in developed countries (See Features of the new growth chart).The revised charts are based on the recommended growth goal for preterm infants,the fetus and the term infant,with smoothing of the disjunction between these datasets,based on the find-ings of our international multicentre validation study (Fenton TR,Nasser R,Eliasziw M,Kim JH,Bilan D,Sauve R:Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term in-fant,The Preterm Infant Multicentre Growth Study. Submitted BMC Ped2012).These charts are consist-ent with the meta-analysis data up to and includinggrowth chart for boys.36weeks,thus they can be used for the assessment of size for gestational age for preterm infants under37 weeks of gestational age.This growth chart is likely ap-plicable to preterm infants in both developed and de-veloping countries since the data was selected from developed countries to minimize the influence from cir-cumstances that may not have been ideal to support growth.Features of the new growth chartBased on the recommended growth goal for preterm infants:The fetus and the term infantGirl and boy specific chartsEquivalent to the WHO growth charts at50weeks gestational age(10weeks post term age).Large preterm birth sample size of4million infants; Recent population based surveys collected between 1991to2007Data from developed countries includingGermany,Italy,United States,Australia,Scotland, and CanadaCurves are consistent with the data to36weeks, thus can be used to assign size for gestational age up to and including36weeks.Chart is designed to enable plotting as infants are measured,not as completed weeks.The x axis wasadjusted for this chart so that infant size data can be plotted without age adjustment,i.e.Babies should be plotted as exact ages,that is a baby at253/7weeksshould be plotted along the x axis between25and26weeks.Exact z-score and percentile calculator available for download from http://ucalgary.ca/fenton.Data isavailable for research upon request.It may be more intuitive to plot on growth charts using exact ages rather than on the basis of completethe revised growth chart for girls(solid curves)and the2003Fenton growth chart for length,head circumference,and weight).Both the2003and the revised growthweeks.Several years ago,the WHO used completed age for growth chart development[12].This recommenda-tion was likely due to the way data had been collected in the past,that is all260/7through266/7week infants were included in the26week completed week category. However,with the use of computers to plot on growth charts comes the potential to more accurately plot mea-surements to the exact day of data collection.Thus the time scale of the horizontal axes of these new growth charts were re-scaled to actual age,for ease of use and un-derstanding.For example,a baby at253/7can be intui-tively plotted between25and26weeks.Exact z-score and centile calculators for the revised charts are available for download:http://ucalgary.ca/ fenton.Data is available for research upon request.The data revealed that between22weeks to50weeks post menstrual age,the fetus/infant multiplies its weight tenfold,for example,the girls’median weight increased from a median ing a fetal-infant growth chart allows clinicians to compare preterm infants’growth to an estimated reference of the fetus and the term infant.There was a remarkably close fit of the included preterm surveys for weight,head circumference and length from the6countries,especially at the50th percentile,even though the data came from different countries.The splining procedures we used have produced a chart that has integrity and good agreement with the original data.Smoothing of the LMS parameters is recommended since minor fluctuations are more likely due to sampling errors rather than physiological events [15].Experts recommend that growth charts be developed based on smoothed L,M and S,to constrain the adjacent curves so that they relate to each other smoothly[15].The World Health Organization set their L parameter to1for head circumference and length,while they maintained the exact L values for infants’weights[58].The data under study here revealed the same effect as the WHO data;wethe revised growth chart for boys(solid curves)and the2003Fenton growth chart for length,head circumference,and weight).Both the2003and the revised growthfound that both head circumference and length were close enough to normal distributions that normal distributions could summarize the data,while the exact L’s were needed to retain the nuances of the weight curves.The differences between the revised growth charts and the2003Fenton preterm growth chart may reflect improvements since the selected preterm growth references for the new versions are more likely globally representative of fetal and infant growth.Some of the differences between the current charts and the2003version are likely due to the separation into girl and boy charts,since the shifts of the girls’curves tend to be downward and the boys’curves upward.The weight shifts after40weeks were upward for both sexes,due to the higher values for the WHOGS compared to the CDC growth reference[59]at 10weeks post term.The ideal growth pattern of preterm infants remains undefined.These revised growth charts were developed based on the growth patterns of the fetus(as has been determined by size at birth in the large population stud-ies)and the term infant(based on the WHO Growth Standard)[2].Ultrasound studies and comparison of subgroups of prematurely born infants suggest that the fetal studies,such as those used in this development,may be biased by the premature birth since fetuses who remain in utero likely differ in important ways from babies who are born early[60,61].However,fetal size from these imperfect studies may be the best data available at this point in time for comparing the growth of preterm infants since the alternative,to compare to in utero infants requires extrapolation from ultrasound measurements.To use other premature infants as the growth reference for preterm infants may not be ideal since the ideal growth of preterm infants has not been defined,has been changing over time[62],and is influenced by the nutrition and medical care received after birth[63,64].Although the WHOGS is considered to be a growth standard,the infants in the population-based surveys of size at birth are more likely representative of the reference populations and were not selected to be healthy.Thus these growth charts are growth references and are not a growth standard.The INTERGROWTH study,currently underway,will rectify this problem,since their purpose is to develop prescriptive standards for fetal and preterm growth[65].ConclusionThe inclusion of data from a number of developed countries increases the generalizability of the growth chart.The revised preterm growth chart,harmonized with the World Health Organization Growth Standard at50weeks,may support an improved transition of preterm infant growth monitoring to the WHO peting interestsThe authors declare that they have no competing interests.Authors’contributionsThe author’s responsibilities were as follows:JHK suggested the study,TRF& JHK designed the study and conducted independent literature searches,TRF extracted the data,performed the statistical analysis,and wrote the manuscript.Both of the authors contributed to interpret the findings and writing the manuscript,and both authors read and approved the final manuscript.AcknowledgementsMany thanks to Patrick Fenton and Misha Eliasziw for statistical assistance, Roseann Nasser,Reg Sauve,Debbie O’Connor,and Sharon Unger for encouragement and advice,and Jayne Thirsk for editing advice.Author details1Alberta Children’s Hospital Research Institute,The University of Calgary, Calgary,AB,Canada.2Department of Community Health Sciences,The University of Calgary,3280Hospital Drive NW,Calgary,AB,Canada.3Division of Neonatology,UC San Diego Medical Center,200West Arbor Drive MPF 1140,San Diego,CA,USA.Received:12October2012Accepted:10April2013Published:20April2013References1.Secker D:Promoting optimal monitoring of child growth in Canada:using the new WHO growth charts.Can J Diet Pract Res2010,71:e1–e3. 2.De Onis M,Garza C,Victora CG,Onyango AW,Frongillo EA,Martines J:TheWHO Multicentre Growth Reference Study:planning,study design,and methodology.Food Nutr Bull2004,25:S15–S26.3.Borghi E,De Onis M,Garza C,den BJ V,Frongillo EA,Grummer-Strawn L,Van Buuren S,Pan H,Molinari L,Martorell R,Onyango AW,Martines JC:Construction of the World Health Organization child growth standards: selection of methods for attained growth curves.Stat Med2006,25:247–265.4.Dietitians of Canada,Canadian Pediatric Society,College of FamilyPhysicians of Canada,Community Health Nurses of Canada:PromotingOptimal Monitoring of Child Growth in Canada:Using the New WHOGrowth Charts.Can J Diet Pract Res2010,71:1–22.mittee on Nutrition American Academy Pediatrics:Nutritional Needs ofPreterm Infants,Pediatric Nutrition Handbook.6th edition.Elk Grove Village Il:American Academy Pediatrics;2009.6.Agostoni C,Buonocore G,Carnielli VP,De CM,Darmaun D,Decsi T,et al:Enteral nutrient supply for preterm infants.A comment of the ESPGHANCommittee on Nutrition.J Pediatr Gastroenterol Nutr2010,50:85–91.7.Nutrition Committee,Canadian Paediatric Society:Nutrient needs andfeeding of premature infants.CMAJ1995,152:1765–1785.8.United Nations Statistics Division:Composition of macro geographical(continental)regions,geographical sub-regions,and selected economic andother groupings./unsd/methods/m49/m49regin.htm#developed.9.Niklasson A,Engstrom E,Hard AL,Wikland KA,Hellstrom A:Growth in verypreterm children:a longitudinal study.Pediatr Res2003,54:899–905. 10.Bertino E,Coscia A,Mombro M,Boni L,Rossetti G,Fabris C,Spada E,MilaniS:Postnatal weight increase and growth velocity of very low birthweight infants.Arch Dis Child Fetal Neonatal Ed2006,91:F349–F356.11.Krauel VX,Figueras AJ,Natal PA,Iglesias PI,Moro SM,Fernandez PC,Martin-Ancel A:Reduced postnatal growth in very low birth weight newborns with GE<or=32weeks in Spain.An Pediatr(Barc)2008,68:206–212. 12.World Health Organization:Physical status:the use and interpretation ofanthropometry.Report of a WHO Expert Committee.World Health Organ Tech Rep Ser1995,854:1–452.13.Hennekens CH,Buring JE:Analysis of epidemiologic studies:Evaluatingthe role of confounding.In Epidemiology in Medicine.Edited by Mayrent SL, Little B.Boston;1987:287–323.14.Voigt M,Zels K,Guthmann F,Hesse V,Gorlich Y,Straube S:Somaticclassification of neonates based on birth weight,length,and headcircumference:quantification of the effects of maternal BMI andsmoking.J Perinat Med2011,39:291–297.15.Cole TJ,Green PJ:Smoothing reference centile curves:the LMS methodand penalized likelihood.Stat Med1992,11:1305–1319.16.Olsen IE,Groveman SA,Lawson ML,Clark RH,Zemel BS:New intrauterinegrowth curves based on United States data.Pediatrics2010,125:e214–e224.17.Roberts CL,Lancaster PA:Australian national birthweight percentiles bygestational age.Med J Aust1999,170:114–118.18.Bertino E,Spada E,Occhi L,Coscia A,Giuliani F,Gagliardi L,Gilli G,Bona G,Fabris C,De CM,Milani S:Neonatal anthropometric charts:the Italianneonatal study compared with other European studies.J PediatrGastroenterol Nutr2010,51:353–361.19.Bonellie S,Chalmers J,Gray R,Greer I,Jarvis S,Williams C:Centile charts forbirthweight for gestational age for Scottish singleton births.BMCPregnancy Childbirth2008,8:5.20.Kramer MS,Platt RW,Wen SW,Joseph KS,Allen A,Abrahamowicz M,Blondel B,Breart G:A new and improved population-based Canadianreference for birth weight for gestational age.Pediatrics2001,108:E35. 21.Karna P,Brooks K,Muttineni J,Karmaus W:Anthropometric measurementsfor neonates,23to29weeks gestation,in the1990s.Paediatr PerinatEpidemiol2005,19:215–226.22.Kwan AL,Verloove-Vanhorick SP,Verwey RA,Brand R:Ruys JH:[Birthweight percentiles of premature infants needs to be updated].Ned Tijdschr Geneeskd1994,138:519–522.23.Riddle WR,DonLevy SC,Lafleur BJ,Rosenbloom ST,Shenai JP:Equationsdescribing percentiles for birth weight,head circumference,and length of preterm infants.J Perinatol2006,26:556–561.24.Figueras F,Figueras J,Meler E,Eixarch E,Coll O,Gratacos E,Gardosi J,Carbonell X:Customised birthweight standards accurately predictperinatal morbidity.Arch Dis Child Fetal Neonatal Ed2007,92:F277–F280. 25.Fok TF,So HK,Wong E,Ng PC,Chang A,Lau J,Chow CB,Lee WH:Updatedgestational age specific birth weight,crown-heel length,and headcircumference of Chinese newborns.Arch Dis Child Fetal Neonatal Ed2003, 88:F229–F236.26.Cole TJ,Williams AF,Wright CM:Revised birth centiles for weight,lengthand head circumference in the UK-WHO growth charts.Ann Hum Biol2011,38:7–11.27.Salomon LJ,Bernard JP,Ville Y:Estimation of fetal weight:reference rangeat20–36weeks’gestation and comparison with actual birth-weightreference range.Ultrasound Obstet Gynecol2007,29:550–555.28.Cole TJ,Freeman JV,Preece MA:British1990growth reference centiles forweight,height,body mass index and head circumference fitted bymaximum penalized likelihood.Stat Med1998,17:407–429.29.Gibbons K,Chang A,Flenady V,Mahomed K,Gardener G,Gray PH:Validation and refinement of an Australian customised birthweightmodel using routinely collected data.Aust N Z J Obstet Gynaecol2010,50:506–511.30.Ogawa Y,Iwamura T,Kuriya N,Nishida H,Takeuchi H,Takada M:Birth sizestandards by gestational age for Japanese neonates.Acta Neonat Jpn1998,34:624–632.31.Storms MR,Van Howe RS:Birthweight by gestational age and sex at arural referral center.J Perinatol2004,24:236–240.32.Romano-Zelekha O,Freedman L,Olmer L,Green MS,Shohat T:Should fetalweight growth curves be population specific?Prenat Diagn2005,25:709–714.33.Ooki S,Yokoyama Y:Reference birth weight,length,chest circumference,and head circumference by gestational age in Japanese twins.J Epidemiol2003,13:333–341.34.Vergara G,Carpentieri M,Colavita C:Birthweight centiles in preterminfants.A new approach.Minerva Pediatr2002,54:221–225.35.Bernstein IM,Mohs G,Rucquoi M,Badger GJ:Case for hybrid“fetal growthcurves”:a population-based estimation of normal fetal size acrossgestational age.J Matern Fetal Med1996,5:124–127.36.Ramos F,Perez G,Jane M,Prats R:Construction of the birth weight bygestational age population reference curves of Catalonia(Spain):Methods and development.Gac Sanit2009,23:76–81.37.Visser GH,Eilers PH,Elferink-Stinkens PM,Merkus HM,Wit JM:New Dutchreference curves for birthweight by gestational age.Early Hum Dev2009, 85:737–744.38.Roberts C,Mueller L,Hadler J:Birth-weight percentiles by gestational age,Connecticut1988–1993.Conn Med1996,60:131–140.39.Zhang X,Platt RW,Cnattingius S,Joseph KS,Kramer MS:The use ofcustomised versus population-based birthweight standards in predicting perinatal mortality.BJOG2007,114:474–477.40.Gielen M,Lindsey PJ,Derom C,Loos RJ,Souren NY,Paulussen AD,ZeegersMP,Derom R,Vlietinck R,Nijhuis JG:Twin-specific intrauterine‘growth’charts based on cross-sectional birthweight data.Twin Res Hum Genet2008,11:224–235.41.Monroy-Torres R,Ramirez-Hernandez SF,Guzman-Barcenas J,Naves-SanchezJ:[Comparison between five growth curves used in a public hospital].Rev Invest Clin2010,62:121–127.42.Blair EM,Liu Y,de Klerk NH,Lawrence DM:Optimal fetal growth for theCaucasian singleton and assessment of appropriateness of fetal growth:an analysis of a total population perinatal database.BMC Pediatr2005,5:13. 43.Carrascosa A,Yeste D,Copil A,Almar J,Salcedo S,Gussinye M:[Anthropometric growth patterns of preterm and full-term newborns(24–42weeks’gestational age)at the Hospital Materno-Infantil Valld’Hebron(Barcelona)(1997–2002].An Pediatr(Barc)2004,60:406–416. 44.Rousseau T,Ferdynus C,Quantin C,Gouyon JB,Sagot P:[Liveborn birth-weight of single and uncomplicated pregnancies between28and42weeks of gestation from Burgundy perinatal network].J Gynecol Obstet Biol Reprod(Paris)2008,37:589–596.45.Polo A,Pezzotti P,Spinelli A,Di LD:Comparison of two methods forconstructing birth weight charts in an Italian region.Years2000–2003.Epidemiol Prev2007,31:261–269.46.Oken E,Kleinman KP,Rich-Edwards J,Gillman MW:A nearly continuousmeasure of birth weight for gestational age using a United Statesnational reference.BMC Pediatr2003,3:6.47.Montoya-Restrepo NE,Correa-Morales JC:[Birth-weight curves].Rev SaludPublica(Bogota)2007,9:1–10.48.Dollberg S,Haklai Z,Mimouni FB,Gorfein I,Gordon ES:Birth weightstandards in the live-born population in Israel.Isr Med Assoc J2005,7:311–314.49.Kierans WJ,Kendall PRW,Foster LT,Liston RM,Tuk T:New birth weight andgestational age charts for the British Columbia population.BC Medical J 2006,48:28–32.50.Uehara R,Miura F,Itabashi K,Fujimura M,Nakamura Y:Distribution of birthweight for gestational age in Japanese infants delivered by cesareansection.J Epidemiol2011,21:217–222.51.Lipsky S,Easterling TR,Holt VL,Critchlow CW:Detecting small forgestational age infants:the development of a population-basedreference for Washington state.Am J Perinatol2005,22:405–412.52.Niklasson A,Albertsson-Wikland K:Continuous growth reference from24th week of gestation to24months by gender.BMC Pediatr2008,8:8.53.Alexander GR,Kogan MD,Himes JH:1994–1996U.S.singleton birthweight percentiles for gestational age by race,Hispanic origin,andgender.Matern Child Health J1999,3:225–231.54.Davidson S,Sokolover N,Erlich A,Litwin A,Linder N,Sirota L:New andimproved Israeli reference of birth weight,birth length,and headcircumference by gestational age:a hospital-based study.Isr Med Assoc J 2008,10:130–134.55.Kato N,A:[Reference birthweight for multiple births in Japan].NihonKoshu Eisei Zasshi2002,49:361–370.56.Braun L,Flynn D,Ko CW,Yoder B,Greenwald JR,Curley BB,Williams R,Thompson MW:Gestational age-specific growth parameters for infants born at US military hospitals.Ambul Pediatr2004,4:461–467.57.Thomas P,Peabody J,Turnier V,Clark RH:A new look at intrauterinegrowth and the impact of race,altitude,and gender.Pediatrics2000,106:E21.58.World Health Organization:The WHO Child Growth Standards.http://www.who.int/childgrowth/standards/en/.59.Kuczmarski RJ,Ogden CL,Guo SS,Grummer-Strawn LM,Flegal KM,Mei Z,Wei R,Curtin LR,Roche AF,Johnson CL:2000CDC Growth Charts for the United States:methods and development.Vital Health Stat2002,11:1–190.60.Hutcheon JA,Platt RW:The missing data problem in birth weightpercentiles and thresholds for“small-for-gestational-age”.Am J Epidemiol 2008,167:786–792.61.Sauer PJ:Can extrauterine growth approximate intrauterine growth?Should it?Am J Clin Nutr2007,85:608S–613S.62.Christensen RD,Henry E,Kiehn TI,Street JL:Pattern of daily weightsamong low birth weight neonates in the neonatal intensive care unit:data from a multihospital health-care system.J Perinatol2006,26:37–43.63.Valentine CJ,Fernandez S,Rogers LK,Gulati P,Hayes J,Lore P,Puthoff T,Dumm M,Jones A,Collins K,Curtiss J,Hutson K,Clark K,Welty SE:Early。
儿童生长发育曲线对照表
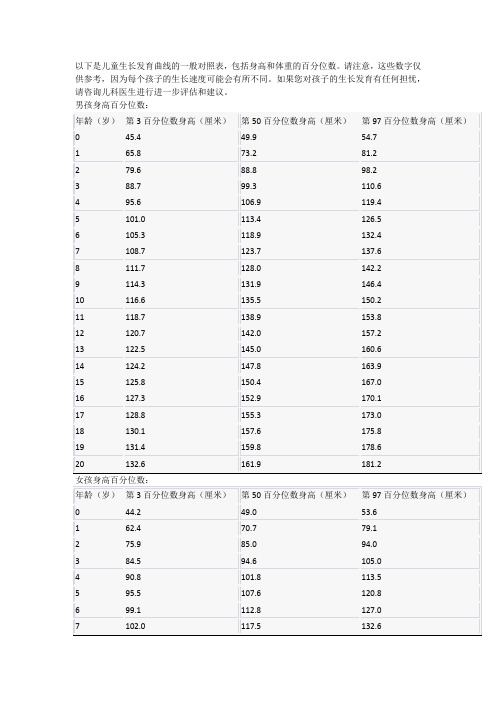
以下是儿童生长发育曲线的一般对照表,包括身高和体重的百分位数。
请注意,这些数字仅供参考,因为每个孩子的生长速度可能会有所不同。
如果您对孩子的生长发育有任何担忧,请咨询儿科医生进行进一步评估和建议。
这些数据是根据世界卫生组织(World Health Organization)发布的标准进行估算的。
请记住,这只是一般的参考值,不代表所有儿童的生长曲线。
每个孩子都是独特的,其生长和发育过程受到多种因素的影响,包括遗传、营养、健康状况和环境等。
儿童生长曲线记录
儿童生长曲线记录
儿童生长曲线记录是指记录儿童在不同年龄段的身高、体重、头围等生长指标,以便评估其生长发育状况是否正常。
通常,这些记录是通过测量儿童的身体尺寸,然后将数据与同龄儿童的平均值进行比较。
儿童生长曲线通常使用百分位数来表示,例如,50%的身高百
分位数表示与同龄儿童中的中等身高相对比。
生长曲线记录的目的是跟踪儿童的生长趋势,并及时发现可能存在的生长问题。
通过儿童生长曲线记录,医生可以根据儿童的生长速度和生长曲线是否正常来判断儿童是否存在生长问题,如生长缓慢、过快或偏离正常范围。
当发现问题时,医生可以及时采取相应的干预措施,如调整饮食、推荐适当的运动或进行进一步的检查等。
儿童生长曲线记录还可以帮助父母了解自己孩子的生长发育状况,并参考同龄儿童的平均值和标准差来评估孩子的相对位置。
这可以帮助父母更好地了解孩子的健康状况,提供关于营养和生活方式的指导,并在必要时咨询医生。
儿童 生长曲线
儿童生长曲线1. 引言儿童的生长与发育是一个复杂而又持续的过程。
了解儿童的生长曲线对于评估其健康状况、制定适当的营养计划以及预防和治疗相关疾病非常重要。
本文将介绍儿童生长曲线的概念、使用方法以及其在临床实践中的应用。
2. 儿童生长曲线的概念儿童生长曲线是描述儿童体格发育变化的统计工具。
它由大量被纳入统计分析的儿童数据所构建,通常基于年龄、性别和地理区域等因素进行分类。
常见的儿童生长曲线有身高、体重、头围等指标。
3. 常用的儿童生长曲线3.1 身高曲线身高是评估儿童发育情况最直观、最常用的指标之一。
根据不同年龄段和性别,可以绘制出身高百分位数曲线图,例如CDC(美国疾控中心)或WHO(世界卫生组织)的曲线图。
这些曲线图将儿童的身高与同龄儿童进行比较,可以帮助判断儿童是否存在生长迟缓或超前的情况。
3.2 体重曲线体重是另一个重要的指标,可以反映儿童的营养状况和整体健康状况。
类似于身高曲线,体重百分位数曲线图可以用来评估儿童是否存在体重不足或超重等问题。
在临床实践中,医生可以根据这些曲线图来制定个性化的营养计划和干预措施。
3.3 头围曲线头围是评估婴幼儿脑发育情况的指标之一。
通常在出生后的几个月内进行头围测量,并绘制相应的头围百分位数曲线图。
异常的头围增长速度可能提示脑发育问题,如颅内压增高或脑积水等。
4. 如何使用儿童生长曲线4.1 绘制个体生长曲线对于单个儿童,可以根据其年龄和性别,在相应的生长曲线图上标记其身高、体重或头围数据点。
通过观察这些数据点在曲线上的位置,可以评估儿童的生长状况是否正常。
4.2 比较群体生长曲线通过将多个儿童的数据点绘制在同一张曲线图上,可以比较不同群体之间的生长差异。
例如,可以比较男女儿童、城市和农村地区的儿童等。
这种比较有助于揭示不同因素对儿童生长发育的影响。
4.3 监测儿童生长变化定期监测儿童的生长变化是非常重要的。
通过定期测量身高、体重和头围,并与相应的生长曲线进行比较,可以及时发现可能存在的问题,并采取相应措施进行干预。
世卫组织最新标准 - (0-5岁)体重生长曲线图 身高生长曲线图 BMI生长曲线图

世卫组织最新标准 - (0-5岁)体重生长曲线图 ~ 身高生长曲线图 ~ BMI生长曲线图世界卫生组织的最新标准是完全根据母乳宝宝的生长情况制定的。
而我国的标准是综合国内不同地区和不同喂养分方式的数据统计出来的。
但这样的数据并不能说明它更正确,而恰恰会由于混合或人工喂养宝宝的因素使数据偏高。
这些新指标是基于8440名母乳喂养的孩子的生长发育状况做出的。
与吃母乳的婴幼儿比起来,吃配方奶的孩子体重比吃母乳的孩子要增长得快些。
而“世卫组织”旧的有关婴幼儿的成长发育指标却是根据吃配方奶的孩子的发育情况制定的,这就意味着这一套标准存在着重大缺陷。
从1997年到2003年间,世界卫生组织对包括巴西等6个国家的孩子进行了跟踪调查。
这些孩子来自巴西、加纳、印度、挪威、阿曼和美国等6个不同的国家,身体都很健康,且他们的母亲都不吸烟,对孩子的照顾也非常周到。
而之前的指标只是取单独一个国家的儿童为样本(也就是美国儿科学会公布的美国婴幼儿生长发育曲线)。
男宝BMI生长曲线图女宝BMI生长曲线图新的婴幼儿生长发育指标中还包含了身体质量指数(BMI=体重(公斤)÷身高(米)的平方,单位为公斤/平方米),这是WHO首次在婴幼儿生长发育指标中引入此项指标。
BMI为评估体重与身高比例提供了工具,对于监控孩子的肥胖症非常有效。
它是评估儿童健康的一个重大革新。
男宝宝体重生长曲线图专家认为,新指标的发表不会给中国孩子生长发育情况带来大影响。
我国每10年都要在北部、中部、南部各选三地,对0-18岁儿童和青少年的身高、体重等情况进行调查统计,并综合了各种喂养方式,得出我国儿童的身高、体重等指标的参照值。
用生长曲线检测孩子的身高、体重的发育,比起简单用一个数字断定孩子是高是胖要更科学。
使用方法如下:1、做顺时记录。
每个月为孩子测量一次身高、体重,把测量结果描绘在生长曲线图上(不要在孩子生病期间测量),连成一条曲线。
如果孩子的生长曲线一直在正常值范围内(3号线到-3号线之间)匀速顺时增长就是正常的。
生长发育曲线

生长发育曲线怎么知道孩子生长发育是否正常,怎么掌握孩子的自身生长发育规律呢?这就要利用生长发育曲线了。
生长发育曲线是通过检测众多正常婴幼儿发育过程后描绘出来的,整个曲线由若干条连续曲线组成。
0-5岁男孩身高发育曲线0-5岁女孩身高发育曲线0-5岁男孩体重发育曲线从生长曲线判断发育速度GoTop年轻的爸爸妈妈们带孩子一起玩时,在一起聊天时,带孩子体检时,都会互相交流孩子的生长状况,看看别人家的孩子现在多高了、多重了,再和自己的孩子比一比。
一比之下,有喜有忧:如果孩子长得偏快,家长心中就暗暗高兴;如果长得偏慢,家长心中则忐忑不安。
难道每个同龄的孩子都要具有一样的身高、体重等发育指标,家长才不会担心吗?究竟如何评价孩子的生长才准确呢?诊室场景回放镜头1宝宝为孕38周经自然分娩的男婴,出生体重3.2千克、身长49厘米,纯母乳喂养。
生后前4个月的体重分别为4.2千克、5.4千克、6.2千克和6.8千克;身长分别为54.5厘米、58厘米、61厘米和63.5厘米。
体重/身长指数始终保持在50%水平。
与同龄孩子相比,妈妈总觉得自己的孩子偏小,担心孩子出现生长落后。
甚至怀疑自己的母乳营养不够丰富,耽误了孩子生长发育。
诊室场景回放镜头2强强也是足月顺产出生的男婴,出生体重4.2千克、身长51.5厘米,用婴儿配方奶喂养,妈妈是严格按照奶粉包装罐上的推荐用量给孩子喂养。
生后前4 个月的体重分别为5.05千克、6.1千克、6.8千克和7.2千克;身长分别为56.5厘米、60厘米、63厘米和66厘米。
体重/身长指数起在75%水平,逐渐降至50%水平,4个月时降至20%水平。
诊室场景回放镜头3壮壮是经剖宫产出生的男婴,出生体重3.6千克、身长51厘米,生后混合喂养,喂养过程非常顺利。
生后前4个月的体重分别为5.4千克、6.8千克、8千克和9千克;身长分别为57厘米、61厘米、64.5厘米和67.5厘米。
出生时体重/身高指数在50%水平,以后迅速上升,满4个月时达到90%水平。
儿童发育曲线

儿童发育曲线
儿童发育曲线是指儿童在生长发育过程中身高、体重、头围等指标随着年龄的增长而变化的曲线。
这些指标的变化反映了儿童的生长发育状况,也是评估儿童健康状况的重要指标之一。
在出生后的第一年,婴儿的身高和体重增长非常迅速,这是因为婴儿在出生后需要适应新的环境,需要大量的营养来支持身体的发育。
在第一年内,婴儿的身高和体重增长速度最快,平均每个月增长2.5-3.5厘米,体重增加约700-800克。
从1岁到3岁,儿童的身高和体重增长速度开始逐渐减缓,但仍然比较快。
在这个阶段,儿童的身高和体重增长速度平均每年分别为6-8厘米和2-3公斤。
此时,儿童的头围也开始逐渐增大,反映了大脑的发育状况。
从3岁到6岁,儿童的身高和体重增长速度进一步减缓,但仍然比较明显。
在这个阶段,儿童的身高和体重增长速度平均每年分别为4-6厘米和1.5-2公斤。
此时,儿童的头围增长速度也开始减缓。
从6岁到青春期,儿童的身高和体重增长速度进一步减缓,但仍然存在。
在这个阶段,儿童的身高和体重增长速度平均每年分别为2-4厘米和1-2公斤。
此时,儿童的头围增长速度几乎停止。
需要注意的是,儿童的生长发育曲线存在个体差异,有些儿童可能生长发育速度较快,有些儿童可能生长发育速度较慢。
因此,家长
应该根据自己孩子的生长发育情况,合理安排孩子的饮食和运动,以促进孩子的健康成长。
同时,家长也应该定期带孩子进行体检,了解孩子的生长发育情况,及时发现问题并采取相应的措施。
婴幼儿生长发育曲线

婴幼儿生长发育曲线什么是生长发育曲线生长发育曲线简单来说,是将宝宝在不同月龄测得的体重值、身高值、头围值以及匀称度,分别绘制成的4条曲线。
通过生长曲线图:●可以直观、快速地了解宝宝到底“长得好不好”;●通过连续追踪观察,可以评估甚至预测宝宝的生长发育趋势,能够及时发现生长轨迹是否偏离正常水平;●对于早产儿、低体重儿,利用它还可以评估宝宝追赶生长的情况。
●我国采用的标准是综合世界卫生组织、国内不同地区和不同喂养方式的数据统计出来。
生长发育曲线如何绘制正确测量宝宝身高、体重、头围,是描绘生长发育曲线的重要前提。
1.身长2岁以内:测身长时,应让宝宝平躺着量。
方法是让宝宝平躺,双腿捋顺、捋直,双脚并拢,头顶上放一本硬质的书,脚底下放一本硬质的书。
平行移动两本书,测量两本书之间的直线距离,就是宝宝的身长。
2岁以上:可以让宝宝站着测量,取其身高值。
注意事项:1)躺着测量时,要保证宝宝躺的地方要偏硬一些。
如果在太软的地方测量,宝宝身体会陷下去一些,测量的结果肯定就会偏短。
2)为了确保测量结果的准确性,家长需要给宝宝测量三遍,取平均数值。
3)今后每次测量,尽量都让宝宝在同一个位置进行。
2.体重体重是反映宝宝营养状况最灵敏的指标,某些疾病可以使孩子的体重在较短时间内发生变化,婴幼儿尤为明显。
测量工具与方法:婴儿秤或普通的电子秤均可(每次测量尽量使用同一个秤)。
注意事项:宝宝的体重是用克计算的,所以无论什么时候测,尽量在同样的条件下进行。
比如刚吃完100毫升奶的孩子和没吃奶的孩子,体重最起码能差100多克。
再比如一宿没换尿不湿的孩子与换了尿不湿的孩子最少差半斤,这对于基数就很小的宝宝来说,是非常大的误差了。
3.头围头围能反映脑和颅骨的发育情况。
测量方法:step 1:找到宝宝两条眉毛的中心点作为1点;step 2:找到宝宝后脑勺最高的位置(枕骨最高点)作为2点;step 3:拿软尺从1点经2点再回到1点,所测得的最大距离就是宝宝的头围啦。
世界卫生组织的婴儿生长曲线

世界卫生组织的婴儿生长曲线婴儿生长曲线是衡量和监测婴儿生长的重要工具,它们可以显示婴儿在不同年龄阶段的体重、身高、头围等指标的增长趋势。
世界卫生组织制定了一套婴儿生长曲线,为全球范围内的婴儿生长提供了参考标准。
1.体重体重是衡量婴儿生长的重要指标之一。
世界卫生组织的婴儿生长曲线以体重为纵坐标,年龄为横坐标绘制而成。
根据这些曲线,家长可以了解宝宝的体重是否在正常范围内,并根据需要采取相应的措施。
2.身高身高也是反映婴儿生长的重要指标之一。
世界卫生组织的婴儿生长曲线以身高为纵坐标,年龄为横坐标绘制而成。
通过比较宝宝的身高与标准曲线,家长可以了解宝宝的身高发育情况。
3.头围头围反映了婴儿头部的大小,与大脑发育密切相关。
世界卫生组织的婴儿生长曲线以头围为纵坐标,年龄为横坐标绘制而成。
家长可以通过监测宝宝的头围来了解宝宝的大脑发育情况。
4.胸围胸围是衡量婴儿胸廓大小的重要指标。
世界卫生组织的婴儿生长曲线以胸围为纵坐标,年龄为横坐标绘制而成。
通过监测宝宝的胸围,家长可以了解宝宝的胸腔发育情况。
5.上臂围上臂围是衡量婴儿上臂肌肉发育情况的重要指标。
世界卫生组织的婴儿生长曲线以上臂围为纵坐标,年龄为横坐标绘制而成。
通过监测宝宝的上臂围,家长可以了解宝宝的肌肉发育情况。
6.腹围腹围是衡量婴儿腹部发育情况的重要指标。
世界卫生组织的婴儿生长曲线以腹围为纵坐标,年龄为横坐标绘制而成。
通过监测宝宝的腹围,家长可以了解宝宝的腹部发育情况。
7.大腿围大腿围是衡量婴儿下肢肌肉发育情况的重要指标。
世界卫生组织的婴儿生长曲线以上腿围为纵坐标,年龄为横坐标绘制而成。
通过监测宝宝的大腿围,家长可以了解宝宝下肢的肌肉发育情况。
8.坐高坐高是衡量婴儿坐姿时的高度,与宝宝的脊柱发育和骨盆底肌肉发育有关。
世界卫生组织的婴儿生长曲线以坐高为纵坐标,年龄为横坐标绘制而成。
通过监测宝宝的坐高,家长可以了解宝宝的脊柱和骨盆底肌肉的发育情况。
总之,世界卫生组织的婴儿生长曲线是监测和评估婴儿生长的重要工具。
儿童身高生长曲线
儿童身高生长曲线儿童身高生长曲线是描述儿童身高发育的一种图表,通常以年龄为横坐标,身高为纵坐标,通过统计一定范围内的儿童身高数据,绘制出一条曲线,以反映儿童身高的平均水平和分布情况。
该曲线是儿童生长发育评估的重要工具,可以帮助医生和家长判断儿童身高是否正常,及时发现身高发育异常的儿童,及时采取措施进行干预。
儿童身高生长曲线的绘制基于大量的儿童身高数据,这些数据来源于国内外多个地区、不同年代的儿童,经过统计分析,得出了不同年龄段的儿童身高平均值和标准差。
平均值反映了儿童身高的中心位置,标准差反映了儿童身高的分布情况,即身高差异的大小。
在绘制曲线时,通常采用3个标准差为一个区间,将曲线分为多个百分位数线,如第3、10、25、50、75、90和97等百分位数线,其中50百分位数线即为儿童身高的中位数,表示有一半的儿童身高高于该值,一半的儿童身高低于该值。
儿童身高生长曲线的绘制有多种方法,常用的有NCHS、WHO和中国标准等。
其中,NCHS曲线是最早应用的曲线,主要适用于美国和加拿大等北美地区的儿童;WHO曲线是在NCHS曲线基础上进行修订的,适用于全球范围内的儿童;中国标准曲线是根据中国儿童身高数据绘制的,适用于中国儿童。
不同的曲线标准有不同的特点和使用范围,选择合适的曲线标准对于准确评估儿童身高发育非常重要。
儿童身高生长曲线的应用非常广泛,除了用于儿童身高发育评估外,还可用于儿童健康管理、儿童营养干预、儿童生长发育研究等方面。
例如,在儿童健康管理中,医生可根据儿童身高生长曲线评估儿童身高发育是否正常,及时发现身高发育异常的儿童,并根据曲线数据制定合理的营养干预方案;在儿童生长发育研究中,研究人员可通过对儿童身高生长曲线的分析,探讨儿童身高发育的影响因素、发育规律等问题,为儿童健康发展提供科学依据。
总之,儿童身高生长曲线是儿童身高发育评估的重要工具,具有广泛的应用价值。
家长和医生应密切关注儿童身高发育情况,及时进行评估和干预,为儿童的健康成长提供保障。
早产儿生长发育评估

早产儿生长发育评估评估早产儿生长发育指标是儿保重要任务。
本文以生长曲线评估为切入点对早产儿生长发育评估的研究进展作一综述。
不同评估标准之间存在差异、标准建立的理念基础等都存在矛盾,后续的研究仍是任重而道远。
标签:早产儿; 生长曲线早产儿是指出生时胎龄<37周的新生儿,其中出生体重<1500 g者为极低出生体重儿,<1000 g为超低出生体重儿【1】。
在我国,早产发生率约为7-15%,在发达国家约为6-11%,并存在增加的趋势【2】。
早产儿的生长可能与足月儿的生长并不匹配,对于如何监测早产儿的生长,以及如何确定这些早产儿的理想生长模式,国际上还没有共识【3】。
我们以生长曲线评估为切入点对早产儿生长发育评估的研究进展作一综述。
1.生长曲线评估1.1Fenton2013Fenton2013是应用META分析方法,纳入美国、瑞典等四个发达国家人口调查数据制成。
纳入早产儿样本约400万,是目前临床常用的生长曲线之一。
Fenton等应用严格的纳入标准,此应用可将胎儿和婴儿尺寸数据转换为早产儿胎儿-婴儿生长图的最佳數据。
研究者认为Fenton 2013这个生长图表,因为数据是从发达国家选择的,可以尽量减少可能不理想的环境对婴儿生长的影响,可能适用于发达国家和发展中国家的早产儿。
这也是目前临床最常使用的早产儿生长评估曲线【4】。
1.2 Intergrowth 2015该曲线于2015年公布,是根据世界卫生组织INTERGROWTH-21计划的研究结果所得出的早产儿出生后生长的数据。
该计划是在全球八个地方进行的、以多中心人口为基础的研究,评估了这八个地区的胎儿、新生儿和产后生长情况。
然而,虽然是全球多中心研究,其纳入的样本量较小,参与研究的4607名女性中,仅有224名是早产单胎,其中201名(90%)参加了早产产后随访研究。
且该研究限定的早产为怀孕26周至37周之前出生的单胎,对更小出生胎龄的早产儿没有提供相应数据【5】。
中国婴幼儿生长曲线

中国婴幼儿生长曲线
摘要:
I.引言
- 介绍中国婴幼儿生长曲线的概念
- 强调生长曲线对于婴幼儿健康的重要性
II.生长曲线的标准
- 介绍世界卫生组织(WHO)和中国卫生部门制定的生长曲线标准
- 解释生长曲线的三个关键指标:身高、体重、头围
III.生长曲线的应用
- 说明生长曲线在医疗、教育、科研等领域的应用
- 介绍生长曲线对于婴幼儿营养状况的评估作用
IV.生长曲线的重要性
- 强调生长曲线对于婴幼儿健康成长的指导意义
- 提醒家长和监护人关注婴幼儿生长曲线,确保孩子健康成长
V.结论
- 总结中国婴幼儿生长曲线的相关知识
- 呼吁全社会关注婴幼儿健康,共同努力提高婴幼儿的生活质量
正文:
中国婴幼儿生长曲线,作为衡量婴幼儿生长发育的重要工具,越来越受到家长和监护人的关注。
