克唑替尼说明书
赛可瑞克唑替尼胶囊服用方法和饮食禁忌
辉瑞赛可瑞克唑替尼(Xalkori)服用方法和饮食禁忌本文由印康源海外医疗整理提供,辉瑞研发的赛可瑞克唑替尼胶囊是Met/ALK/ROS的ATP竞争性的多靶点蛋白激酶抑制剂,主要用于治疗间变性淋巴瘤激酶(ALK)阳性的局部晚期或转移性非小细胞肺癌(NSCLC)。
辉瑞面向印度市场,开发了品牌名称为Crizalk的印度版克唑替尼,另外还有印度本地品牌的克唑替尼(微信:yinkangyuan88)。
不论是哪个版本的克唑替尼,在开始治疗之前和服用过程中都有一些注意事项。
在开始治疗之前,医生可能会进行测试,以确保克唑替尼是您的肺癌类型的最佳治疗。
服用方法剂量和时间需医生处方。
不要加大或者减少药量或超过推荐的时间。
克唑替尼的推荐剂量为250mg,每天服用两次可以带食物或者不带食物服用不要粉碎,咀嚼,溶解或打开克唑替尼胶囊,整个吞下为了确保这种药物对病情有帮助,而且不会造成有害影响,血细胞和肝功能可能需要经常检测。
心脏功能可能需要使用心电图(ECG或EKG)进行测试。
根据这些测试的结果,癌症治疗可能会延迟未经医生允许,不要停止服用药物在室温下储存,远离湿气和热量,不用时请将瓶子盖紧。
如果忘记服用克唑替尼,如果记起,尽快服用,但是如果距离下次用药已经不足6小时,那么忽略掉这一次用药,按照正常药量和用药时间服药。
尽量避免在治疗期间进食葡萄柚和西柚汁。
有些药物可能会与克唑替尼产生相互作用。
华法林(Coumadin,Jantoven)等血液稀释剂环孢素(Gengraf,Neoral,Sandimmune),西罗莫司(Rapamune)或他克莫司(Prograf)地塞米松(Cortastat,Dexasone,Solurex,DexPak)地高辛(洋地黄,Lanoxin,Lanoxicaps)异烟肼(用于治疗结核病)尼卡地平(Cardene)匹莫齐特(Orap)圣约翰草茶碱(Elixophyllin,Theo-24,Theochron,Uniphyl)红霉素(E.E.S.,EryPed,Ery-Tab,Erythrocin,Pediazole),利福布丁(Mycobutin),利福平(Rifadin,Rifater,Rifamate),利福喷汀(Priftin)或泰利霉素(Ketek)去甲丙咪嗪(Norpramin),多塞平(Sinequan,Silenor),艾司西酞普兰(Lexapro),米氮平(Remeron),奈法唑酮,舍曲林(Zoloft),曲唑酮(Desyrel,Oleptro),三甲吡啶(Surmontil)或文拉法辛(Effexor)如伊曲康唑(Sporanox),酮康唑(Nizoral),咪康唑(Oravig)或伏立康唑(Vfend)等抗真菌药物司可巴比妥(Seconal),戊巴比妥(Nembutal)或苯巴比妥(Solfoton)等巴比妥类麦角胺(Ergomar,Cafergot)或二氢麦角胺(D.H.E.45,Migranal鼻喷雾剂)普鲁卡因胺(Procan,Pronestyl)或奎尼丁(Quin-G)等心脏节律药物阿扎那韦(Reyataz),地拉呋啶(Delavirdine),依非韦伦(Efavirenz),依地韦林(Etivirenz),依地韦林(Etravirine),茚地那韦(Crixivan),奈非那韦(Viracept),奈韦拉平(Viramune),利托那韦(Norvir,Kaletra)或沙奎那韦(Invirase)非氨酯(Felbatol),奥卡西平(Trileptal),苯妥英(Dilantin),扑米酮(Mysoline)或丙戊酸(Depakene,Stavzor)以上未列出所有可能与克唑替尼产生相互作用的药物,还有许多其他药物可以与克唑替尼相互作用。
克唑替尼(赛可瑞)用药手册(中文版)

所有的药物都可能有副作用,然而很多患者不会经历副作用或者只有轻微副作用。如果它们 引起您的顾忌或长时间不减轻,请咨询您的医生或就诊。
• 劳累,虚弱• 味觉改变• 腹痛• 胃部不适或呕吐• 便秘• 腹泻• 无饥饿感• 鼻、喉部刺激 感• 流鼻涕、打喷嚏• 体重下降或增加• 肌肉痉挛• 头痛
我怎么保存这个药物?
• 室温保存 • 干燥保存 • 请将药物放在儿童和宠物够不到的地方
其他注意事项?
• 如果您的症状和疾病不好转或加重,请咨询您的医生。 • 严禁将您的药物分享给他人或服用他人的药物 • 建议将您在服用的所有药物(包括保健品)列一张清单,看病时给医生作参考 • 如果您要服用任何药品和保健品,请先咨询您的医生
说明:目前,印度有非常便宜的克挫替尼,可以找正规的海外医疗公司通过正规渠道获取, 在国内做的比较早的是康安途海外医疗。
这个药物怎么服用?
• 坚持遵医嘱服药,勿私自改变剂量。 • 为保证最优药效,请勿漏服药物。 • 空腹或和食物一起服用皆可。 • 整粒药吞服,不能咀嚼、磨碎、切开药物。 • 如果服药后呕吐,不要马上再吃一次,按照正常的下一次服药时间服药。
如果我忘记服药了怎么办?
• 如果刚过服药时间不久,可以在想起来的时候马上服药。 • 如果距离下一次服药时间不到 6 小时,那么就直接跳过忘记服药的那一天,继续服药。 • 请勿为了补忘记服的药物一次吃两片或多片药。
出现以下情况,请立即通知您的医生或赴急诊就医:
警告:药物严重副作用虽然很少见,但是您如果在服药期间出现下列副作用,它们可能是非 常严重甚至危及生命的,请务必咨询医生或立即就医。 • 出现过敏反应(包括皮疹,风团,瘙痒,呼吸困难,咳嗽,眼睛或面部水肿,喉头水肿, 休克等)
克唑替尼原理

克唑替尼原理
克唑替尼是一种针对ALK阳性的非小细胞肺癌( NSCLC)的靶向治疗药物。
它的原理是通过抑制ALK融合基因所编码的酪氨酸激酶的活性,从而阻断肿瘤细胞的增殖和侵袭。
克唑替尼在2011年获得美国FDA的批准,用于治疗晚期或转移性的ALK阳性NSCLC,是第一个针对ALK的靶向药物。
多项临床试验表明,克唑替尼相比传统的化疗,能够显著提高ALK阳性NSCLC 患者的客观缓解率、无进展生存期和总生存期,同时具有较好的耐受性和安全性。
然而,克唑替尼并非万能的,它也存在一些不良反应和局限性。
最重要的问题就是耐药,即患者在使用克唑替尼一段时间后,肿瘤细胞会发生一些变化,使得克唑替尼失去了原有的抑制作用,导致疾病的恶化或复发。
目前已知的耐药机制主要有以下几种:
-(ALK二级突变:指ALK融合基因的酪氨酸激酶结构域内发生的导致氨基酸替换的点突变,使得ALK融合蛋白对克唑替尼的亲和力降低或失去,从而降低克唑替尼的抑制效果。
-(ALK基因扩增:指ALK融合基因在染色体上的拷贝数增加,导致ALK融合蛋白的表达水平升高,从而抵消克唑替尼的抑制作用。
-(躲避信号通路的激活:指肿瘤细胞通过激活其他与ALK信号
通路平行或下游的信号通路,如EGFR、KRAS、PI3K/AKT、MAPK等,来维持细胞的增殖和存活,从而规避克唑替尼的抑制作用。
-(肿瘤微环境的改变:指肿瘤细胞周围的血管、基质、免疫细胞等发生的变化,影响克唑替尼的药物输送、代谢和效应,从而降低克唑替尼的治疗效果。
克唑替尼说明书

_______________________________________________________________________________________________________________________________________ _______________________________________________________________________________________________________________________________________ HIGHLIGHTS OF PRESCRIBING INFORMATION •QTInterval Prolongation: Occurred in 2.7% of patients. Monitor with These highlights do not include all the information needed to use electrocardiograms and electrolytes in patients who have a history of orXALKORI ®safely and effectively. See full prescribing information for predisposition for QTc prolongation, or who are taking medications that XALKORI. prolong QT. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (5.3) XALKORI ® (crizotinib) Capsules, oral • Bradycardia: XALKORI can cause bradycardia. Monitor heart rate and Initial U.S. Approval: 2011blood pressure regularly. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (5.4) ----------------------------INDICATIONS AND USAGE---------------------------•Embryofetal Toxicity: XALKORI can cause fetal harm when XALKORI is a kinase inhibitor indicated for the treatment of patients with administered to a pregnant woman. (5.5, 8.1) metastatic non-small cell lung cancer (NSCLC)whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test. (1)------------------------------ADVERSE REACTIONS-------------------------------The most common adverse reactions (≥25%) are vision disorders, nausea, ----------------------DOSAGE AND ADMINISTRATION-----------------------diarrhea, vomiting, constipation, edema, elevated transaminases, and fatigue. •Recommended dose: 250 mg orally, twice daily (2.2) (6) • Renal Impairment: 250 mg orally,once daily in patients with severe renal impairment (creatinine clearance <30 mL/min) not requiringTo report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. atdialysis. (2.2)1-800-438-1985 or FDA at 1-800-FDA-1088 or /medwatch . •Dosing interruption and/or dose reductions may be required based on adverse drug reactions. (2.3)------------------------------DRUG INTERACTIONS-------------------------------• CYP3AInhibitors: Avoid concurrent use of XALKORI with strong ---------------------DOSAGE FORMS AND STRENGTHS----------------------CYP3A inhibitors. (7.1)• Capsules: 250 mg and 200 mg (3) • CYP3AInducers: Avoid concurrent use of XALKORI with strong CYP3A inducers. (7.2)-------------------------------CONTRAINDICATIONS------------------------------• CYP3A Substrates: Avoid concurrentuse of XALKORI with CYP3A • None (4) substrates with narrow therapeutic indices. (7.3)See 17 forPATIENT COUNSELING INFORMATION and FDA------------------------WARNINGS AND PRECAUTIONS------------------------• Hepatotoxicity: Fatal hepatotoxicity occurred in 0.2% of patients. approved patient labeling.Monitor with periodic liver testing. Temporarily suspend, dose reduce, or permanently discontinue XALKORI. (5.1) Revised: 03/2015• Interstitial Lung Disease (ILD)/Pneumonitis: Occurred in 2% of patients. Permanently discontinue in patients with ILD/pneumonitis. (5.2)FULL PRESCRIBING INFORMATION: CONTENTS*8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy 8.3 Nursing Mothers 1 INDICATIONS AND USAGE8.4 Pediatric Use 2 DOSAGE AND ADMINISTRATION8.5 Geriatric Use 2.1Patient Selection 8.6 Hepatic Impairment 2.2Recommended Dosing 8.7 Renal Impairment 2.3Dose Modification 10 OVERDOSAGE 3DOSAGE FORMS AND STRENGTHS 11 DESCRIPTION 4CONTRAINDICATIONS 12 CLINICAL PHARMACOLOGY 5 WARNINGS AND PRECAUTIONS12.1 Mechanism of Action 5.1Hepatotoxicity 12.2 Pharmacodynamics 5.2Interstitial Lung Disease (Pneumonitis) 12.3 Pharmacokinetics 5.3QT Interval Prolongation 5.4Bradycardia 13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility 5.5 Embryofetal Toxicity 14 CLINICAL STUDIES 6 ADVERSE REACTIONS 6.1 Clinical Trials Experience 16 HOW SUPPLIED/STORAGE AND HANDLING 17 PATIENT COUNSELING INFORMATION 7 DRUG INTERACTIONS 7.1 Drugs That May Increase Crizotinib Plasma Concentrations * Sections or subsections omitted from the Full Prescribing Information are 7.2 Drugs That May Decrease Crizotinib Plasma Concentrations not listed. 7.3 Drugs Whose Plasma Concentrations May Be Altered By CrizotinibFULL PRESCRIBING INFORMATION1 INDICATIONS AND USAGEXALKORI is indicated for the treatment of patients with metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test.2 DOSAGE AND ADMINISTRATION2.1 Patient SelectionSelect patients for the treatment of metastatic NSCLC with XALKORI based on the presence of ALK positivity in tumor specimens [see Indications and Usage (1) and Clinical Studies (14)]. Information on FDA-approved tests for the detection of ALK rearrangements in NSCLC is available at/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm301431.htm.2.2 Recommended DosingThe recommended dose of XALKORI is 250 mg orally, twice daily until disease progression or no longer tolerated by the patient. The recommended dose of XALKORI in patients with severe renal impairment (creatinine clearance <30 mL/min) not requiring dialysis is 250 mg orally, once daily [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].XALKORI may be taken with or without food. Swallow capsules whole. If a dose of XALKORI is missed, make up that dose unless the next dose is due within 6 hours. If vomiting occurs after taking a dose of XALKORI, take the next dose at the regular time.2.3 Dose ModificationReduce dose as below, if one or more dose reductions are necessary due to adverse reactions of Grade 3 or 4 severity, as defined by NCI Common Terminology Criteria for Adverse Events (CTCAE) version 4.0: •First dose reduction: XALKORI 200 mg taken orally twice daily•Second dose reduction: XALKORI 250 mg taken orally once daily•Permanently discontinue if unable to tolerate XALKORI 250 mg taken once dailyDose reduction guidelines are provided in Tables 1 and 2.Table 1. XALKORI Dose Modification – Hematologic Toxicities aCTCAE Grade XALKORI DosingGrade 3 Withhold until recovery to Grade 2 or less, then resume at the same dose scheduleGrade 4 Withhold until recovery to Grade 2 or less, then resume at next lower dosea Except lymphopenia (unless associated with clinical events, e.g., opportunistic infections).Table 2. XALKORI Dose Modification – Non-Hematologic ToxicitiesCriteria XALKORI DosingAlanine aminotransferase (ALT) or aspartate Withhold until recovery to baseline or less than or equal to 3 times aminotransferase (AST) elevation greater ULN, then resume at reduced dosethan 5 times upper limit of normal (ULN)with total bilirubin less than or equal to1.5 times ULNALT or AST elevation greater than 3 times ULN with concurrent total bilirubin elevation greater than 1.5 times ULN (in the absence of cholestasis or hemolysis) Permanently discontinueAny Grade drug-related interstitial lung disease/pneumonitis Permanently discontinueQTc greater than 500 ms on at least 2 separate ECGs Withhold until recovery to baseline or to a QTc less than 481 ms, then resume at reduced doseQTc greater than 500 ms or greater than or equal to 60 ms change from baseline with Torsade de pointes or polymorphic ventricular tachycardia or signs/symptoms of serious arrhythmia Permanently discontinueBradycardia a (symptomatic, may be severe and medically significant, medical intervention indicated) Withhold until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or aboveEvaluate concomitant medications known to cause bradycardia, as well as anti-hypertensive medicationsIf contributing concomitant medication is identified and discontinued, or its dose is adjusted, resume at previous dose upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or aboveIf no contributing concomitant medication is identified, or if contributing concomitant medications are not discontinued or dose modified, resume at reduced dose upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or aboveBradycardia a,b (life-threatening consequences, urgent intervention indicated) Permanently discontinue if no contributing concomitant medication is identifiedIf contributing concomitant medication is identified and discontinued, or its dose is adjusted, resume at 250 mg once daily upon recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, with frequent monitoringab Permanently discontinue for recurrence.Monitor complete blood counts including differential white blood cell counts monthly and as clinically indicated, with more frequent repeat testing if Grade 3 or 4 abnormalities are observed, or if fever or infection occurs.3 DOSAGE FORMS AND STRENGTHS250 mg capsulesHard gelatin capsule, size 0, pink opaque cap and body, with “Pfizer” on the cap and “CRZ 250” on the body.200 mg capsulesHard gelatin capsule, size 1, white opaque body and pink opaque cap, with “Pfizer” on the cap and “CRZ 200” on the body.4 CONTRAINDICATIONSNone5 WARNINGS AND PRECAUTIONS5.1 HepatotoxicityDrug-induced hepatotoxicity with fatal outcome occurred in 2 (0.2%) of the 1225 patients treated with XALKORI across three main clinical trials. Concurrent elevations in alanine aminotransferase (ALT) greater than three times the upper limit of normal and total bilirubin greater than two times the upper limit of normal, with normal alkaline phosphatase, occurred in 7 patients (0.6%). Additionally, elevations in ALT greater than five times the upper limit of normal occurred in 109 patients (9.2%). Eight patients (0.7%) required permanent discontinuation due to elevated transaminases. These laboratory findings were generally reversible upon dosing interruption. Transaminase elevations generally occurred within the first 2 months of treatment.Monitor with liver function tests including ALT and total bilirubin every 2 weeks during the first 2 months of treatment, then once a month and as clinically indicated, with more frequent repeat testing for increased liver transaminases, alkaline phosphatase, or total bilirubin in patients who develop transaminase elevations. Temporarily suspend, dose reduce, or permanently discontinue XALKORI as described in Table 2 [see Dosage and Administration (2.3) and Adverse Reactions (6)].5.2 Interstitial Lung Disease (Pneumonitis)Severe, life-threatening, or fatal interstitial lung disease (ILD)/pneumonitis can occur in patients treated with XALKORI. Across clinical trials (n=1225), 31 XALKORI-treated patients (2.5%) had any grade ILD,11 patients (0.9%) had Grade 3 or 4, and 6 patients (0.5%) had fatal cases. These cases generally occurred within 2 months after the initiation of treatment.Monitor patients for pulmonary symptoms indicative of ILD/pneumonitis. Exclude other potential causes of ILD/pneumonitis, and permanently discontinue XALKORI in patients diagnosed with drug-relatedILD/pneumonitis [see Dosage and Administration (2.3) and Adverse Reactions (6)].5.3 QT Interval ProlongationQTc prolongation can occur in patients treated with XALKORI. Across clinical trials (n=1225), QTc prolongation (all grades) was observed in 34 (2.7%) patients and QTc greater than 500 ms on at least 2 separate ECGs occurred in 17 (1.4%) patients.Avoid use of XALKORI in patients with congenital long QT syndrome. Consider periodic monitoring with electrocardiograms (ECGs) and electrolytes in patients with congestive heart failure, bradyarrhythmias, electrolyte abnormalities, or who are taking medications that are known to prolong the QT interval. Permanently discontinue XALKORI in patients who develop QTc greater than 500 ms or greater than or equal to 60 ms change from baseline with Torsade de pointes or polymorphic ventricular tachycardia orsigns/symptoms of serious arrhythmia. Withhold XALKORI in patients who develop QTc greater than 500 ms on at least 2 separate ECGs until recovery to a QTc less than or equal to 480 ms, then resume XALKORI at a reduced dose as described in Table 2 [see Dosage and Administration (2.3) and Clinical Pharmacology (12.2)].5.4 BradycardiaSymptomatic bradycardia can occur in patients receiving XALKORI. Across clinical trials, bradycardia with a heart rate less than 50 beats per minute occurred in 11% of 1174 patients treated with XALKORI. In Study 1, Grade 3 syncope occurred in 2.9% of XALKORI-treated patients and in none of the chemotherapy-treated patients.Avoid using XALKORI in combination with other agents known to cause bradycardia (e.g., beta-blockers, non-dihydropyridine calcium channel blockers, clonidine and digoxin) to the extent possible. Monitor heart rate and blood pressure regularly. In cases of symptomatic bradycardia that is not life-threatening, hold XALKORI until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, re-evaluate the use of concomitant medications, and adjust the dose of XALKORI. Permanently discontinue for life-threatening bradycardia due to XALKORI; however, if associated with concomitant medications known to cause bradycardia or hypotension, hold XALKORI until recovery to asymptomatic bradycardia or to a heart rate of 60 bpm or above, and if concomitant medications can be adjusted or discontinued, restart XALKORI at 250 mg once daily with frequent monitoring [see Dosage and Administration (2.3) and Adverse Reactions (6)].5.5 Embryofetal ToxicityXALKORI can cause fetal harm when administered to a pregnant woman based on its mechanism of action. In nonclinical studies in rats, crizotinib was embryotoxic and fetotoxic at exposures similar to those observed in humans at the recommended clinical dose of 250 mg twice daily. There are no adequate and well-controlled studies in pregnant women using XALKORI. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus [see Use in Specific Populations (8.1)].6 ADVERSE REACTIONSThe following adverse reactions are discussed in greater detail in other sections of the labeling: •Hepatotoxicity [see Warnings and Precautions (5.1)]•Interstitial Lung Disease/Pneumonitis [see Warnings and Precautions (5.2)]•QT Interval Prolongation [see Warnings and Precautions (5.3)]•Bradycardia [see Warnings and Precautions (5.4)]6.1 Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.Safety evaluation of XALKORI is based on more than 1200 patients with ALK-positive metastatic NSCLC who received XALKORI as monotherapy at a starting oral dose of 250 mg twice daily continuously.The most common adverse reactions (≥25%) of XALKORI are vision disorder, nausea, diarrhea, vomiting, constipation, edema, elevated transaminases, and fatigue.ALK-positive metastatic NSCLC-Study 1The data in Table 3 are derived from 343 patients with ALK-positive metastatic NSCLC enrolled in a randomized, multicenter, active-controlled, open-label trial (Study 1). Patients in the XALKORI arm (n=172) received XALKORI 250 mg orally twice daily until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. A total of 171 patients in the chemotherapy arm received pemetrexed 500 mg/m2 (n=99) or docetaxel 75 mg/m2 (n=72) by intravenous infusion every three weeks until documented disease progression, intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. Patients in the chemotherapy arm received pemetrexed unless they had received pemetrexed as part of first-line or maintenance treatment.The median duration of study treatment was 7.1 months for patients who received XALKORI and 2.8 months for patients who received chemotherapy. Across the 347 patients who were randomized to study treatment (343 received at least one dose of study treatment), the median age was 50 years; 84% of patients in the XALKORI arm and 87% of patients in the chemotherapy arm were younger than 65 years. A total of 57% of patients on XALKORI and 55% of chemotherapy patients were female. Forty-six percent (46%) of XALKORI-treated and 45% of chemotherapy-treated patients were from Asia.Serious adverse reactions were reported in 64 patients (37.2%) treated with XALKORI and 40 patients (23.4%) in the chemotherapy arm. The most frequent serious adverse reactions reported in patients treated with XALKORI were pneumonia (4.1%), pulmonary embolism (3.5%), dyspnea (2.3%), and interstitial lung disease (ILD; 2.9%). Fatal adverse reactions in XALKORI-treated patients in Study 1 occurred in 9 (5%) patients, consisting of: acute respiratory distress syndrome, arrhythmia, dyspnea, pneumonia, pneumonitis, pulmonary embolism, ILD, respiratory failure, and sepsis.Dose reductions due to adverse reactions were required in 16% of XALKORI-treated patients. The most frequent adverse reactions that led to dose reduction in the patients treated with XALKORI were alanine aminotransferase (ALT) elevation (7.6%) including some patients with concurrent aspartate aminotransferase (AST) elevation, QTc prolongation (2.9%), and neutropenia (2.3%).Discontinuation of therapy in XALKORI-treated patients for adverse reactions was 17.0%. The most frequent adverse reactions that led to discontinuation in XALKORI-treated patients were ILD (1.7%), ALT and AST elevation (1.2%), dyspnea (1.2%), and pulmonary embolism (1.2%). Tables 3 and 4 summarize common Adverse Reactions and Laboratory Abnormalities in XALKORI-treated patients.Table 3. Adverse Reactions Reported at a Higher Incidence (≥5% Higher for All Grades or ≥2% Higher for Grades 3/4) with XALKORI than Chemotherapy in Study 1 Adverse Reaction XALKORI (N=172) Chemotherapy (Pemetrexed or Docetaxel) (N=171) All Grades (%) Grade 3/4 (%) All Grades (%) Grade 3/4 (%) Nervous System Disorder Dizziness aDysgeusia Syncope 22 26 3 1 0 3 8 9 0 0 0 0 Eye Disorders Vision disorder b60 0 9 0 Cardiac Disorders Electrocardiogram QT prolonged Bradycardia c5 5 3 0 0 0 0 0 Investigations Weight decreased 10 1 4 0 Gastrointestinal Disorders Vomiting Nausea Diarrhea Constipation Dyspepsia 47 55 60 42 8 1 1 0 2 0 18 37 19 23 3 0 1 1 0 0 Infections and Infestations Upper respiratory infection d 26 0 13 1 Respiratory, Thoracic and Mediastinal Disorders Pulmonary embolism e 6 5 2 2 General Disorders and Administration Site Conditions Edemaf 31 0 16 0 Includes cases reported within the clustered terms:aDizziness (Balance disorder, Dizziness, Dizziness postural) bVision Disorder (Diplopia, Photophobia, Photopsia, Vision blurred, Visual acuity reduced, Visual impairment, Vitreous floaters) cBradycardia (Bradycardia, Sinus bradycardia) dUpper respiratory infection (Laryngitis, Nasopharyngitis, Pharyngitis, Rhinitis, Upper respiratory tract infection) ePulmonary embolism (Pulmonary artery thrombosis, Pulmonary embolism) fEdema (Face edema, Generalized edema, Local swelling, Localized edema, Edema, Edema peripheral, Periorbital edema) Additional adverse reactions occurring at an overall incidence between 1% and 30% in patients treated with XALKORI included decreased appetite (27%), fatigue (27%), neuropathy (19%; dysesthesia, gait disturbance, hypoesthesia, muscular weakness, neuralgia, peripheral neuropathy, parasthesia, peripheral sensory neuropathy, polyneuropathy, burning sensation in skin), rash (9%), ILD (4%; acute respiratory distress syndrome, ILD, pneumonitis), renal cyst (4%), and hepatic failure (1%).Table 4. Summary of Treatment-Emergent Laboratory Abnormalities with Grade 3 or 4 Incidence of≥4% in XALKORI-Treated Patients Laboratory Abnormality CrizotinibAny Grade Grade 3/4 ChemotherapyAny Grade Grade 3/4HematologyNeutropeniaLymphopenia 49%51%12%9%28%60%12%25%ChemistryALT elevationAST elevationHypokalemiaHypophosphatemia 76%61%18%28%17%9%4%5%38%33%10%25%4%0%1%6%ALK-positive metastatic NSCLC-Study 2The safety analysis population in Study 2 included 934 patients with ALK-positive metastatic NSCLC who received XALKORI in a clinical trial. The median duration of treatment was 23 weeks. Dosing interruptions and reductions due to treatment-related adverse events occurred in 23% and 12% of patients, respectively. The rate of treatment-related adverse events resulting in permanent discontinuation was 5%. The most common adverse reactions (≥25%) included vision disorder (55%), nausea (51%), vomiting (46%), diarrhea (46%), edema (39%), constipation (38%), and fatigue (26%).Description of selected adverse drug reactionsVision disordersVision disorders, most commonly visual impairment, photopsia, blurred vision, or vitreous floaters, occurred in 691 (56%) patients across clinical trials (n=1225). The majority (99%) of these patients had Grade 1 or 2 visual adverse reactions. Across clinical studies, one patient had a treatment-related grade 3 vision abnormality.Based on the Visual Symptom Assessment Questionnaire (VSAQ-ALK), patients treated with XALKORI in Study 1 reported a higher incidence of visual disturbances compared to patients treated with chemotherapy. The onset of vision disorders generally started within the first week of drug administration. The majority of patients on the XALKORI arm in Study 1 (> 50%) reported visual disturbances; these visual disturbances occurred at a frequency of 4-7 days each week, lasted up to 1 minute, and had mild or no impact (scores 0 to 3 out of a maximum score of 10) on daily activities as captured in a patient questionnaire.NeuropathyNeuropathy, most commonly sensory in nature, occurred in 235 (19%) of 1225 patients. Most events (95%) were Grade 1 or Grade 2 in severity.Renal CystsRenal cysts occurred in 7 (4%) patients treated with XALKORI and 1 (1%) patient treated with chemotherapy in Study 1. The majority of renal cysts in XALKORI-treated patients were complex. Local cystic invasion beyond the kidney occurred, in some cases with imaging characteristics suggestive of abscess formation. However, across clinical trials no renal abscesses were confirmed by microbiology tests.7 DRUG INTERACTIONS7.1 Drugs That May Increase Crizotinib Plasma ConcentrationsCoadministration of crizotinib with strong CYP3A inhibitors increases crizotinib plasma concentrations [see Clinical Pharmacology (12.3)]. Avoid concomitant use of strong CYP3A inhibitors, including but not limited toatazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, troleandomycin, and voriconazole. Avoid grapefruit or grapefruit juice which may also increase plasma concentrations of crizotinib. Exercise caution with concomitant use of moderate CYP3A inhibitors.7.2 Drugs That May Decrease Crizotinib Plasma ConcentrationsCoadministration of crizotinib with strong CYP3A inducers decreases crizotinib plasma concentrations [see Clinical Pharmacology (12.3)]. Avoid concomitant use of strong CYP3A inducers, including but not limited to carbamazepine, phenobarbital, phenytoin, rifabutin, rifampin, and St. John’s Wort.7.3 Drugs Whose Plasma Concentrations May Be Altered By CrizotinibCrizotinib inhibits CYP3A both in vitro and in vivo [see Clinical Pharmacology (12.3)]. Avoid concomitant use of CYP3A substrates with narrow therapeutic range, including but not limited to alfentanil, cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus in patients taking XALKORI. If concomitant use of these CYP3A substrates with narrow therapeutic range is required in patients taking XALKORI, dose reductions of the CYP3A substrates may be required due to adverse reactions.8 USE IN SPECIFIC POPULATIONS8.1 PregnancyPregnancy Category D [see Warnings and Precautions (5.5)]XALKORI can cause fetal harm when administered to a pregnant woman based on its mechanism of action. There are no adequate and well-controlled studies of XALKORI in pregnant women. In nonclinical studies in rats, crizotinib was embryotoxic and fetotoxic at exposures similar to those observed in humans at the recommended clinical dose of 250 mg twice daily. Crizotinib was administered to pregnant rats and rabbits during organogenesis to study the effects on embryo-fetal development. Postimplantation loss was increased at doses ≥ 50 mg/kg/day (approximately 0.6 times the AUC at the recommended human dose) in rats. No teratogenic effects were observed in rats at doses up to the maternally toxic dose of 200 mg/kg/day (approximately 2.7 times the AUC at the recommended human dose) or in rabbits at doses of up to60 mg/kg/day (approximately 1.6 times the AUC at the recommended human dose), though fetal body weights were reduced at these doses.Advise women of childbearing potential to avoid becoming pregnant while receiving XALKORI. Women of childbearing potential who are receiving this drug, or partners of women of childbearing potential receiving this drug, should use adequate contraceptive methods during therapy and for at least 90 days after completing therapy. If this drug is used during pregnancy, or if the patient or their partner becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus.8.3 Nursing MothersIt is not known whether XALKORI is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from XALKORI, consider whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.8.4 Pediatric UseThe safety and efficacy of XALKORI in pediatric patients has not been established. Decreased bone formation in growing long bones was observed in immature rats at 150 mg/kg/day following once daily dosing for 28 days(approximately 5.4 times the AUC in adult patients at the recommended human dose). Other toxicities of potential concern to pediatric patients have not been evaluated in juvenile animals.8.5 Geriatric UseOf XALKORI treated patients in Study 1, 27 (16%) were 65 years or older, in Study 2, 152 (16%) were65 years or older, and in Study 3, 16 (13%) were 65 years or older. No overall differences in safety or effectiveness were observed between these patients and younger patients.8.6 Hepatic ImpairmentXALKORI has not been studied in patients with hepatic impairment. As crizotinib is extensively metabolized in the liver, hepatic impairment is likely to increase plasma crizotinib concentrations. Clinical studies excluded patients with AST or ALT greater than 2.5 x ULN, or greater than 5 x ULN, if due to liver metastases. Patients with total bilirubin greater than 1.5 x ULN were also excluded. Therefore, use caution in patients with hepatic impairment [see Clinical Pharmacology (12.3)].8.7 Renal ImpairmentNo starting dose adjustment is needed for patients with mild (creatinine clearance [CLcr] 60-89 mL/min) or moderate (CLcr 30-59 mL/min) renal impairment based on a population pharmacokinetic analysis.Increased exposure to crizotinib occurred in patients with severe renal impairment (CLcr <30 mL/min) not requiring dialysis. Administer XALKORI at a dose of 250 mg taken orally once daily in patients with severe renal impairment not requiring dialysis [see Dosage and Administration (2.2) and ClinicalPharmacology (12.3)].10 OVERDOSAGEThere have been no known cases of XALKORI overdose. There is no antidote for XALKORI.11 DESCRIPTIONXALKORI (crizotinib) is an oral receptor tyrosine kinase inhibitor. The molecular formula for crizotinib isC21 H22 C l2FN5O. The molecular weight is 450.34 Daltons. Crizotinib is described chemically as (R)-3-[1-(2,6-Dichloro-3-fluorophenyl)ethoxy]-5-[1-(piperidin-4-yl)-1H-pyrazol-4-yl]pyridin-2-amine.。
肺癌常用化疗药物

肺癌常用化疗药物目录肺癌常用化疗药物 (1)一、吉非替尼 (1)二、厄洛替尼 (2)三、埃克替尼 (3)四、马来酸阿法替尼 (4)五、奥希替尼 (6)六、克唑替尼 (6)七、贝伐珠单抗 (7)八、重组人血管内皮抑制素 (8)九、盐酸安罗替尼 (9)十、塞瑞替尼 (10)十一、纳武利尤单抗 (11)一、吉非替尼通用名:吉非替尼片制剂与规格:片剂:250mg适应证:EGFR基因具有敏感突变的局部晚期或转移性非小细胞肺癌(NSCLC)。
合理用药要点:1.用药前必须明确有经国家药品监督管理局批准的EGFR基因检测方法检测到的EGFR 敏感突变。
2.肿瘤组织和血液均可用于EGFR基因突变检测,但组织检测优先。
3.治疗期间因药物毒性不可耐受时,可在同一代药物之间替换,如疾病进展则不能在同一代药物之间替换。
4.治疗过程中影像学显示缓慢进展但临床症状未发生恶化的患者,可以继续使用原药物;发生局部进展的患者,可以继续使用原药物加局部治疗;对于快速进展的患者,建议改换为其他治疗方案。
5.用药期间必须注意常见的皮肤反应和腹泻;应特别注意间质性肺炎、肝脏毒性和眼部症状的发生。
6.避免与CYP3A4诱导剂(如,苯妥英、卡马西平、利福平、巴比妥类或圣约翰草)联合使用。
避免与CYP3A4酶抑制剂(如酮康唑、异烟肼)等联合使用,其联合使用可能导致血药浓度升高而增加不良反应。
服用华法林的患者应定期监测凝血酶原时间或INR的改变。
能显著且持续升高胃液pH值的药物有可能会降低吉非替尼的血药浓度,从而降低吉非替尼疗效。
※7.在某些肿瘤急症的情况下如脑转移昏迷或呼吸衰※注:本指导原则“合理用药要点”带※部分为特殊情况下的药物合理使用专家共识。
竭,在充分知情的情况下,对不吸烟的肺腺癌患者可考虑使用。
一旦病情缓解,必须补充进行EGFR突变的组织检测。
二、厄洛替尼通用名:盐酸厄洛替尼片制剂与规格:片剂:150mg适应证:EGFR基因具有敏感突变的局部晚期或转移性非小细胞肺癌(NSCLC)。
克唑替尼胶囊(赛可瑞)说明书

克唑替尼胶囊(赛可瑞)【规格】250mg、200mg【适应症】可用于经SFDA批准的检测方法确定的间变性淋巴瘤激酶(ALK)阳性的局部晚期或转移性非小细胞肺癌(NSCLC)患者的治疗。
【禁忌症】对本品有严重超敏反应者禁用。
【用法用量】推荐剂量为250mg口服,每日两次。
胶囊应整粒吞服。
克唑替尼胶囊与食物同服或不同服均可。
若漏服一剂克唑替尼胶囊,则补服漏服剂量的药物,除非距下次服药时间短于6小时。
【不良反应】1、视觉异常:包括视觉损害、闪光感、视物模糊、玻璃体浮游物、畏光和复视。
上述不良事件通常在给药后两周内开始发生。
若患者出现闪光感或首次出现玻璃体浮游物或加重时,应考虑进行眼科检查。
2、心脏异常:心动过缓,也观察到QTc延长。
3、肾脏损伤:发生复杂性肾囊肿。
4、实验室检查异常:中性粒细胞减少、血小板减少和淋巴细胞减少。
5、消化道反应:消化不良、吞咽困难、上腹部不适,疼痛,烧灼感、食管炎、食管梗阻,溃疡、胃食管反流、吞咽疼痛和反流性食管炎。
6、全身异常:水肿,局部水肿和外周水肿。
7、神经系统:感觉迟钝、感觉过敏、感觉减退、神经痛、感觉异常、周围神经病变、外周运动神经病变和外周感觉神经病变。
【注意事项】1.根据不同患者安全性与耐受性可中断治疗或减少剂量。
如需减少剂量,则降低克唑替尼胶囊至200mg口服,每日两次。
若需要进一步减少剂量,则根据患者安全性和耐受性将剂量调整为250mg口服,每日一次。
2.育龄妇女在服用克唑替尼胶囊进行治疗时应尽量避免怀孕。
3.定期检查肝功能。
包括ALT和总胆红素,每月至少应检测一次,并且根据临床状况对氨基转移酶水平升高的患者更频繁地进行重复检测肝氨基转移酶、碱性磷酸酶或总胆红素升高水平。
在出现不良反应时进行减量或中断给药。
4.观测到QTc间期延长。
先天性长QT综合征患者应避免服用克唑替尼胶囊。
对于充血性心力衰竭、缓慢性心律失常和电解质异常患者,以及正在服用已知可致QT间期延长药物的患者,使用本品治疗时应定期监测其心电图与电解质。
克唑替尼胶囊说明书

克唑替尼胶囊说明书请仔细阅读说明书并在医师指导下使用【药品名称】通用名: 克唑替尼胶囊商品名: 赛可瑞®/XALKORI® 英文名: Crizotinib Capsules 汉语拼音: KeZuoTiNi JiaoNang 【成份】本品主要成份及其化学名称为:3-[(R)-1-(2,6-二氯-3-氟苯基)乙氧基]-5-[1-(哌啶-4-基)-1H-吡唑-4-基]吡啶-2-胺其结构式为:分子式:C21H22Cl2FN5O 分子量:450.3367【性状】本品为粉红色硬胶囊剂,内容物为白色结晶粉末。
【适应症】用于治疗间变性淋巴瘤激酶(ALK)阳性的局部晚期和转移的非小细胞肺癌(NSCLC)。
【规格】(1) 200 mg; (2) 250 mg;【用法用量】本品治疗ALK阳性的非小细胞肺癌晚期的推荐剂量是250mg,一次1粒,每日2次,早晚确定时间各服1粒,一天剂量为500mg,口服;整粒胶囊吞服,不可嚼碎服用,不可溶解服用,不可打开胶囊;与食物同服或不同服均可;不可与葡萄汁柚子汁一起服用。
剂量调整根据药物在个体中的安全性和耐受性情况,在医生的建议下调整剂量。
【不良反应】肝功能异常以下情况请马上联系你的主治医师:比平常更加疲惫,皮肤变黄,眼睛白色球变黄,尿液变暗或呈棕色(茶色);恶心,呕吐,食欲不振;胃部右侧疼痛;皮肤瘙痒,或比平时更容易擦伤;医生将进行血常规检测肝功能,如果检测指标不正常,医生会决定减小克唑替尼的剂量或者停止服用克唑替尼。
肺炎如果你感觉呼吸困难,咳嗽,发烧,请马上联系你的主治医师。
头晕,昏厥,胸部不适如果你发现心电图症状标识变化,或者心律不齐,请马上联系你的主治医师,医生会对你进行心电图检测,来观察克唑替尼治疗期间对身体的影响。
非常普遍的不良反应(可能大于10%)•肝功能异常•视觉效应(闪光,视力模糊,重影,一般在服用克唑替尼后不久就会出现)•神经病(神经麻痹,神经结合处,末端或者肌肉发麻)•头昏眼花,疲倦•水肿(身体组织积液,引起手足水肿)•肠胃不适(恶心,呕吐,腹泻,便秘,食道咽喉不适)•食欲不振,味觉减退•皮疹普遍的不良反应(1%~10%)•红细胞,白细胞,血小板减少•消化不良•心率降低不常见不良反应(0.1%~1%)•肾脏闭囊液【禁忌】对本品或药物的非活性成份严重过敏者禁用。
克唑替尼的作用机制和临床前数据-PPT精选文档
I期药代动力学数据: PROFILE 1001和PK研究
XALKORI® 包装说明书 Tan 等,编写稿
克唑替尼250 mg BID重复用药后的波谷浓度
1.000
Median Target Ceff (ALK) Target Ceff (c-MET)
800
600
400
200
0 0 20 40 60 80 100 120
永久扩增和凋亡抑制
克唑替尼抑制 EML4-ALK 融合蛋白
IC50低值提示在临床剂量可以有效抑制ALK
Pfizer, data on file
克唑替尼: 对EML4-ALK 细胞疗效的临床前证据
克唑替尼: 对H3122 细胞生长抑制和凋亡诱导
125 100 % control 75 50 25 0 –25 0.0001 0.01 –50 0.1 1 10 细胞 死亡
28 32
120
在黑暗中时间 (min)
与对照相比,克唑替尼治疗的大鼠的b波振幅起始下降,2小时后恢复正常
PR =光感受器层; ONL = 外核层 OPL = 外网织层; INL = 内核层 IPL = 内网织层; GL =神经节细胞层
Matsumoto et al., AACR 2019; Abs #4385
Cohort 1 (n=3) 50 mg QD
Cohort 2 (n=4) 100 mg QD
Cohort 3 (n=8) 200 mg QD
1 DLT: G3 ALT
Cohort 4 (n=7) 200 mg BID
Cohort 5 (n=6) 300 mg BID
2 DLTs: G3 疲劳
第1部分: 剂量递增 (n=37)
克唑替尼合理用药要点
克唑替尼合理用药要点
通用名:克唑替尼胶囊
制剂与规格:胶囊:200mg、250mg
适应证:
1.间变性淋巴瘤激酶(ALK)阳性的局部晚期或转移性非小细胞肺癌(NSCLC)患者的治疗。
2.ROS1阳性的晚期非小细胞肺癌(NSCLC)患者的治疗。
合理用药要点:
1.用药前必须明确有经国家药品监督管理局批准的ROS1或ALK 检测方法检测到的ROS1阳性或者ALK阳性。
2.治疗过程中影像学显示缓慢进展但临床症状未发生恶化的患者,可以继续使用原药物;发生局部进展的患者,可以继续使用原药物加局部治疗;对于快速进展的患者,建议改换为其他治疗方案。
3.用药期间必须注意常见的肝功能异常和视觉异常,治疗开始的最初两个月应每周检测一次,之后每月检测一次患者的肝功能,严重肝损伤患者禁用。
4.如果患者出现美国国立癌症研究所不良事件通用术语标准(NCICTCAE,第4.0版)规定的严重程度为3级或4级的不良事件,需一次或多次减少剂量,按以下方法减少剂量:(1)第一次减少剂量:口服,200mg,每日两次;(2)第二次减少剂量:口服,250mg,每日一次如果每日一次口服250mg克唑替尼胶囊仍无法耐受,则永久停服。
5.目前CYP3A抑制剂对稳态克唑替尼暴露量影响程度尚不确定。
克唑替尼是一种CYP3A的中度抑制剂。
体外研究表明,尽管克唑替尼是CYP2B6底物代谢的介导抑制剂,但在临床上不会发生药物相互作用。
6.用于cMET14外显子跳跃 NSCLC突变的晚期患者。
克唑替尼胶囊质量标准

克唑替尼胶囊质量标准克唑替尼胶囊是一种抗癌药物,被广泛应用于治疗某些类型的癌症,如非小细胞肺癌、胃肠道间质瘤等。
为了确保克唑替尼胶囊的质量和安全性,制定了一系列的质量标准。
克唑替尼胶囊的质量标准主要包括以下几个方面:1. 外观特征:克唑替尼胶囊应呈现出均匀的颜色、光滑的表面和一致的形状。
胶囊的尺寸应符合规定的要求,并且不得有明显的破损、变形或异物。
2. 标识和包装:每个克唑替尼胶囊应有清晰可辨的标识,包括药品名称、规格、批号、生产日期、有效期等信息。
药品的包装应符合相关法规要求,保证产品在运输和储存过程中不受损。
3. 质量控制:克唑替尼胶囊的含量应符合规定的要求。
药品中克唑替尼的含量应在一定范围内,确保药效的稳定性和一致性。
同时,还需要对药品进行微生物限度和重金属含量等方面的检测,确保产品符合卫生安全标准。
4. 纯度和杂质:克唑替尼胶囊中不得含有任何有害物质或杂质。
对于可能存在的杂质,如有机溶剂残留、重金属、微生物等,需要进行严格的检测和控制,确保药品的纯度和安全性。
5. 药效和安全性:克唑替尼胶囊在临床应用中应具有明确的药效,并且不会引起严重的不良反应。
药品的药效和安全性需要通过临床试验和监测来验证,并符合相关法规和标准。
6. 贮存和运输条件:克唑替尼胶囊在贮存和运输过程中需要符合一定的条件,如温度、湿度等。
药品在贮存和运输过程中需要避免受到阳光直射、高温、潮湿等不利因素的影响,以确保产品质量不受损。
以上是克唑替尼胶囊的质量标准要求,制定这些标准是为了保证药品的质量和安全性。
只有在严格按照这些标准进行生产和监控,才能确保患者获得高质量、有效和安全的治疗药物。
同时,监管部门也会对克唑替尼胶囊进行抽检和监督,以确保市场上销售的产品符合质量标准。
患者在使用克唑替尼胶囊时,也要按照医生的建议进行正确使用,以获得最佳的治疗效果。
癌症的个体化治疗—克唑替尼的研发与应用

P H A - 6 6 5 7 5 2与非磷酸化 ME T激酶域的共 晶结构设计而成的。2 一 氨基一 3 一 苄氧基吡啶系列化合物
可与非活性 ME T蛋白发生更有效的相互作用 ,并稳定其在非活化 自抑制构象 中,从而取得高的
细胞活性 。通过对先导化合物系列 进行优化 ,得到 临床候选药物克唑替尼 ( P F - 0 2 3 4 1 0 6 6 ) 。各
45
中国药理通讯 2 0 1 3 年第三十卷第二期
8 月2 6日 快速通道批准了克唑替尼在 A L K阳性晚期肺癌患者 中的使用 。同时 ,克唑替尼在临床
试 验 中显示 了多种 与其靶 点 紧密 相关 的抗 ห้องสมุดไป่ตู้瘤 活性 ,包 括 AL K 阳性 的 间变性 大细 胞淋 巴瘤 ;炎 性 肌纤 维母 细胞 性肿 瘤 ;神 经母 细胞 瘤 患 者 ;R OS阳性 的非 小 细 胞 肺 癌 患 者 ;以 及 存 在 ME T
而引起严重的毒副作用和降低人 的免疫能力。随着对肿瘤细胞 生物学 的深入研究 ,正常细胞与
肿瘤细胞复杂信号通路 的差异正在逐 渐地被 了解和揭示 。阻断肿瘤细胞特异 的信号通路从而达
到攻击肿瘤细胞 的高选择性 ,低毒性的分子靶 向治疗 ( mo l e c u l a r t a r g e t t h e r a p y )正在受到越来 越多 的关 注 。1 9 9 7年 选 择 性 作 用 于 人 类 表 皮 生 长 因 子 受 体 2 ( He r 2 ) 的 曲 妥 珠 单 抗 ( t r a s t u z u ma b )获批用于 He r 2 4 - 乳腺癌病人 ,以及 2 0 0 1 年 Ab l 蛋白激酶抑制剂伊马替尼获批用
炎症诱 发肿瘤 的机制探 索
克唑替尼中文说明书

克唑替尼说明书(中文)【药物名】Xalkori 【商品名】Crizotinib (克唑替尼) 【美国上市时间】o ROS-1阳性非小细胞肺癌;o FDA 批准的检测方法确定的间变性淋巴瘤激酶( ALK)阳性的局部晚期患者;上市时间:2011 年【类别】酪氨酸酶抑制剂【靶点】ALK【分子结构】分子式:C21H22C l2 FN5O化学名:(R)-3-[1-(2,6-Dichloro-3-fluorophenyl)ethoxy]-5-[1-(piperidin-4-yl)-1H-pyrazol-4-yl]pyridin-2-amine 结构式为:分子量为:450.34 KDa【生产公司】Pfizer 辉瑞公司【购买地】美国【剂型和规格】口服胶囊,剂量为250mg和200mg。
250mg胶囊:硬明胶胶囊,大小0,粉色不透明帽和体,在帽上有“ Pfizer ”和体上“ CRZ 250” ,60胶囊瓶:NDC 0069-8140-20。
200mg胶囊:硬明胶胶囊,大小1,白色不透明体和粉色不透明帽,帽上有“ Pfizer 和体上“ CRZ 200”,60胶囊瓶:NDC 0069-8141-20。
【本质】克唑替尼胶囊硬壳含250 mg 或200 mg 的克唑替尼胶体二氧化硅,微晶纤维素,无水磷酸氢钙,羟基乙酸淀粉钠,硬脂酸镁和硬胶囊胶囊壳为无活性成分。
粉红色不透明胶囊壳组分含明胶,二氧化钛,和氧化铁红。
白色不透明胶囊壳组分含明胶和二氧化钛。
印刷油墨含有虫胶,丙二醇,强氨水溶液,氢氧化钾,和黑色氧化铁。
【作用机理】克唑替尼是酪氨酸激酶受体包括ALK,肝细胞生长因子受体(HGFR, c-Met),ROS1(c-ros),和酪氨酸激酶(RON)的一种抑制剂。
易位可影响ALK基因导致致癌融合蛋白的表达。
ALK融合蛋白的形成导致激活和基因表达和增加细胞增殖有贡献信号的调节异常而生存肿瘤表达这些蛋白。
克唑替尼就是通过阻断对肿瘤细胞生长与存活起关键作用的多种细胞通路,导致肿瘤的稳定或消退。
药物Crizotinib(克唑替尼)合成检索总结报告
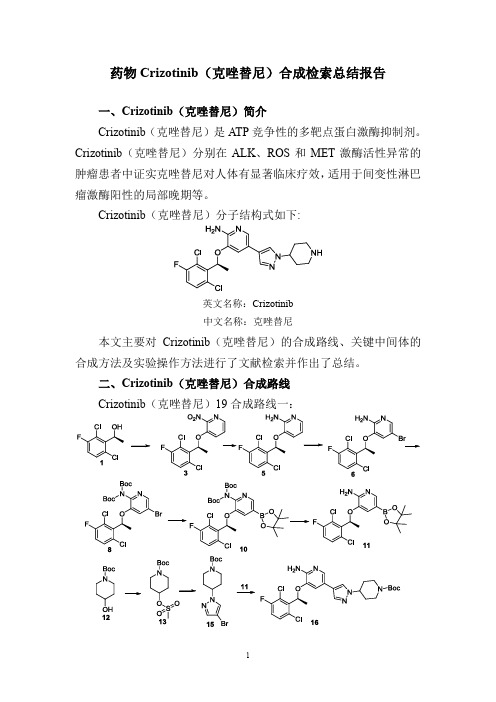
药物Crizotinib(克唑替尼)合成检索总结报告
一、Crizotinib(克唑替尼)简介
Crizotinib(克唑替尼)是ATP竞争性的多靶点蛋白激酶抑制剂。
Crizotinib(克唑替尼)分别在ALK、ROS和MET激酶活性异常的肿瘤患者中证实克唑替尼对人体有显著临床疗效,适用于间变性淋巴瘤激酶阳性的局部晚期等。
Crizotinib(克唑替尼)分子结构式如下:
英文名称:Crizotinib
中文名称:克唑替尼
本文主要对Crizotinib(克唑替尼)的合成路线、关键中间体的合成方法及实验操作方法进行了文献检索并作出了总结。
二、Crizotinib(克唑替尼)合成路线
Crizotinib(克唑替尼)19合成路线一:
Crizotinib(克唑替尼)19合成路线二:
三、Crizotinib(克唑替尼)合成检索总结报告(一) Crizotinib(克唑替尼)中间体3的合成方法一
(二) Crizotinib (克唑替尼)中间体3的合成方法二
(三) Crizotinib (克唑替尼)中间体5的合成
(四) Crizotinib(克唑替尼)中间体6的合成方法一。
抗肿瘤分子靶向药物致化疗相关性腹泻(完整版)
抗肿瘤分子靶向药物致化疗相关性腹泻(完整版)化疗相关性腹泻(CRD)可导致治疗效果和患者依从性降低,影响肿瘤患者的长期治疗结局,甚至危及生命。
除传统化疗药物外,许多分子靶向药物也可导致CRD,包括小分子表皮生长因子受体(EGFR)抑制剂、抗EGFR单克隆抗体、磷酸肌醇3-激酶抑制剂、血管内皮细胞生长因子受体小分子抑制剂、BCR-ABL1和KIT抑制剂、人表皮生长因子受体2靶点抑制剂、周期蛋白依赖性激酶抑制剂、抗体-药物偶联物等多种分子靶向药物。
其发生机制可能与分子靶向治疗药物引起肠黏膜损伤或肠炎等有关,临床表现为大便频率增加和/或松散不成形,患者常伴有产气过多和/或肠绞痛。
不同药物引起的CRD发生率不同,临床应重视病史采集和鉴别诊断,积极干预并进行动态评估,加强患者教育,以及时发现和预防肠毒性的发生。
CRD的临床表现初期症状:大便频率增加、大便松散不成形、产气过多、肠绞痛。
重度表现:频繁的水样便、大便中出现黏液或血液。
严重并发症:血容量不足、急性肾损伤、电解质紊乱(低钾血症、代谢性酸中毒、低钠血症或高钠血症)。
感染风险:肠粘膜破坏导致的感染、脓毒症风险增加(尤其在免疫抑制状态下)。
治疗:重度患者常需住院接受支持治疗。
结肠炎类型:中性粒细胞减少性、缺血性、艰难梭菌相关性、淋巴细胞结肠炎。
中性粒细胞减少性小肠结肠炎特点:常见于中性粒细胞绝对计数<500 个/uL的患者,右下腹痛,全身症状在接受化疗后第3周出现。
缺血性肠炎特点:用药后4-10天后发病,左腹部疼痛,24小时内出现直肠出血或血性腹泻。
艰难梭菌相关性腹泻特点:水泻样,24小时内稀便次数达3次以上,可能伴有肠梗阻。
淋巴细胞性结肠炎特点:使用阿柏西普治疗者可能发生,脐周阵发性疼痛,慢性水样便,需活检确认。
常见导致腹泻的分子靶向治疗药物1、小分子EGFR抑制剂药物:吉非替尼、厄洛替尼、阿法替尼、达可替尼和奥希替尼是常见的EGFR 酪氨酸激酶抑制剂。
重磅!克唑替尼Ⅲ期研究PROFILE1029试验研究结果揭晓

重磅!克唑替尼Ⅲ期研究PROFILE1029试验研究结果揭晓19号,在万众瞩目之下,辉瑞制药公布了克唑替尼的又一个大型Ⅲ期临床研究PROFILE 1029试验的结果。
PROFILE 1029研究达到了主要研究终点,研究结果证实了在东亚人群,克唑替尼一线治疗间变性淋巴瘤激酶(ALK)阳性晚期非小细胞肺癌(NSCLC)患者的疗效明显优于标准铂类药物为基础的化疗方案。
来源:肿瘤资讯背景克唑替尼国际多中心III期研究PROFILE1014试验已经证实了克唑替尼一线治疗ALK阳性晚期非小细胞肺癌患者的疗效明显优于标准铂类药物为基础的化疗方案,克唑替尼的不良反应与已知的该药物安全性相一致,这项突破性研究结果发表在了《新英格兰医学杂志》。
而PROFILE 1029试验是随机、开放、双臂III期临床研究,旨在评价在东亚人群,ALK抑制剂克唑替尼一线治疗既往未经过系统性治疗的ALK阳性NSCLC患者的疗效和安全性。
PROFILE 1029试验的研究设计与PROFILE 1014完全一样,只是患者人群不一样。
PROFILE 1014包括非亚裔和亚裔人群,而PROFILE 1029是在大样本东亚人群(主要是中国人群)进行的Ⅲ期研究。
研究结果再次证实:与标准含铂类化疗药物相比,每天两次250 mg克唑替尼一线治疗能够显著延长ALK阳性晚期NSCLC东亚患者的无进展生存期(PFS)。
方法和结果PROFILE 1029试验最终入组207例晚期ALK阳性NSCLC患者,其中中国患者183例。
FISH法检测ALK阳性,这些患者既往未接受过任何系统性治疗。
随机入组,分为两组,一组为克唑替尼组,患者接受克唑替尼250 mg BID治疗,直至不能耐受或疾病进展后,研究者判断不能从克唑替尼继续治疗中获益;另一组为化疗组,患者接受顺铂或卡铂联合培美曲塞治疗,每3周一个周期,化疗周期不超过6个周期。
化疗组患者在疾病进展后允许交叉至克唑替尼组,接受克唑替尼治疗。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
【不良反应】
肝功能异常 以下情况请马上联系你的主治医师:比平常更加疲惫,皮肤变黄,眼睛白色球变 黄,尿液变暗或呈棕色(茶色);恶心,呕吐,食欲不振;胃部右侧疼痛;皮肤 瘙痒,或比平时更容易擦伤;医生将进行血常规检测肝功能,如果检测指标不正 常,医生会决定减小克唑替尼的剂量或者停止服用克唑替尼。
肺炎 如果你感觉呼吸困难,咳嗽,发烧,请马上联系你的主治医师。
克唑替尼胶囊说明书 请仔细阅读说明书并在医师指导下使用
【药品名称】 通用名: 克唑替尼胶囊 商品名: 赛可瑞®/XALKORI® 英文名: Crizotinib Capsules 汉语拼音: KeZuoTiNi JiaoNang
【成份】 本品主要成份及其化学名称为: 3-[(R)-1-(2,6-二氯-3-氟苯基)乙氧基]-5-[1-(哌啶-4-基)-1H-吡唑-4-基]吡啶-2-胺 其结构式为:
【有效期】 24个月
普遍的不良反应(1%~10%) • 红细胞,白细胞,血小板减少 • 消化不良 • 心率降低
不常见不良反应(0.1%~1%) • 肾脏闭囊液
【禁忌】 对本品或药物的非范围为15-30℃
【包装】 瓶装,60粒/瓶; 国外购买克唑替尼咨询 xalkori@
分子式:C21H22Cl2FN5O 分子量:450.3367
【性状】 本品为粉红色硬胶囊剂,内容物为白色结晶粉末。
【适应症】 用 于 治 疗 间 变 性 淋 巴 瘤 激 酶 (ALK) 阳 性 的 局 部 晚 期 和 转 移 的 非 小 细 胞 肺 癌 (NSCLC)。
【规格】 (1) 200 mg; (2) 250 mg;
头晕,昏厥,胸部不适 如果你发现心电图症状标识变化,或者心律不齐,请马上联系你的主治医师,医 生会对你进行心电图检测,来观察克唑替尼治疗期间对身体的影响。
非常普遍的不良反应(可能大于10%) • 肝功能异常 • 视觉效应(闪光,视力模糊,重影,一般在服用克唑替尼后不久就会出现) • 神经病(神经麻痹,神经结合处,末端或者肌肉发麻) • 头昏眼花,疲倦 • 水肿(身体组织积液,引起手足水肿) • 肠胃不适(恶心,呕吐,腹泻,便秘,食道咽喉不适) • 食欲不振,味觉减退 • 皮疹
【用法用量】 本品治疗ALK阳性的非小细胞肺癌晚期的推荐剂量是250mg,一次1粒,每日2次, 早晚确定时间各服1粒,一天剂量为500mg,口服;
整粒胶囊吞服,不可嚼碎服用,不可溶解服用,不可打开胶囊;
与食物同服或不同服均可;不可与葡萄汁柚子汁一起服用。
剂量调整 根据药物在个体中的安全性和耐受性情况,在医生的建议下调整剂量。
