118-肱骨远端骨折(英文)
骨科疾病分类

1.开放性骨折的分类(Gustilo) 2.骨骺损伤分类(Salter & Harris) 3.骨骺损伤的特殊类型 4.锁骨外侧端骨折分类(Rockwood) 5.肩锁关节脱位分类(Rockwood) 6.肩锁关节损伤分类(Allman) 7.肱骨近端骨折分类(Neer) 8.盂肱指数 9.肘部骨骺出现和闭合年龄 10.儿童肱骨内髁骨折分类(Kilfoyle,1965) 11.肱骨远端髁间骨折分类(Riseborough) 12.肱骨内、外髁骨折(Milch,1964) 13.Baumann角 14.肘部提携角(Carrying angle) 15.儿童肘关节侧位X线象测量 16.肱骨小头骨骺滑 17.脏关节脂肪垫征 18.儿童肱骨内上髁骨折分类 19.儿童肱骨外髁骨折分类 20.尺内鹰嘴骨折分类 21.尺骨鹰嘴骨折分类 22.桡骨头骨折分类 23.桡骨头骨折分类 24.桡骨颈部骨折分类 25.儿童桡骨头骨折分类 26.Monteggia骨折分类 27.尺桡骨远端长度比较 28.尺桡骨远端形态测量 29.桡骨远端骨折分类 30.Colles骨折 31.桡骨远端关节内骨折分类 32.桡骨远端关节内骨折分类 33.手关节侧位X线象 34.腕关节不稳定的X线测量 35.腕舟骨骨折分类 36.腕舟骨骨折分类 37.月骨无菌性坏死分类 38.月骨无菌性坏死 39.第一掌骨基部骨折分类 40.第一掌腕关
肱骨远端C型骨折

One-third tubular-hook-plate osteosynthesis for olecranon osteotomies in distal humerus type-C fractures:A preliminary report of results and complications K.Schmidt-Horlohe´*,P.Wilde,A.Bonk,L.Becker,R.HoffmannDepartment for Trauma Surgery and Orthopedic Surgery,Berufsgenossenschaftliche Unfallklinik Frankfurt am Main,Friedberger Landstrasse430,60389,Germany Fixing fractures of the distal humerus is one of the mostchallenging procedures in operative trauma care,particularlywhen articular comminution and diminished bone quality arepresent.Adequate exposure of the fracture fragments is needed toallow precise anatomic reduction and proper placement of theimplants.The importance of an early initiation of physical therapyis frequently reported.1–3A large variety of approaches to the distalhumerus has been proposed.4–7However,it is generally agreedthat the best exposure is achieved using a transolecranonapproach,first described by MacAusland in1915.2,4,8,9Thearticular surface exposed via an olecranon osteotomy($60%)isnearly doubled compared with that achieved using the bilatero-tricipital(26%)or triceps-splitting approach(35%),respective-ly.10,11Nevertheless,approach-related complications are frequentand derogate the ing a simple transverse osteotomyand reconstruction with the tension band-wire technique,nonunionrates of up to30%and loss of reduction in60%of patients werereported.7Even with sophisticated approach and osteotomytechniques,complication rates up to14%with respect to theosteotomy remain considerably high,most often represented bynonunion orfixation failure.9,12–16Faced with an increasingpopulation at risk of sustaining distal humerus fractures due todemographic trends,it is of outstanding importance to reduceapproach-related complications.17–19Few clinical and biomechani-cal studies showed promising results using platefixation ofolecranon osteotomies.20–22The one-third tubular-hook-platetechnique was successfully used in treating olecranon fractures.23Low complication rates and excellent clinical results were reported,suggesting the suitability forfixation in osteotomies.This study attempted to determine the usefulness and compli-cation rates of the one-third tubular-hook-plate technique in thetreatment of olecranon osteotomies in distal humerus fractures.Injury,Int.J.Care Injured43(2012)295–300A R T I C L E I N F OArticle history:Accepted27June2011Keywords:Distal humerusFractureOpen reductionApproachOsteotomyOlecranonHook plateFixationFailureA B S T R A C TIntroduction:Distal humerus fractures are rare and challenging to treat.Anatomic reduction of thearticular surface and stable osteosynthesis are mandatory for satisfactory results.The transolecranonapproach allows superior visualisation of the joint.However,controversy exists regarding how best tofixthe osteotomy.The purpose of the present study was to investigate the eligibility of a one-third tubularhook plate for osteosynthesis of olecranon osteotomies in distal humerus type-C fractures.Patients and methods:A consecutive series of34patients who were treated through an olecranonosteotomy and underwentfixation using a one-third tubular hook plate were identified.Thirty-onepatients(17females,14males)with a median age of50years(14–87,standard deviation(SD)18.3)wereavailable for a comprehensive assessment after a mean of12.3months(6–20,SD3.7).Using theArbeitsgemeinschaft fu¨r Osteosynthesefragen(AO)classification,six(19.4%)fractures were categorisedas type C2and25(80.6%)were categorised as C3.Physical and radiological examinations wereperformed.The Mayo Elbow Performance Score(MEPS)and the Disabilities of the Arm,Shoulder andHand score(DASH)were evaluated.Results:Mean extension–flexion ROM was found to be1028(50–1458,SD25).Pronation and supinationwere only slightly compromised.The mean MEPS was87.2points(50–100,SD12.4).Fourteen patients(45.2%)were rated as excellent,and15(48.4%)were rated as good.One patient was rated fair,and onepatient was rated as poor,respectively.Mean DASH score was24.4points(0–65,SD20.3).Complicationsregarding the osteotomy occurred in seven patients(22.5%).Revision surgery was necessary infive cases(16%).At follow-up,all osteotomies went on to d joint degeneration(Broberg I)was found in10patients(32.2%).Implant removal was carried out in15patients(48.4%).Conclusion:Based on this study,the osteosynthesis of olecranon osteotomies using a one-third tubularhook plate can be regarded as a safe procedure with a low complication rate.The implant needed iswidely available and cost-efficient,in contrast to specially designed plates or nails.ß2011Elsevier Ltd.All rights reserved.*Corresponding author.Tel.:+49694752841;fax:+49694752223.E-mail address:kay.schmidt-horlohe@bgu-frankfurt.de(K.Schmidt-Horlohe´).Contents lists available at ScienceDirectInjuryj o ur n a l ho m e p a g e:w w w.e l s e vi e r.c om/l o c a t e/i nj u r y0020–1383/$–see front matterß2011Elsevier Ltd.All rights reserved.doi:10.1016/j.injury.2011.06.418Patients and methodsInclusion and exclusionThirty-four skeletally mature patients with operatively treated isolated type-C fractures of the distal humerus(Arbeitsge-meinschaft fu¨r Osteosynthesefragen(AO)classification)24seen during the period from December2005until January2010were identified retrospectively.Patients who were skeletally immature at the time of injury as well as fractures treated by implants other than angular-stable plates or those who underwentfixation through an approach other than olecranon osteotomy were excluded.Patients with accompanying injuries of the elbow(i.e., olecranon or radial head fracture)were also excluded.Only patients who underwent open reduction and internalfixation (ORIF)of the distal humerus via a transolecranon approach and refixation involving a one-third tubular hook plate were included.The study protocol was reviewed and approved by the Institutional Review Board of the department involved.Each patient provided written and informed consent.Thirty-two patients met the inclusion criteria.One patient died for reasons not related to the index procedure.As a result,31 patients(97%)were available for a comprehensive assessment.Clinical and radiological assessmentThe assessment included a review of the patient charts and detection of complications that arose during the treatment course. Complications were grouped as minor and major:they were deemed major if significant impairment resulted or surgical intervention was needed.At follow-up,a standard physical examination was performed.In addition to range-of-motion (ROM)measurement and testing the stability of the elbow joint, the Mayo Elbow Performance Score(MEPS)25and the Disabilities of the Arm,Shoulder and Hand score(DASH)26as elbow-and limb-specific questionnaires were surveyed.Postoperative antero-posterior and lateral radiographs were used to evaluate the quality of osteotomy reduction andfixation.A step or gap of<2mm at the articular surface of the olecranon was considered satisfactory.27Union was defined as replacement of the radiolucent osteotomy site with bone on antero-posterior and lateral radiographs.Nonunion of the osteotomy was defined as radiolucency beyond the6th postoperative month in association with pain.Assessment of degenerative changes followed the classification system of Broberg:grade0=normal elbow,grade I=slight joint space narrowing with minimum osteophyte forma-tion,grade II=moderate joint space narrowing with moderate osteophyte formation and grade III=severe degenerative changes with gross destruction of the joint.28Heterotopic ossifications(HOs) were classified using the Hastings rating scale,with class I being HO without functional limitation;class II,subtotal limitations in one or two planes;and class III,ankylosis of the joint.29The duration of the operative procedures was not evaluated for this study because it was mainly influenced by the treatment of the distal humerus fracture rather than repair of the olecranon osteotomy.The frequency of implant removal with respect to the olecranon was recorded.Surgical techniqueThe surgical procedure was performed with the patient under general anaesthesia,in the supine position,with the involved arm on an armrest.A tourniquet was used,depending on the surgeon’s ing a posterior midline incision,medially and laterally full-thicknessflaps were developed.The ulnar nerve was identified and mobilised routinely;however,anterior transposition was carried out depending on the position of the implant at the medial epicondyle.After blunt dissection of the triceps at the medial and lateral intermuscular septae,medial visualisation of the olecranon joint was performed to identify the bare area.Depending on surgeons’preference,an interfragmentary screw hole for refixation was drilled before performing the ing a thin oscillating saw,an apex-distal configured osteotomy of the olecranon was created,approximately2.5cm distal to the olecranon tip.The V-shaped pattern theoretically improves rotational stability and increases the bone surface for improved healing.The osteotomy was completed by fracturing the last third of the ulna,creating an irregular osteochondral fracture line for improved interdigitation and facilitated reduction. Reduction andfixation of the distal humerus fracture were performed using anatomically contoured,angular-stable implants (LCP distal humerus plates system,Synthes,Umkirch,Germany) with use of the standard Arbeitsgemeinschaft fu¨r Osteosynthese-fragen/American Society for Internal Fixation(AO/ASIF)tech-nique.30At the conclusion of the procedure,temporary reduction of the olecranon fragment was secured using K-wires.Definitive fixation was achieved using a one-third tubular hook plate.By cutting off the terminal plate link,leaving two spikes,and bending the terminal plate link to a hook,the plate was thenfitted to the individual anatomy of the olecranon.Following a wing-like incision of the distal insertion of the triceps tendon,the hooks were placed near the tip of the olecranon,carefully avoiding irritation of the olecranon fossa.Subsequently,compression was created at the osteotomy site by using eccentrically placed shaft screws.Thereafter,the olecranon fragment was additionallyfixed and compression was increased through a so-called beam screw extending through the plate and olecranon distally to the anterior cortex near the base of the coronoid(Fig.1).The triceps incision and the intermuscular approach werefinally adapted with No.1 resorbable sutures.Postoperative protocolAt24–48h,the subcutaneous drain was removed.Immobilisa-tion was carried out if necessary,depending onfixation stability at the distal humerus.Early physiotherapy with unrestricted exten-sion andflexion were allowed with respect to olecranon osteotomy osteosynthesis.Full weight-bearing exercises were performed when radiological fracture and osteotomy healing were verified.Statistical analysisStatistical analyses were performed with the Predictive Analytics Software(PASW)Statistics18software package(SPSS Inc.,Chicago,IL,USA).Data are represented as means and standard deviations.ResultsThis study investigated31patients with osteotomies of the olecranonfixed with a one-third tubular hook plate.The average age of the17women and14men was50years(14–87,standard deviation(SD)18.3).The dominant arm was involved in11cases (35.5%).Six(19.4%)fractures of the distal humerus were classified as C2,and25(80.6%)were classified as C3type.Eight fractures (25.8%)were grade I,and two fractures(6.5%)were grade II open (Gustilo classification).31After a mean of12.3months(6–20,SD 3.7),the patients were followed up.In all patients,the olecranon osteosynthesis was considered stable by the surgeon,and thus did not interfere with the rehabilitation protocol.However,due to distal humerusK.Schmidt-Horlohe´et al./Injury,Int.J.Care Injured43(2012)295–300 296osteosynthesis,immobilisation of the elbow was needed in five patients for 20days (7–42,SD 20.2).The mean extension–flexion arc of motion at the time of follow-up was found to be 1028(50–1458,SD 25).There was a mean extension deficit of À208(À58to 408,SD 13.7)in 28patients,whereas extension was not compromised in only three patients.Mean flexion was 1228(80–1458,SD 19.4).With 818external (15–908,SD 16.6)and 858internal rotation (70–908,SD 7.3),forearm motion was almost ing the MEPS,14patients (45.2%)were rated as excellent and 15(48.4%)as good.One patient was rated as fair,and one patient was rated as poor.The mean MEPS score was 87.2points (50–100,SD 12.4).The mean DASH score was 24.4points (0–65,SD 20.3).With respect to the olecranon osteotomy,a total of 11complications occurred in seven patients (22.5%).The details of the two minor and five major complications are displayed in Table 1.Surgical interventions concerning the olecranon osteotomy were necessary in five cases (16%).All nonunions and mechanical failures went on to union after revision surgery.As measured from the postoperative radiographs,there were no osteotomies with a gap or step of more than 2mm at the articular surface.Degenerative changes of the elbow joint at stage I (according to Broberg)were found in 10patients (32.2%).Heterotopic bone formation was present in four patients (two type-I patients and two IIa patients,according to Hastings classification).At final follow-up,the hook plate had already been removed in 15patients (48.4%).Implant removal was performed upon patient request.The hook plate was reported as bothersome in only two cases (6.4%).DiscussionThe purpose of the study presented was to determine the usefulness and complication rates of the one-third tubular-hook-plate technique in the treatment of olecranon osteotomies in distal humerus fractures.Although nearly 81%of the patients presented with type-C3fractures,14excellent and 15good results were found in the MEPS.The mean MEPS score was found to be 87.2points and the mean DASH score was 24.4points.All osteosynthesis of the olecranon osteotomy were considered stable to allow early initiation of physical therapy by the treating surgeon.In total,11complications occurred in seven patients (22.5%).Surgical intervention due to complications was necessary in five cases (16%).The implant was reported as bothersome with subsequent implant removal in two patients.Intra-articular fractures of the distal humerus are rare and difficult to treat.However,good functional results can be obtained when anatomic and stable joint reconstruction is achieved,and early initiation of physical therapy is realised.1,3,8,32–37Therefore,adequate visualisation of the articular surface is of major importance.Several approaches to the distal humerus have been advocated.There remains controversy as to whether these fractures should be treated through a triceps-sparing,triceps-splitting or transolecranon approach.The articular surface exposed is maximised using the transolecranon approach,emphasising its suitability as the gold standard in complex distal humerus fractures.2,4,8,10,11,13,38If total elbow arthroplasty is considered as a treatment option,the transolecranon approach should be considered critical because it interrupts the extensormechanismFig.1.Technique for one-third tubular hook plate:(a)cutting the plate link,(b)plate with spikes,(c)bending,(d)and (e)one-third tubular hook plate finished for refixation ofthe osteotomy.K.Schmidt-Horlohe´et al./Injury,Int.J.Care Injured 43(2012)295–300297and refixation is hindered by the ulnar stem.In this situation, precise preoperative planning including multiplanar computed tomography(CT)reconstruction is mandatory.The bilaterotrici-pital approach described by Alonso-Lames allows the surgeon to explore the articular situation,with the option to extend the procedure to an olecranon osteotomy if ORIF seems possible.Enthusiasm for the transolecranon approach is somewhat limited by the various complications resulting from the osteotomy and itsfixation.However,the functional results found in our study were excellent or good in the vast majority of patients(>90%)(Fig.2).On the one hand,thesefindings might be explainable by the new angular-stable fixation device for the distal humerus,allowing an early initiation of physical therapy in nearly all patients.Similar clinical results were found in previous studies dealing with angular stable osteosynth-esis.16,39–41On the other hand,the quality of restoration of the distal humerus articular surface might have been influenced positive by visualisation through the transolecranon approach.5,42 As in all patients the hook-plate osteosynthesis was considered as stable,the approach did not hinder the rehabilitation protocol.In contrast to the promising functional results,we found an overall complication rate of22.5%related to the osteotomy.InFig.2.Case of a33-year-old patient who suffered from a I8open C2fracture of the distal humerus.(a)preoperative X-ray,(b)osteosynthesis of the distal humerus fracture with the LCP distal humerus plate system(Synthes,Umkirch,Germany)and refixation of the osteotomy with a one-third tubular hook plate(c)functional result after1year. Table1Detailed description of the two minor andfive major complications.Type of complication Total(n)%Complications in detail(potential coincidental)n%Patient ID Minor2 6.4Delayed union2 6.425;30Screw loosening1 3.225Major516.0Bothersome implant a2 6.47;10Non-union2 6.412;22Dislocation412.93;7;12,22a Necessitating removal.K.Schmidt-Horlohe´et al./Injury,Int.J.Care Injured43(2012)295–300298detail,two patients suffered minor andfive major complications. The amount of minor complications seems to be negligible as the postoperative and rehabilitative course was not affected.Addi-tional surgery concerning the osteotomy andfixation was necessary in thefive patients with major complications(16%).Comparing13patients with olecranon osteotomies and13 patients treated with a triceps split approach for the treatment of open supracondylar fractures,McKee et al.observed improved scores on the DASH and Mayo Elbow questionnaire following use of the triceps split technique.43However,the same author found no differences concerning ROM and strength between the triceps split and transolecranon approach in a later study;tension band-wire removal was necessary in27%of the osteotomy group.44 Accordingly,Ring et al.found symptoms related to tension band wiring in13%.45Using intramedullary screw and tension band wiring for osteosynthesis of the olecranon osteotomy,Tak et al. report19%symptomatic implants necessitating removal.46K-wire migration was found in31%of the series published by Gupta, leading the authors to recommend intramedullary screwfixa-tion.47However,due to the angulation of the proximal ulna and the large variety in intramedullary canal diameter,intramedullary screwfixation must be considered with caution.4,5,48,49 Removal of symptomatic implants at the olecranon was performed in two patients(6.4%)in our series,which is remarkably less than in the studies aforementioned.Thesefindings are comparable with those of Coles et al.,who found symptomatic osteotomyfixation in8%.The removal rate of symptomatic implants was distributed equally between intramedullary screw and platefixation in his study($6.5%).5Since Gainor found30%nonunion in transverse osteotomies,it is now well accepted that the olecranon osteotomy should be performed in a chevron style to maximise the bony contact area.7 In addition,the chevron-style technique,combined with an osteochondral fracture line,facilitates anatomic reduction and theoretically improves rotational stability.4,5,45,46We are in concert with this statement and routinely use an apex distal chevron-style osteotomy.The nonunion rate reported in the literature is nearly identical with the rate found in our study and ranges from6.4%to9%.12–14 Hewins and Gofton reported low complication rates of6%and0% using3.5-mm reconstruction plates.14,20However,using implants other than a3.5-mm reconstruction plate(i.e.,tension band wiring and intramedullary screw),Gofton found25%nonunions at the osteotomy site.Using tension band wiring for refixation of both intra-and extra-articular osteotomies,Sane et al.reported36%of patients to have non-anatomic reductions.15By contrast,Coles et al.observed fixation failure with dislocation in only two patients(3%)in whom fixation was carried out by use of intramedullary screws.Dislocation of the olecranon osteotomy was encountered in four patients(12.9%)of our series.In all four patients,unrestricted ROM exercises were permitted.At least in two patients,compli-ance might have been questionable.In another patient,the beam screw did not penetrate the anterior cortex of the coronoid process, thereby weakening the construct stability.The rate of wound infection is reported with up to10%in the literature.12,46,50Much to our delight,we found no infections in our cohort although more than32%of the fractures were grade I and II open.In summary,the encountered complications in our population described remain manageable,particularly when compared with complex reconstructive issues at the distal humerus as a result of inadequate articular visualisation.Our data indicate that plate fixation of olecranon osteotomies is a suitable method.Biomechanical studies strongly support the use of plates.There are some potential advantages to the use of plate osteosynthesis for olecranon osteotomies.In a biomechanical study,a significantly smaller displacement was found when comparing tension band wiring and posterior plating of osteotomies in embalmed human ulna.22,51This might become important in the context of early active-motion therapy.The limitations of our study are related to the inherent weakness of a retrospective review and the relatively small number of patients.There was no comparison with techniques other than the olecranon osteotomy approach involving use of a one-third tubular hook plate.Sufficient anatomic reduction of the olecranon was achieved in all patients.However,results were evaluated using plain radiographs in two planes.A threshold of a2-mm articular step or gap was used on the basis of Murphy et al., who found significantly more degenerative elbow joint changes in patients with incongruences above2mm.27Due to geometrically determined effects,small amounts of displacement may not have been detected.This should also be recognised as a limitation.It needs to be mentioned that the functional results are mainly influenced by the fracture of the distal humerus,rather than the approach used.In addition,the short duration of follow-up might have contributed to the low incidence of osteoarthritis,which is known to develop after many years.The strengths of the study include standardised treatment of the distal humerus fracture with latest-generation angular-stable plates,performance of olecranon osteosynthesis with one single technique and the inclusion of consecutive patients.The use of standard and validated outcome measurements should also be judged as a strength.For future research,prospective randomised trials including different approaches and,in case of osteotomy,different types of osteotomy refixation in larger sample sizes are needed.Only C3 fractures should be included to homogenise the study cohort.In addition,the treatment of the distal humerus fracture should be performed using a single type of implant to exclude potential confounding factors.Evaluating the approaches and related complications,the future studies ought to focus on the osteotomy complications rather than functional result,as this is mainly influenced by the distal humerus fracture itself.ConclusionsExposure is enhanced by olecranon osteotomy,which facilitates reduction and internalfixation of complex distal humerus fractures,thereby improving the quality of anatomic reconstruc-tion and enabling superior outcome.One-third tubular-hook-plate osteosynthesis after chevron-shaped olecranon osteotomies achieves high primary stability with relatively few complications, thus not interfering with an active ROM postoperative protocol in distal humerus fractures.In addition,the implant is marked by its cost-effectiveness and widespread availability.Anatomically pre-shaped and angular-stable plates as well as specially designed nails might be suitable for refixation of osteotomies,but they are much more expensive.52–54Nonunion and failure rates are in concert with previous studies but the need for implant removal is remarkably decreased. Reviewing our31patients,we feel comfortable in recommending the one-third tubular-hook-plate osteosynthesis of olecranon osteotomies as a simple and safe procedure.Conflicts of interestThe authors of the paper‘‘One-third tubular hook plate osteosynthesis for olecranon osteotomies in distal humerus type C fractures:a preliminary report of results and complications’’state that there are no conflicts of interest.K.Schmidt-Horlohe´et al./Injury,Int.J.Care Injured43(2012)295–300299References1.Korner J,Lill H,Muller LP,Hessmann M,Kopf K,Goldhahn J,et al.Distalhumerus fractures in elderly patients:results after open reduction and internalfixation.Osteoporos Int2005;16(Suppl.2):S73–9.2.Jupiter JB,Neff U,Holzach P,Allgower M.Intercondylar fractures of thehumerus.An operative approach.J Bone Joint Surg Am1985;67:226–39.3.Letsch R,Schmit-Neuerburg KP,Sturmer KM,Walz M.Intraarticular fractures ofthe distal humerus.Surgical treatment and results.Clin Orthop Relat Res 1989;(241):238–44.4.Pollock JW,Athwal GS,Steinmann SP.Surgical exposures for distal humerusfractures:a review.Clin Anat2008;21:757–68.5.Coles CP,Barei DP,Nork SE,Taitsman LA,Hanel DP,Bradford Henley M.Theolecranon osteotomy:a six-year experience in the treatment of intraarticular fractures of the distal humerus.J Orthop Trauma2006;20:164–71.6.Cottias P,Camara KB,Clavert P,Kahn JL,Liverneaux PA.Digastric olecranonosteotomy:feasibility study of a new approach to the elbow.Surg Radiol Anat 2010;32:485–9.7.Gainor BJ,Moussa F,Schott T.Healing rate of transverse osteotomies of theolecranon used in reconstruction of distal humerus fractures.J South Orthop Assoc1995;4:263–8.8.Gupta R.Intercondylar fractures of the distal humerus in adults.Injury1996;27:569–72.9.Henley MB.Intra-articular distal humeral fractures in adults.Orthop Clin NorthAm1987;18:11–23.10.Dakoure PW,Ndiaye A,Ndoye JM,Sane AD,Niane MM,Seye SI,et al.Posteriorsurgical approaches to the elbow:a simple method of comparison of the articular exposure.Surg Radiol Anat2007;29:671–4.11.Wilkinson JM,Stanley D.Posterior surgical approaches to the elbow:a com-parative anatomic study.J Shoulder Elbow Surg2001;10:380–2.12.Kundel K,Braun W,Wieberneit J,Ruter A.Intraarticular distal humerusfractures.Factors affecting functional outcome.Clin Orthop Relat Res 1996;(332):200–8.13.Henley MB,Bone LB,Parker B.Operative management of intra-articular frac-tures of the distal humerus.J Orthop Trauma1987;1:24–35.14.Gofton WT,Macdermid JC,Patterson SD,Faber KJ,King GJ.Functional outcomeof AO type C distal humeral fractures.J Hand Surg Am2003;28:294–308. 15.Sane AD,Dakoure PW,Dieme CB,Kinkpe CV,Dansokho AV,Ndiaye A,et al.Olecranon osteotomy in the treatment of distal humeral fractures in adults: anatomical and functional evaluation of the elbow in14cases.Chir Main 2009;28:93–8.16.Schmidt-Horlohe K,Bonk A,Wilde P,Becker L,Hoffmann R.Functional resultsafter osteosynthesis of the distal humerus fracture with an anatomically precontoured,angular-stable double plate system.Z Orthop Unfall 2010;148:300–8.17.Palvanen M,Kannus P,Niemi S,Parkkari J.Secular trends in distal humeralfractures of elderly women:nationwide statistics in Finland between1970and 2007.Bone2010;46:1355–8.18.Palvanen M,Kannus P,Niemi S,Parkkari J.Secular trends in the osteoporoticfractures of the distal humerus in elderly women.Eur J Epidemiol1998;14:159–64.19.Palvanen M,Niemi S,Parkkari J,Kannus P.Osteoporotic fractures of the distalhumerus in elderly women.Ann Intern Med2003;139.p.W-W61.20.Hewins EA,Gofton WT,Dubberly J,MacDermid JC,Faber KJ,King GJ.Platefixation of olecranon osteotomies.J Orthop Trauma2007;21:58–62.21.Petraco DM,Koval KJ,Kummer FJ,Zuckerman JD.Fixation stability of olecranonosteotomies.Clin Orthop Relat Res1996:181–5.22.Tejwani NC,Garnham IR,Wolinsky PR,Kummer FJ,Koval KJ.Posterior olecra-non plating:biomechanical and clinical evaluation of a new operative tech-nique.Bull Hosp Jt Dis2002;61:27–31.23.Schmidt-Horlohe´K,Wilde P,Becker L,Reimertz C,Bonk A,Hoffmann R.Functional and radiological results after modified one-third tubular-hook plate osteo-synthesis in olecranon fracture treatment(Abstract).German Medical Science GMS Publishing House;2009.DocWI65-1126.24.Mu¨ller M,Nazarian S,Koch P.The AO classification of long bones.Berlin HeidelberNew York:Springer;1987.25.Morrey BF,An KN.Evaluation of the elbow.3rd ed.Philadelphia,London,NewYork,St.Louis,Sydney,Toronto:WB Sounders Company;2000.26.Hudak PL,Amadio PC,Bombardier C.Development of an upper extremityoutcome measure:the DASH(disabilities of the arm,shoulder and hand) [corrected].The Upper Extremity Collaborative Group(UECG).Am J Ind Med 1996;29:602–8.27.Murphy DF,Greene WB,Dameron Jr TB.Displaced olecranon fractures in adultsclinical evaluation.Clin Orthop Relat Res1987:215–23.28.Broberg MA,Morrey BF.Results of delayed excision of the radial head afterfracture.J Bone Joint Surg Am1986;68:669–74.29.Hastings2nd H,Graham TJ.The classification and treatment of heterotopicossification about the elbow and forearm.Hand Clin1994;10:417–37.30.Ruedi T,Buckley R,Moran C.AO principles of fracture managment.AO Publishing;2007.31.Gustilo RB,Anderson JT.Prevention of infection in the treatment of onethousand and twenty-five open fractures of long bones:retrospective and prospective analyses.J Bone Joint Surg Am1976;58:453–8.32.Papaioannou N,Babis GC,Kalavritinos J,Pantazopoulos T.Operative treatmentof type C intra-articular fractures of the distal humerus:the role of stability achieved at surgery onfinal outcome.Injury1995;26:169–73.33.Holdsworth BJ,Mossad MM.Fractures of the adult distal humerus.Elbowfunction after internalfixation.J Bone Joint Surg Br1990;72:362–5.34.John H,Rosso R,Neff U,Bodoky A,Regazzoni P,Harder F.Operative treatment ofdistal humeral fractures in the elderly.J Bone Joint Surg Br1994;76:793–6. 35.Lill H,Josten C.Proximal and distal humerus fractures in advanced age.Orthopade2000;29:327–41.36.Ring D,Jupiter JB.Fractures of the distal humerus.Orthop Clin North Am2000;31:103–13.37.Huang TW,Wu CC,Fan KF,Tseng IC,Lee PC,Chou YC.Tension band wiring forolecranon fractures:relative stability of Kirschner wires in various configura-tions.J Trauma2010;68:173–6.38.Helfet DL,Kloen P,Anand N,Rosen HS.Open reduction and internalfixation ofdelayed unions and nonunions of fractures of the distal part of the humerus.J Bone Joint Surg Am2003;85-A:33–40.39.Greiner S,Haas NP,Bail HJ.Outcome after open reduction and angular stableinternalfixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system.Arch Orthop Trauma Surg2008;128:723–9.40.Rubberdt A,Surke C,Fuchs T,Frerichmann U,Matuszewski L,Vieth V,et al.Preformed plate-fixation system for type AO13C3distal humerus fractures: clinical experiences and treatment results taking access into account.Unfall-chirurg2008;111:308–22.41.Reising K,Hauschild O,Strohm PC,Suedkamp NP.Stabilisation of articularfractures of the distal humerus:early experience with a novel perpendicular plate system.Injury2009;40:611–7.42.Huang TL,Chiu FY,Chuang TY,Chen TH.The results of open reduction andinternalfixation in elderly patients with severe fractures of the distal humerus:a critical analysis of the results.J Trauma2005;58:62–9.43.McKee MD,Kim J,Kebaish K,Stephen DJ,Kreder HJ,Schemitsch EH.Functionaloutcome after open supracondylar fractures of the humerus.The effect of the surgical approach.J Bone Joint Surg Br2000;82:646–51.44.McKee MD,Wilson TL,Winston L,Schemitsch EH,Richards RR.Functionaloutcome following surgical treatment of intra-articular distal humeral frac-tures through a posterior approach.J Bone Joint Surg Am2000;82-A:1701–7.45.Ring D,Gulotta L,Chin K,Jupiter JB.Olecranon osteotomy for exposure offractures and nonunions of the distal humerus.J Orthop Trauma2004;18: 446–9.46.Tak SR,Dar GN,Halwai MA,Kangoo KA,Mir BA.Outcome of olecranonosteotomy in the trans-olecranon approach of intra-articular fractures of the distal humerus.Ulus Travma Acil Cerrahi Derg2009;15:565–70.47.Gupta R,Khanchandani P.Intercondylar fractures of the distal humerus inadults:a critical analysis of55cases.Injury2002;33:511–5.[48].Rouleau DM,Faber KJ,Athwal GS.The proximal ulna dorsal angulation:aradiographic study.J Shoulder Elbow Surg2010;19:26–30.49.Wang AA,Mara M,Hutchinson DT.The proximal ulna:an anatomic study withrelevance to olecranon osteotomy and fracturefixation.J Shoulder Elbow Surg 2003;12:293–6.50.Srinivasan K,Agarwal M,Matthews SJ,Giannoudis PV.Fractures of the distalhumerus in the elderly:is internalfixation the treatment of choice?Clin Orthop Relat Res2005:222–30.51.Fyfe IS,Mossad MM,Holdsworth BJ.Methods offixation of olecranon fractures.An experimental mechanical study.J Bone Joint Surg Br1985;67:367–72. 52.Athwal GS,Hoxie SC,Rispoli DM,Steinmann SP.Precontoured parallel platefixation of AO/OTA type C distal humerus fractures.J Orthop Trauma 2009;23:575–80.53.Koslowsky TC,Mader K,Dargel J,Schadt R,Koebke J,Pennig D.Olecranonfracturefixation with a new implant:biomechanical and clinical consider-ations.Injury2009;40:618–24.54.Nowak TE,Mueller LP,Sternstein W,Burkhart KJ,Reuter M,Mueller LA,et al.Dynamic analysis of olecranon osteosyntheses—an in vitro comparison of two osteosynthesis systems.Biomed Tech(Berl)2008;53:86–90.K.Schmidt-Horlohe´et al./Injury,Int.J.Care Injured43(2012)295–300 300。
肱骨干骨折(fracture of the shaft of the humerus)(1)
概述肱骨外科颈远端1cm以下至肱骨髁部上方2cm以上为肱骨干。
肱骨干骨折(fracture of the shaft of the humerus)多见于青壮年,好发于中部,其次为下部,上部最少。
中下1/3段后外侧有桡神经沟,有由臂丛神经后束发出的桡神经经内后方紧贴骨面斜向外前方进入前臂,此处骨折易合并桡神经损伤,下1/3骨折易发生骨不连。
病因和发病机制1、直接暴力常发生于交通及工伤事故,多见于中1/3,多为粉碎或横行骨折。
2、间接暴力跌倒时因手掌或肘部着地所致,多见于下1/3,骨折线为斜形或螺旋形。
3、旋转暴力新兵训练中,少数新战士投手榴弹突然间前臂及肱骨远端向前及内旋,而肩部及肱骨近端未能前旋,不协调应力作用于肱骨中段,导致投掷的扭转螺旋骨折。
好发于中下1/3处,骨折线为螺旋形。
肱骨干骨折端的移位除与暴力方向及肢体重力有关外,更与肌肉的收缩直接有关。
当骨折位于肱骨干上部、三角肌止点之上时,骨折近端受胸大肌、背阔肌和大圆肌的牵拉向前内移位,远端受三角肌牵拉向上外移位;肱骨干中部骨折,骨折处位于三角肌止点以下时,近端因三角肌和喙肱肌收缩向外前移位,远端因肱二头肌、肱三头肌收缩向上移位;肱骨干下部骨折,两端肌肉拉力基本平衡,移位方向取决于外力方向、肢体所处位置及重力等。
临床表现受伤后上臂出现疼痛、肿胀、畸形,皮下淤斑,上肢活动障碍。
若合并桡神经损伤可出现腕下垂、拇指不能外展、掌指关节不能自主伸直、前臂旋后障碍,手背桡侧皮肤感觉减退或消失。
实验室及其他检查1、查体可发现假关节活动,骨摩擦感,骨传导音减弱或消失;2、X线摄片可确定骨折的类型、移位方向。
坎贝尔第三卷(英文版)-肱骨远端骨折
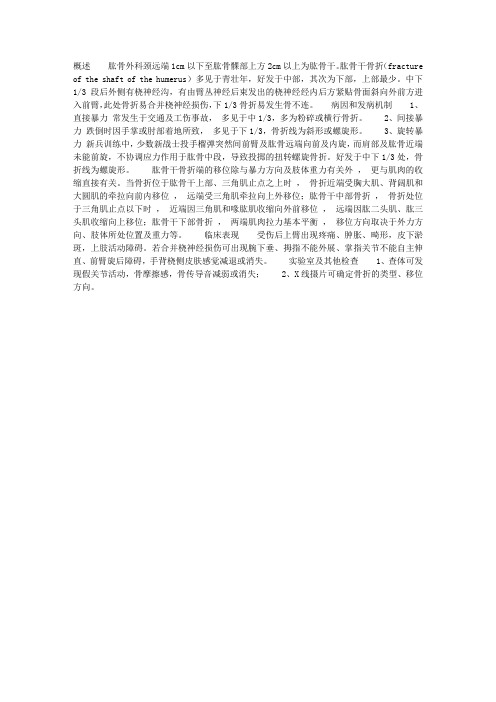
Canale & Beaty: Campbell's Operative Orthopaedics,11th ed.ElsevierDISTAL HUMERAL FRACTURESFractures of the distal humerus remain a challenging problem despite advances in technique and implants.These injuries often involve articular comminution, and many occur in older patients with osteoporotic bone.Joint function often is compromised because of stiffness, pain, and weakness. Rarely is a “normal” elbow the outcome after these fractures, but outcomes have been improved with advances in implant technology,surgical approaches, and rehabilitation protocols. Most distal humeral fractures in adults must be treated operatively, in contrast to fractures of the proximal humerus or humeral shaft. Nonoperative treatment with the “bag of bones” technique may be reasonable in an elderly patient with significant medical comorbidities.The complexity of distal humeral fractures in adults is reflected in the attempts at classifying the variety of injuries possible in this location. The AO/OTA classification, if all subgroup classifications are used, defines 61 types, although the three kinds of articular involvement are the most commonly used designations—A,extraarticular; B, partially articular; and C, completely articular. A more recent classification systemsuggested by Jupiter and Mehne is simpler: it describes only 25 types. This classification system is based on the “two-column” and “tie-arch” concepts of elbow stability. Mehne and Matta described complexbicolumnar distal humeral fractures according to the configuration formed by the fracture lines (Fig. 54-38):high or low T-fractures, Y-fractures, H-fractures, and medial and lateral l-fractures. We generally prefer to use the Jupiter classification system because it has been useful for preoperative planning.Fig. 54-38 A-F, Mehne and Matta classification of distal humeral fractures.(From Jupiter JB: Internal fixation for fracture about the elbow, Op Tech Orthop 4:34, 1994.)l i k u Www .d o c u -tr a c k .c mC c t ob yNO !w w .d o c u -t r a c k .c oThe goal of treatment is anatomical restoration of the joint surface with stable internal fixation that allows early motion. Lateral or medial column fractures (AO/OTA type B) (Fig. 54-39) usually can be reduced through a direct approach and fixed with simple buttress plating. Intraarticular fractures (AO/OTA type C)vary greatly. Generally, the lower the transverse component, the more difficult is attaining stable fixation.Likewise, the greater the comminution, the more difficult is attaining an anatomical reduction.A variety of approaches have been described for reduction and fixation of distal humeral fractures (Table 54-1). Most commonly, a posterior approach with an olecranon osteotomy has been used (see Technique 54-8), but concerns about healing and symptomatic implants have led to more frequent use of a triceps-reflecting (Bryan-Morrey [Fig. 54-40] or triceps-reflecting anconeus pedicle [Fig. 54-41]) approach, as advocated by Bryan and Morrey and O'Driscoll, or a triceps-splitting (Campbell [Fig. 54-42]) approach, as advocated by McKee et al. The best fracture exposure is provided by an olecranon osteotomy approach. As more familiarity is gained with fracture patterns and reduction techniques, a triceps-reflecting or triceps-splitting approach may be selected to reduce complications. With all posterior approaches, the ulnar nerve must be carefully dissected without excessive stripping and usually is transposed anterior to the medial epicondyle at the end of the procedure.Table 54-1 -- Surgical Approaches Used for Treatment of Fractures of the Distal HumerusFig. 54-39 A and B, Isolated lateral condylar fracture fixed with lag screw and minifragment buttress plate.SurgicalApproach Indications Contraindications Advantages Disadvantages Posterior Olecranon osteotomyORIF for fractures involving columns and articular surfaceTERGood access to posterior articular surfaces for reconstructionNonunion and failure of fixation of osteotomy Poor anterior access to capitellum Triceps-splittingORIF/TER for fractures involving columns and articular surfacePrevious olecranon osteotomy approach Patients atincreased risk forAvoidscomplications associated with olecranon osteotomyPoor access to articular surface for internal fixation Risk of tricepsww .d o c u -tr a c k .c w .d o c u -t r a c k .c ohealing problemsdetachment Triceps-reflectingFractures requiring TERORIFPrevious olecranon osteotomy approach Patients at risk for healing problemsAvoidscomplications associated with olecranon osteotomyRisk of triceps detachmentTriceps-detachingORIF/TER for fractures involving columns and articular surfacePrevious olecranon osteotomy approach Patients at risk for healing problemsAvoidscomplications associated with olecranon osteotomy Poor access to articular surfaces for internal fixation Risk of triceps detachment MedialMedialepicondylar fractures Lateral column inaccessibleMedial column fracturesKocherLateral column fractures Suspected more complex articular surface fractureRadial nerve protected Medial column inaccessibleLateralepicondylar fractures Capitellar fracturesLateral KoeberRisk of injury to radial nerve Medial column inaccessibleJupiterComplex articular surface fractures Significant involvement of the columns Medial column inaccessible AnteriorHenryVascular injuryRequirement for plate fixation of columns or articular surface reconstructionGood access to brachial arteryLimited access to columnsModified from Robinson CM: Fractures of the distal humerus. In Bucholz RW, Heckman JD, Court-Brown CM,eds: Rockwood and Green's fractures in adults, 6th ed. Philadelphia, 2006, Lippincott Williams & Wilkins.TECHNIQUE 54-8ORIF, open reduction and internal fixation; TER, total elbow replacement.Open Reduction and Internal Fixation of the Distal Humerus with Olecranon Osteotomy•P Aww .d o c u -tr a c k .c w .d o c u -t r a c k .c o•ParMthDPFig. 54-46Olecranon osteotomy approach (see text).A, Olecranon osteotomy is marked in shape of shallow V or chevron.B, Thin-blade oscillating saw is used to start osteotomy.C, Osteotomized proximal olecranon fragment is elevated proximally; ulnar nerve is isolated, mobilized, and protected.•LatriEPMthRprDUIfin).Fig. 54-47Open reduction and internal fixation of distal humerus through olecranon osteotomy approach (see text).A, Threaded Kirschner wires used as joysticks for fracture reduction.B, After plate application.C, After plate fixation of olecranon osteotomy.•PIfreRanUcoEERlaFig. 54-40 A and B, Plate application through triceps-reflecting approach.Fig. 54-41Triceps-reflecting anconeus pedicle approach.A, Modified Kocher lateral approach is combined with medial triceps-reflecting approach.B, Access to distal humerus is similar to that provided by olecranon osteotomy.(From Sanchez-Sotelo J, Torchia ME, O'Driscoll SW: Principle-based internal fixation of distal humerus fractures, Tech Hand Upper Extremity Surg 5:179, 2001.)The standard plating technique calls for plates to be placed at orthogonal angles (90-90 plating) (Fig. 54-43). Studies by Self et al. and Schemitsch et al. showed that direct medial and lateral plating isbiomechanically sound (Fig. 54-44). Sanchez-Sotelo et al. listed several principles for distal humeral fracture fixation that we have incorporated into our treatment protocol (Box 54-2). Small osteochondralfragments can be fixed with headless screws, countersunk minifragment screws, or absorbable screws (Fig.54-45).Fig. 54-42Triceps-splitting approach to distal humerus.A, Triceps split.B,Split extended to transcutaneous border of ulna.(From Frankle MA: Triceps split technique for total elbow arthroplasty, Tech Shoulder Elbow Surg 3:23, 2002.)Fig. 54-43 A, Supracondylar fracture with intraarticular extension.B, Fixation with 90-90 locked plates through olecranon osteotomy approach.C, After removal of symptomatic hardware.Fig. 54-44 A, Distal humeral fracture with intraarticular extension.B, After direct medial and lateral plate fixation.Box 54-2Technical Objectives for Fixation of Distal Humeral FracturesEvery screw should pass through a plate.Each screw should engage a fragment on the opposite side that is also fixed to a plate.As many screws as possible should be placed in the distal fragments.Each screw should be as long as possible.Each screw should engage as many articular fragments as possible.Plates should be applied such that compression is achieved at the supracondylar level for bothcolumns.Plates used must be strong enough and stiff enough to resist breaking or bending before unionoccurs at the supracondylar level.From Sanchez-Sotelo J, Torchia ME, O'Driscoll SW: Principle-based internal fixation of distal humerus fractures, Tech Hand Upper Extremity Surg 5:179, 2001.Fig. 54-45 A, Fixation of small osteochondral fragment with absorbable screw.B, Very distal intercondylar fracture fixed with headless screws and minifragment buttress plating through olecranon osteotomy approach.Reconstruction of the distal humerus can be done according to two strategies: (1) reduction and fixation of the articular surfaces followed by attachment to the humeral shaft or (2) reduction and fixation of the medial or lateral condyle to the shaft, then reconstruction of the articular surface (advantageous when the articular surface is comminuted), followed by reduction and fixation of the contralateral condyle. Care must be taken not to narrow the trochlea with a lag screw when there is bone loss because this would not allow the arm to sit properly. Because the area for screws is limited in the distal segment, provisional fixation can be used at the joint, with definitive fixation screws passing through the plate to ensure that the screws in the distal segment contribute to the overall stability of the construct (see Fig. 54-45). Newer plates that are precontoured or 3.5-mm compression plates are preferable to one-third tubular and 3.5-mm reconstruction plates because of fatigue failure in the latter group in fractures with metaphyseal comminution. For low-type fractures, additional minifragment plates may provide added fixation (see Fig. 54-45). Locking plates may provide added stability, but there are no clinical studies at this time to support this.If the goal of stable fixation that allows early motion is met, rehabilitation can begin within 3 days of surgery. Waddell et al. showed that disabling stiffness develops if the elbow is immobilized for more than 3 weeks. Supervised physical therapy sessions are scheduled three times a week, along with a daily home exercise program. Dynamic flexion and extension splinting is prescribed when early motion goals are not obtained. Union rates for distal humeral fractures have improved significantly over the years. The most frequent complication is stiffness, which often requires a second procedure. McKee et al. reported an average motion arc of 108 degrees, 74% strength compared with the opposite side, and a mean DASH (Disability of the Arm, Shoulder, and Hand) score of 20 (0 = perfect and 100 = complete disability) in 25 patients at an average 3 years after medial and lateral plate fixation of intraarticular distal humeral fractures. Other complications include ulnar neuropathy, posttraumatic arthritis, osteonecrosis, and symptomatic hardware (see Fig. 54-43). It has been estimated that one in eight patients with operative fixation of a distal humeral fracture eventually requires a second procedure. Many complications can be avoided by the appropriate choice of procedure and meticulous attention to technical details.AFTERTREATMENTThe elbow is splinted in extension. The drain is removed 2 days after surgery, and range of motion is begun3 days after surgery. No bracing is used.Posterior Fracture-Dislocations of the ElbowPosterior fracture-dislocations of the elbow in adults usually are treated surgically because most areunstable owing to the fracture and ligamentous components of the injury. Fracture of the coronoid process or radial head or both can render the elbow significantly unstable after reduction (Fig. 54-48). Untreated injury to the lateral collateral ligamentous complex and medial collateral ligament after repair of the osseous component of the injury can leave residual instability. Lengthy immobilization greatly increases stiffness,and open reduction and stable fixation should be done to allow early motion.These injuries usually result from a fall on the outstretched hand with a shearing component to the injury.Most dislocations are posterior in direction, and fracture of the radial head, radial neck, or coronoid process,or a combination of these, occurs as the proximal ulnar-radial complex is driven posteriorly. Valgus-directed stress can result in avulsion of the medial epicondyle, which is much more common in adolescents. The medial collateral ligament and lateral collateral ligamentous complex are invariably torn.Neurovascular InjuriesFig. 54-48Fracture-dislocation of elbow.A, Posterior fracture-dislocation with irreparable radial head and neck fractures. Type II coronoid fracture is not apparent. This patient's injuries were bilateral and almost identical.B, One elbow has redislocated in posterior splint at 90degrees of elbow flexion. Large radial head fragment and coronoid fracture are readily apparent. Coronoid fracture had to be repaired to provide stability before radial head could be excised.(From Crenshaw AH: Adult fractures and complex joint injuries of the elbow. In Stanley D, Kay NRM, eds: Surgery of the elbow: practical and scientific aspects, London, 1998, Arnold.)l i k u Www .d o c u -tr a c k .c mC c t ob yNO !w w .d o c u -t r a c k .c oInjury of the brachial artery in dislocation of the elbow is a rare but potentially disastrous complication.Arterial injury may range from an intimal tear with delayed occlusion from thrombosis to complete immediate transection. All of these vascular injuries involve stretching of the vessel as the mechanism of injury,especially in closed dislocations.Early recognition is crucial. If arterial flow is not reestablished after closed reduction, the vessel should be reconstructed immediately, using a saphenous vein graft. Arteriograms should be made in the operating room as the patient is being prepared and not in an angiography suite. If treatment has been delayed,forearm fasciotomies are necessary to reduce the chance of compartment syndrome. Howard et al.recommended immediate repair of the brachial artery or reconstruction with a saphenous vein graft for this vascular injury.Because intimal tears can cause delayed arterial thrombosis, all patients with dislocations of the elbowshould be observed closely. Severe swelling is common after reduction, and all patients should bemonitored closely for compartment syndrome.Dislocation of the elbow can damage the median, ulnar, or anterior interosseous nerves. Most such cases involve simple neurapraxia, which resolves quickly. If nerve deficit is present before and after reduction, it is best to wait and observe for signs of resolution. If resolution has not occurred at 3 months, exploration may be needed. Signs of nerve injury that appear after reduction of a dislocation warrant immediate nerveexploration.TreatmentA closed reduction should be performed as soon as possible. Radiographs often are necessary afterreduction to define the osseous injury completely. Three-dimensional CT may be necessary to identify all of the components of this injury. The elbow should be carefully placed through a flexion-extension arc ofmotion. Subluxation or impending dislocation at 30 degrees or more from full extension indicates instability,and surgical stabilization is required. If the elbow is stable, a long-arm posterior splint is applied with the elbow in 90 degrees of flexion. The patient is followed closely, and if subluxation or spontaneousredislocation occurs, the elbow is surgically stabilized. Patients with fracture-dislocations with nondisplaced and stable fracture components are started on early active exercises at 2 to 3 weeks.If surgical intervention is necessary, open reduction and internal fixation of the osseous components areperformed. Regan and Morrey divided fractures of the coronoid process into three types (Fig. 54-49). A type I fracture is a simple avulsion of the tip. A type II fracture involves less than 50% of the coronoid process,and a type III fracture involves more than 50%. Type III and some type II fractures render the elbowextremely unstable, especially if there is an associated fracture of the radial head. Type I and type IIcoronoid fractures are fixed with heavy suture woven into the brachialis and coronoid insertions, passed through two drill holes in the proximal ulna, and tied securely. Type III coronoid fractures are fixed with ascrew using interfragmentary techniques or a coronoid plate (Accumed, Hillsboro, Ore) (Fig. 54-50). Radial head and neck fractures are repaired as described later in the section on fractures of the radial head and fractures of the radial neck.ww .d o c u -t r a c k .c w .d o c u -t r a c k .c oTreatment of radial head and neck fractures associated with elbow dislocations is controversial. The radial head, similar to the coronoid process, is an important stabilizer of the elbow joint. Open reduction andinternal fixation of radial head fractures are preferable to excision if the radial head is salvageable.Josefsson et al. recommend preservation of the radial head, if possible, especially if there is an associated fracture of the coronoid process. If the radial head cannot be preserved, the medial collateral ligament and flexor-pronator mass should be repaired. The elbow should be immobilized in 90 degrees or more of flexion for 3 to 4 weeks and followed closely for redislocation. Broberg and Morrey recommend early, completeexcision of the radial head for type III fractures (see Technique 54-13) and immobilization for no longer than4 weeks. Use of a metallic radial head implant after excision of the radial head is controversial, but should Fig. 54-49Classification of fractures of coronoid process.(From Regan W, Morrey B: Fractures of the coronoid process of the ulna, J Bone Joint Surg 71A:1348, 1989.)Fig. 54-50Coronoid plate for fixation of type III fractures (Accumed, Hillsboro, Ore).ww .d o c u -t r a c k .c w .d o c u -t r a c k .c obe considered if instability is still present after the medial collateral ligament and flexor-pronator mass havebeen repaired. Harrington et al. followed 20 patients who had metallic radial head implants used for grossly unstable elbows. At a mean of more than 12 years, 80% had good-to-excellent results.TECHNIQUE 54-13If radial head excision is necessary, the head is reconstructed on the operative field to ensure that allfragments are removed. If the radial head is excised, the medial collateral ligament and flexor-pronatormass are repaired. If the elbow is still unstable to valgus stress, a radial head prosthesis is fitted as apermanent or temporary spacer. The goal of surgical intervention is a stable elbow, and, if necessary, all structures should be repaired to achieve this.Pugh et al. recommended the following operative treatment protocol, with repair of damaged structures proceeding from deep to superficial through a lateral approach (see Chapter 1): (1) repairing coronoidstability by open reduction and internal fixation of type II and type III fractures; (2) repairing the radial head fracture if possible or replacing with a metal prosthesis; (3) repairing the lateral collateral ligamentouscomplex and secondary constraints (common extensor origin and lateral capsule); and (4) if residualposterior instability remains, repairing the medial collateral ligament and applying a hinged external fixator.The elbow is immobilized in 90 degrees of flexion in a posterior splint. Active motion is started at 2 to 3weeks in a controlled motion brace that limits extension.ComplicationsExcision of the Radial HeadIf this procedure is performed early, relatively good function may be restored in most patients, and only a slight laxity of the lateral side of the elbow joint may remain. Regardless of how carefully the operation is done, the results may not be entirely satisfactory in many patients because rotation may be limited byexcess bone or scar tissue. If not enough bone is removed, or if the operation is delayed until new bone formation is well advanced, a poor result is more likely; motion in the elbow may be markedly limited, or synostosis may develop between the radius and the ulna.• Make an incision along the posterolateral aspect of the shaft of the radius beginning 5 cm distalto the head and extending proximally over the radial head and the lateral humeral condyle.• In the distal part of the incision, carry the dissection down between the extensor carpi ulnarisand the extensor digitorum communis muscles to the periosteum, then proximally over theremains of the radial head, and through the posterior capsule of the joint to the posterior surfaceof the lateral condyle.• An alternative and probably preferable approach to the radial head is through the intervalbetween the anconeus and extensor carpi ulnaris muscles (see Chapter 1).• Remove all loose particles of bone, and thoroughly irrigate the joint of cancellous bone debrisand blood clots.• Reflect the periosteum from the shaft down to the level of the bicipital tuberosity.• Just proximal to the tuberosity, divide the shaft transversely, and remove the head.• Resect the remains of the annular ligament, and excise every particle of periosteum withpainstaking care to limit new bone formation.• Reassemble the removed fragments of the radial head to ensure that none of the fragments hasbeen left behind.• If the articular surface of the radial head cannot be anatomically reassembled, anteroposteriorand lateral radiographs should be made, and a search for the remaining free fragments shouldbe done.• Suture the adjacent soft tissue over the raw end of the bone.• Removal of the annular ligament does not result in significant instability of the upper shaft of theradius. Attempts to leave a portion of the annular ligament intact may result in excision of toosmall a part of the radial head, with subsequent encroachment of the end of the radius on thecapitellum in certain positions of the elbow.l i k u W w w .d o c u -t r a c k .c m C c t o b y NO !w w .d o c u -t r a c k .c oStiffness, recurrent instability, and posttraumatic arthritis are common complications of elbow fracture-dislocation. Anatomical reduction of intraarticular fractures is necessary to prevent arthritic changes. Loss of extension to some degree is expected.Ectopic calcification is common, including calcium deposition in the collateral ligaments and capsule. As Buxton pointed out, however, this condition rarely requires treatment.Heterotopic ossification can cause almost complete ankylosis of the elbow if severe enough (Fig. 54-51). It is common after fracture-dislocations and can be seen on radiographs 3 to 4 weeks after injury. Its severity seems to be associated with the magnitude of the injury and the length of immobilization. Also implicated as a cause is early passive elbow stretching. Rigid fracture fixation, thorough irrigation of soft tissues after fracture repair, and early motion also seem to reduce heterotopic ossification.Although radiation therapy is successful in controlling heterotopic ossification after total hip arthroplasty, as Coventry and Scanlon have shown, it is not suitable after fracture-dislocation of the elbow. The surgical incision cannot be easily isolated from the radiation ports, and wound healing may be compromised.Indomethacin has proved to be effective in reducing postoperative heterotopic ossification around the hip joint, as shown by Ritter and Gioe in total hip arthroplasty and by McLaren in repair of acetabular fractures.Although there are no prospective or retrospective studies related to the elbow, indomethacin can be used to reduce heterotopic ossification.Early resection of heterotopic bone (i.e., before it matures) can greatly increase stiffness because ofreformation. Resection of heterotopic bone to improve motion should be delayed until 12 months after injury.Fig. 54-51Extensive heterotopic ossification after fracture-dislocation of elbow and radial head excision.l i k u W ww .d o c u -t r a c k .c m C c t o b y NO !w w .d o c u -t r a c k .c oOften a functional range of motion can be achieved by then, making resection unnecessary.Copyright © 2008 Elsevier Inc. All rights reserved. - likuWw w .d o c u -t r a c k .c mCct obyNO !w w .d o c u -t r a c k .c o。
中医药名词英文翻译18(中医骨伤科学)

18.001骨折fracture骨的完整性或连续性受到破坏所引起的,以疼痛、肿胀、青紫、功能障碍、畸形及骨擦音等为主要表现的疾病。
18.002损伤injury外界各种创伤因素作用于人体,引起皮肉、筋骨、脏腑等组织结构破坏,及其局部和全身反应疾病的统称。
18.003青枝骨折greenstick fracture仅有部分骨质和骨膜被拉长、皱褶或破裂,常有成角、弯曲畸形,如青嫩的树枝被折断状的一类骨折。
多见于儿童。
18.004裂缝骨折fissured fracture以骨折间隙呈裂缝或线状,骨折片无移位,形似瓷器上的裂纹为主要表现的一类骨折。
18.005锁骨骨折fracture of clavicle锁骨部发生的骨折。
18.006肩胛骨骨折fracture of scapula肩胛骨部发生的骨折。
18.007肱骨外科颈骨折fracture of surgicalneck of humerus以局部肿胀、疼痛、压痛和伤肢纵轴叩击痛,肩关节活动功能障碍,上臂上段可见瘀斑等为主要表现,发生在肱骨解剖颈下2~3cm处的骨折。
18.008肱骨大结节骨折fracture of greatertuberosity of humerus以局部疼痛、肿胀,肩关节活动障碍,尤以肩外展及外旋为甚,活动时疼痛加重,压痛明显,有移位骨折,可扪及异常活动及骨擦音等为主要表现,发生在肱骨大结节部的骨折。
18.009肱骨干骨折fracture of shaft ofhumerus 以患臂肿胀、疼痛、不能抬举,且有明显的压痛和纵轴叩击痛等为主要表现,发生在肱骨外科颈以下至内外髁上2cm处的骨折。
18.010肱骨髁上骨折supracondylar fractureof humerus 以肘部疼痛,肿胀明显甚至有张力水泡,肘部畸形,活动障碍为主要表现,发生在肱骨下端肱骨内、外上髁上方2cm以内的骨折。
18.011肱骨髁间骨折intercondylar fractureof humerus 以肘部肿胀、疼痛、畸形,肘关节呈半屈曲位,前臂旋前,肘部三角关系改变,稍用力掐捏肘部即有骨擦音为主要表现,发生在肱骨内、外髁之间及其邻近部位的骨折。
骨科特殊类型骨折汇总-考博真题
>特殊类型骨折>上肢【bankart骨折】指肩关节盂前下边缘骨折,伴或者不伴有肩前脱位。
【Hill-Sachs损伤】指肱骨头压缩性骨折,当肩关节前脱位时,关节盂前缘撞击导致肱骨头后外侧压缩骨折。
【Holstein —Lewis骨折】肱骨远端1/3骨折伴桡神经嵌压。
【Posadas骨折】经髁的肱骨骨折,伴有骨折碎块向前移位,以及因双髁骨折造成尺桡骨的脱位。
【Kocher骨折】肱骨小头骨折(分四型,I型为Hahn-steinthal骨折;n型为Kocher-lorenz 骨折;山型粉碎性骨折;W型软骨挫伤。
)【Hahn-steinthal骨折】全肱骨小头骨折,为一种少见的关节内骨折,多见于成年人。
【Hume骨折】译休姆【Monteggia骨折】孟氏骨折,指桡骨头脱位合并尺骨骨折。
孟氏骨折孟氏骨折Bado分类(1967)I型:尺骨干骨折向前成角,桡骨头向前脱位,约占60%,石膏固定于屈肘110°,前臂旋后II型:尺骨干骨折向后成角,桡骨头向后脱位,约占15%,石膏固定于屈肘70 °,前臂旋后III型:儿童尺骨近端干骺端骨折合并桡骨头前/外侧脱位,约占20% IV:型尺骨近端1/3骨折,桡骨头脱位。
约占5%。
【Galeazzi骨折】指桡骨干骨折伴下尺桡关节脱位脱位。
【双极骨折】即Monteggia骨折合并Galeazzi骨折.【肘关节恐怖三联征】特指伴有桡骨头和尺骨冠突骨折的肘关节后脱位,属于肘关节内复杂骨折脱位的一种类型。
这类损伤均同时伴有肘内外侧副韧带的撕裂,但不伴有尺骨鹰嘴骨折。
【Essex—Lopresti骨折】指桡骨颈骨折伴有远端尺桡关节分离。
【夜盗(杖)骨折】即尺骨干骨折【警棍骨折】(Night-stick fracture )前臂单纯的尺骨骨折【Colles骨折】Colles骨折指桡骨远端骨折,伴有桡骨远端向背侧的移位,是关节外骨折,常常伴有尺骨茎突骨折。
【Smith骨折】桡骨远端屈曲型骨折,骨折远端向掌侧移位。
精品医学课件-肱骨近端骨折(英文)
Classification
• Neer (4 part)
– 2 part
• AN (anatomic neck) • SN (surgical neck)
– 3 part
• SN+GT, LT
– 4 part
• SN+GT+LT
• Young/Middle age
– nonreconstructable articular surface (severe head split) or extruded anatomic neck
• Elderly
– many 4 parts – some severe 3 parts – most 3,4 part fracture
Proximal Humerus Fractures/Dislocations
History/Demographics
• Bimodal: young-high energy, elderly-low energy(osteoporosis)
• 45% of all humerus fx. • elderly females 4:1
Radiographic Work Up
• Trauma Series
– true scapular AP – axillary (head defects,
displacement of tuberosities
– Y or transscapular
• Other
– modified axillary – AP in int. and ext.
• Displaced d or unstable surgical neck fx
坎贝尔第三卷(英文11版)-肱骨干骨折
Canale & Beaty: Campbell's Operative Orthopaedics,11th ed.Elsevier FRACTURES OF THE HUMERAL SHAFTFractures of the humeral shaft account for roughly 3% of all fractures; most can be treated nonoperatively. Charnley stated, “It is perhaps the easiest of the major long bones to treat by conservative methods.” The range of motion afforded by the shoulder and elbow joints, coupled with a tolerance for small amounts ofshortening, allow radiographic imperfections that cause minimal functional deficit and are well tolerated by the patient. Historically, methods of conservativetreatment have included skeletal traction, abduction casting and splinting, Velpeau dressing, and hanging arm cast, each with its own advantages anddisadvantages.Functional bracing has essentially replaced all other conservative methods and has become the “gold standard” for nonoperative treatment because of its ease of application, adjustability, allowance of shoulder and elbow motion, relatively low cost, and reproducible results. Initially popularized by Sarmiento in 1977, thefunctional brace works on the principles of the hydraulic effect of the brace, active contraction of the muscles, and beneficial effect of gravity. Union rates of 96% to 100% have been reported with this technique. We currently use a coaptation splint or hanging arm cast for the first 7 to 10 days to allow pain to subside and then convert to a prefabricated functional brace. The use of a sling is discouraged to avoid varus and internal rotation deformities. Pendulum exercises are started early,and use of the extremity is encouraged as tolerated, avoiding active shoulder abduction. The brace is worn until the patient is pain-free, and there is radiographic evidence of union. Skin maceration is a concern, so daily hygiene is stressed. Morbid obesity may increase the risk of varus deformities; however, these deformities are more of a cosmetic issue than a functional issue and often are not evident in an obese arm.Sarmiento et al. and Pehlivan reported high union rates with functional bracing of distal-third humeral shaft fractures. We reserve the use of a hanging arm cast for patients in whom compliance or finances preclude the use of a functional brace. Guidelines for acceptable reduction include less than 3 cm of shortening, angulation of less than 20 degrees, and rotation of less than 30 degrees.Operative TreatmentThe choice of operative treatment for a humeral shaft fracture depends on multiple factors. McKee divided the indications for operative treatment into threecategories: (1) fracture indications, (2) associated injuries, and (3) patient indications (Box 54-1). Some indications are more absolute than others. Failure ofconservative treatment, pathological fracture, displaced intraarticular extension, vascular injury, and brachial plexus injury almost always require surgery. Other conditions, such as minimally displaced segmental fractures and obesity, are only relative indications. Our most common indication for operative treatment is early mobilization of patients with polytrauma. Treatment decisions must take all factors into consideration, tailoring the treatment to the specific patient.Box 54-1The goal of operative treatment of humeral shaft fractures is to reestablish length, alignment, and rotation with stable fixation that allows early motion and ideally early weight bearing on the fractured extremity. Options for fixation include plate osteosynthesis, intramedullary nailing, and external fixation. External fixation generally is reserved for high-energy gunshot wounds, fractures with significant soft-tissue injuries, and fractures with massive contamination.Plate OsteosynthesisPlate osteosynthesis remains the “gold standard” of fixation for humeral shaft fractures. Plating can be used for fractures with proximal and distal extension and forIndications for Primary Operative Treatment of Humeral Shaft FracturesFracture IndicationsAssociated InjuriesPatient IndicationsFailure to obtain and maintain adequate closed reductionl i k u W w w .d o c u -t r a c k .c m C c t o b y NO !w w .d o c u -t r a c k .c oopen fractures. It provides enough stability to allow early upper extremity weight bearing in polytrauma patients and produces minimal shoulder or elbow morbidity,as shown by Tingstad et al. Numerous reports in the literature cite high union rates, low complication rates, and rapid return to function after plate fixation of humeral shaft fractures. Five large series (Foster et al., McKee et al., Vander Griend et al., Bell et al., and Tingstad et al.) including 361 fractures had an average union rate of 96.7%.In a prospective, randomized comparison of plate fixation (23 patients) and intramedullary nail fixation (21 patients) of humeral shaft fractures, McCormack et al.found no significant differences in the function of the shoulder and elbow, but shoulder impingement occurred in six patients with intramedullary nailing and only one patient with plating, and a second surgical procedure was required in seven patients with intramedullary nails and only one patient with a plate. These authors concluded that intramedullary nailing may be indicated for specific situations, such as pathological or segmental fractures, but is technically more demanding and has a higher rate of complications than plating. A limitation of this study is that different nailing techniques were used. Flinkkilä et al. compared antegradeintramedullary nailing in 44 patients with plating in 29 and found that although patients had slightly more shoulder pain after intramedullary nailing than after plating,there was no difference in shoulder joint function except for flexion, which was better in patients with plating. Bhandari et al., in a meta-analysis of the literature,pooled data from three randomized trials that included 155 patients to compare intramedullary nailing with compression plating of humeral shaft fractures. They found that reoperation and shoulder impingement were significantly more common after intramedullary nailing.Implant ChoiceThe most commonly used plate for fixation of humeral shaft fractures is the broad, 4.5-mm, limited-contact dynamic compression plate (Fig. 54-28); occasionally, a narrow, 4.5-mm, limited-contact dynamic compression plate is used for smaller bones. The distal metaphyseal-diaphyseal transition zone may require dual 3.5-mm,limited-contact dynamic compression plates (Fig. 54-29) or newer plates designed specifically for the metaphysis. For spiral or oblique fractures, the ideal construct consists of a lag screw with a neutralization plate, whereas transverse fractures are ideally suited for a compression plating technique. In these fractures, attaining provisional reduction with a lag screw, Kirschner wire, or minifragment plate (Eglseder technique) allows direct observation of the reduction and a relatively simple plate application on the reduced humeral shaft (Fig. 54-30).Fig. 54-28Anterior plating of humeral shaft fracture with limited-contact dynamic compression plate.l i k u W w w .d o c u -t r a c k .c m C c t o b y NO !w w .d o c u -t r a c k .c oComminuted fractures may require a bridge plating technique. Anatomical reduction of each fracture fragment is unnecessary. Attaining correct alignment, rotation,and length without disrupting the soft-tissue attachments to the comminuted fragments often leads to successful healing. Livani et al. reported 15 patients withbridge plating done through two small incisions proximal and distal to the fracture; all united within 12 weeks except for a grade III open fracture with an associated brachial plexus injury.In patients with poor bone quality, longer implants should be used to improve stability (Fig. 54-31). Locking plates and screw augmentation with methylmethacrylatehave been reported to add more stability to the construct. Generally, at least eight cortices (four screws) above and below the fracture are necessary to avoid screw pullout with longer implants; more screws may be needed for instability caused by poor bone quality or fracture comminution.Fig. 54-29Dual plating of distal metaphyseal-diaphyseal humeral shaft fracture.Fig. 54-30 A, Oblique humeral shaft fracture.B, After provisional reduction with lag screw and fixation with plate and screws.As minimally invasive plate osteosynthesis has become popular in other long bones, its use for humeral shaft fractures has been suggested; however, risk of injury to the radial nerve has been a concern. Apivatthakakul et al. determined in a cadaver study that with minimally invasive plate osteosynthesis, the plate was 2 to 4.9mm (average 3.2 mm) from the radial nerve. Pronation of the forearm moved the radial nerve closer to the plate by 3 mm. This technique has not been proved in any large series of patients, and we have no experience with it.ApproachNumerous approaches can be used for plate fixation of the humerus. Fractures of the middle or proximal third usually are best approached through an anterolateral approach (brachialis-splitting approach). A posterior approach (triceps-splitting or modified posterior approach) is best for fractures that are midshaft or extend into the distal third of the humerus (Fig. 54-32). Gerwin, Hotchkiss, and Weiland described a modified posterior approach in which the triceps is reflected medially off the lateral intermuscular septum (see Technique 54-6). This approach exposed an average 10 cm more of the humeral shaft than the standard posterior approach. Less frequently, a direct lateral or anteromedial approach may be appropriate.TECHNIQUE 54-6Fig. 54-31 A, Segmental shaft fracture with extension into proximal humerus.B and C,Long plate used to obtain secure fixation.Fig. 54-32 A, Fracture of distal third of humeral shaft.B, After plate fixation through posterior triceps-splitting approach.Open Reduction and Internal Fixation of the Humeral Shaft through a Modified Posterior Approach (Triceps-Reflecting)•PUMPostoperative Care Postoperatively, range of motion of the shoulder and elbow is begun within the first week, and weight bearing usually is allowed if fixation is stable.ComplicationsThe most frequently reported complication after plate fixation of humeral shaft fractures is radial nerve palsy. When using an anterolateral (brachialis-splitting)approach, it is essential to ensure that the nerve is not under the implant during plate application to avoid iatrogenic radial nerve injury. Posteriorly, soft-tissuetethers on the radial nerve can lead to iatrogenic injury. This can be remedied by adequate soft-tissue release off the radial nerve. Infection is reported to occur after 1% to 2% of closed humeral fractures and 5% of open fractures. Refractures occur in approximately 1% of patients. Nonunion of humeral shaft fractures isinfrequent. Treatment of nonunion is discussed in Chapter 56.Intramedullary FixationThe success of intramedullary nailing in the lower extremities led to an initial enthusiasm for intramedullary nailing of the humeral shaft, but without equal success.Although there are many reports in the literature of good results with nailing techniques, problems with insertion site morbidity and union rates have dampened the original enthusiasm for this mode of treatment. Shoulder pain has been reported after antegrade intramedullary nailing in 16% to 37% of patients in more recent studies, and Bhandari et al. found that reoperation and shoulder impingement were significantly more common after intramedullary nailing than after plate fixation.Confounding variables, such as flexible or rigid nails; antegrade or retrograde insertion; and lateral, anterolateral, or extraarticular portal for antegrade insertion,make conclusions difficult to interpret. A large well-controlled trial is needed.Early flexible nails, such as Rush and Enders, provided little axial or rotational stability and required additional forms of stabilization (cerclage wiring or prolonged immobilization) in comminuted or unstable fractures (Fig. 54-34). Even with additional stabilization, the resulting construct generally was not stable enough to allow early motion or weight bearing, especially in multiply-injured patients with concomitant lower extremity injuries. The development of locking nails improved stability and rotational control, but results still did not reach the successful outcomes obtained in lower extremity fractures. Because nail sizes were limited, reaming was required for insertion of most locked nails, and fracture distraction was a problem, especially in small medullary canals. Newer nails come in smaller sizes (7 mm, 8mm, or 9 mm) to fit smaller bones and can be inserted with or without reaming.).Fig. 54-33Open reduction and internal fixation of humeral shaft fracture through modified (triceps-reflecting) posterior approach (see text).A, Incision.B, Incision of fascia to expose intramuscular septum.C,cutaneous nerve.D, Mobilization of radial nerve.E, Bone clamp used to control fragments.F, After débridement, fixation with lag screw.G, After plate application.•CId33C). This usually is at Release the tourniquet.•IdDFrseptum for 3 cm to allow mobilization of the nerve•InPPsoft tissues with t •A transverse fractures where lag screw fixation is diffic technique can be used, or a minifragment plate (Eglseder technique) can be used for provisional fixation, followed by plate fixation.•PCPFig. 54-34Humeral shaft fracture treated by closed intramedullary nailing with multiple flexible intramedullary (Ender) nails.An antegrade approach is most commonly used for intramedullary nail fixation of humeral shaft fractures in adults. The specific portal placement is controversial, however. Traditionally, a midacromial lateral incision was used, which tends to place the nail through the posterior humeral head. In addition, the incision through the rotator cuff is not in line with the fibers of the tendon (see Fig. 54-22). An anterolateral starting portal is collinear with the humeral medullary canal, and the incision is in line with the fibers of the rotator cuff. Several authors have postulated that shoulder pain after antegrade nailing is caused by the transverse incision through the rotator cuff. Alternatives to antegrade humeral nailing (e.g., plate osteosynthesis) should be considered in patients who have preexisting shoulder pathology or who demand upper extremity weight bearing for ambulation (paraplegic or quadriplegic patients).Because of the frequency of shoulder pain after antegrade insertion, retrograde insertion has been advocated to avoid this complication; however, retrograde insertion has been associated with distal humeral fracture propagation. The traditional starting point for retrograde humeral nailing is in the midline, 2 cm above the olecranon fossa. More recently, insertion through the superior aspect of the olecranon fossa has been recommended. Proposed advantages of the olecranon fossa site include an increase in the effective working length of the distal fracture segment and straight alignment with the medullary canal; however, biomechanical studies have shown less resistance to torque and a reduction in load-to-failure with this approach compared with the more superior portal.Although flexible humeral nails have been successful in obtaining fracture union, insertion site morbidity and their suitability for only the most stable fracture patterns have limited their use. Albritton et al., in a cadaver study, found that the axillary nerve was at significant risk during insertion of the interlocking and tension screws of a titanium flexible humeral nail; they recommended blunt dissection through the deltoid, direct observation of the humeral cortex, and use of a soft-tissue sleeve during predrilling and placement of the screws.Newer self-locking expandable nails are reported to be easier to insert, while providing bending and torsional stiffness equal to that of locked nails. Few clinical studies are available to allow evaluation of these nails. Franck et al. described the use of an expandable nail (Fixion; Disc-o-Tech, Herzliya, Israel) for fixation of 25 unstable humeral shaft fractures in elderly patients with osteoporotic bone; all fractures healed without complications. Stannard et al. used a flexible locking nail (Synthes, Paoli, Penn) inserted through an extraarticular antegrade or retrograde portal for fixation of 42 humeral shaft fractures, with healing in 39; 86% had full range of motion, and 90% had no pain. Five complications occurred in four patients: two nonunions, two hardware failures, and one wound infection. All complications occurred in patients whose fractures were fixed with 7.5-mm nails, and the authors recommended that flexible nails should be used with caution in medullary canals with a diameter of 8 mm or less. The technique is technically demanding.Currently, we prefer rigid, locked nails inserted through an antegrade approach when intramedullary nailing is indicated, such as for segmental fractures (see Fig.54-16), for proximal–middle third junction fractures, for pathological fractures, for fractures with poor soft-tissue coverage, for fractures in obese patients, and forfractures in certain patients with polytrauma (Fig. 54-35A to C). We use an anterolateral incision with direct inspection and repair of the rotator cuff. Iatrogenic radialnerve injury has been reported, and care must be taken during fracture reduction, reaming, nail insertion, and locking screw placement. Intramedullary nailing is contraindicated in patients with very narrow medullary canals.TECHNIQUE 54-7Fractures of the Humeral Shaft with Radial Nerve PalsyThe radial nerve is the nerve most frequently injured with fractures of the humeral shaft because of its spiral course across the back of the midshaft of the bone and its relatively fixed position in the distal arm as it penetrates the lateral intermuscular septum anteriorly (Fig. 54-36). Usually the radial nerve injury is a neurapraxia,with recovery rates of 100% in low-energy injuries and 33% in high-energy injuries. Although it is possible for the nerve to be severed by the sharp edge of a bone fragment, this rarely occurs. We treat the fractured humeral shaft in the usual nonoperative manner, support the wrist and fingers with a dynamic splint, and reserve exploration of the nerve for instances when function has not returned in 3 to 4 months and the fracture has healed. Because the nerve usually is only bruised or stretched, function can be expected to return spontaneously. Routine exploration of the nerve would subject many patients to an unnecessary operation and mightincrease the frequency of complications. Early exploration and repair of a severed nerve have not been proved to produce any better results than repair at a laterdate.Fig. 54-35Intramedullary nailing of humeral shaft fracture (see text).A, Segmental shaft fracture in patient with multiple trauma.B and C, After fixation with intramedullary nail.D, Transverse shaft fracture.E and F, Reduction device is used to reduce fracture.G, Reaming is done to 1 to 1.5 mm larger than nail diameter.H, Outrigger device is used for insertion of proximal locking bolts.I, Reduction and screw placement confirmed with fluoroscopy.(D-I courtesy of Thomas A. Russell, MD, Memphis, Tenn.)•Carefully evaluate preoperative radiographs (Fig. 54-35D) to ensure that the diaphyseal diameter is adequate to accommodate the intramedullary nail; if the diameter is too small, plate fixation is indicated.• Position the patient on a radiolucent table with the thorax “bumped” 30 to 40 degrees. Place the image intensifer unit on the opposite side of the tablefrom the surgeon (see Fig. 54-21); rolling the unit back allows an adequate anteroposterior view, and rolling it forward allows an adequate lateral viewof the shoulder and humerus.• Make an incision diagonally from the anterolateral corner of the acromion, splitting the deltoid in line with its fibers in the raphe between the anteriorand middle thirds of the deltoid (see Fig. 54-22). To protect the axillary nerve, avoid splitting the deltoid more than 5 cm distal to the acromion.• Under direct observation, incise the rotator cuff in line with its fibers (see Fig. 54-22A). Use full-thickness sutures to protect the cuff from damageduring reaming of the humeral canal.• Place the initial guidewire posterior to the biceps tendon, and advance it under fluoroscopic guidance into the appropriate position as shown onanteroposterior and lateral views (see Fig. 54-21).• Carefully advance the proximal reamer, protecting the rotator cuff.• Use the reduction device to reduce the fracture and pass the bead-tipped guidewire (Fig. 54-35E and F). With sequentially larger reamers, ream thehumerus to the predetermined diameter, usually 1 to 1.5 mm larger than the nail diameter (Fig. 54-35G). With fractures of the middle third of theshaft, a small incision can be made at the fracture site to ensure manually that the radial nerve is not entrapped in the fracture before reduction andreaming.• When reaming is complete, pass the nail down the humeral canal, avoiding distraction of the fracture; ensure that the nail is below the articularsurface of the humeral head.• With the use of the outrigger device, insert the proximal locking bolts (Fig. 54-35H). Carefully spread the soft tissues to avoid injury to the axillarynerve.• Place the distal interlocking screws in an anterior-to-posterior direction to avoid the radial nerve. Make a 4- to 5-cm incision anteriorly to expose thebiceps musculature; bluntly split the muscle to avoid iatrogenic damage to the brachial artery.• Repair the rotator cuff with full-thickness sutures.•Confirm reduction and screw length on anteroposterior and lateral fluoroscopy images (Fig. 54-35I).• Begin an early rehabilitation program with active-assisted range-of-motion exercises.If radial nerve palsy occurs with an open fracture of the humeral shaft, the nerve should be explored at the time of the irrigation and débridement of the wound. If it is found intact, only watchful waiting is required while the fracture heals. Early exploration is required if evidence suggests that the radial nerve is impaled on a bone fragment or is caught between the fragments. Advances in ultrasonography have been useful in diagnosing entrapped and lacerated radial nerves. If this diagnostic tool proved to be reproducible in large numbers of patients, the indications for nerve exploration would be more specifically defined.In patients with radial nerve palsy for whom operative treatment of a humeral shaft fracture is indicated, the nerve should be explored at the time of fracture fixation.Shao et al. reviewed 21 scientific articles that included 4517 humeral shaft fractures and found an overall prevalence of radial nerve palsy of almost 12% (n = 532).Radial nerve palsy was most frequent with fractures of the middle and middle–distal humeral shaft and was more common with transverse and spiral fractures than with oblique or comminuted fractures. Overall, recovery occurred in 88%. Complete transection of the radial nerve usually occurs with open fractures of the humerus and requires nerve repair or grafting; most nerve palsies that occur with a closed fracture recover without treatment. Based on their review, Shao et al. developed an algorithm for the treatment of radial nerve palsy associated with humeral shaft fractures (Fig. 54-37).Periprosthetic Humeral Shaft Fractures Fig. 54-36Entrapment of radial nerve between fragments in spiral fracture of distal third of humerus.A, Nerve is least mobile as it passes through lateral intermuscular septum in distal third of arm.B, Oblique fracture is typically angulated laterally, and distal fragment is displaced proximally. Radial nerve, fixed to proximal fragment by lateral intermuscular septum, is trapped between fragments when closed reduction is attempted.(Redrawn from Holstein A, Lewis GB: Fractures of the humerus with radial-nerve paralysis, J Bone Joint Surg 45A:1382, 1963.)Fig. 54-37Treatment algorithm for radial nerve palsy associated with humeral shaft fracture. EMG, electromyogram; NAP, nerve axonal physiology; NCV, nerve conduction velocity.(From Shao YC, Harwood P, Grotz MR, et al: Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review, J Bone Joint Surg 87B:1647, 2005.)Periprosthetic humeral shaft fractures after shoulder or elbow arthroplasty are rare, but can be difficult to treat. Poor bone stock from osteoporosis, osteomalacia, or rheumatoid arthritis is the major contributing factor, and a variety of fracture patterns can result from low-energy direct blows, minor twisting injuries, “same level”falls, or intraoperative technical errors. Fractures around humeral arthroplasties may occur at the tuberosity level, metaphysis, upper diaphysis around the stem, or distal to the stem tip. Fractures around the humeral component of total elbow arthroplasties also can occur at any level from the medial or lateral column to proximal to the stem tip.Stable postoperative fractures without component loosening can be treated conservatively with immobilization. Stable fractures with component loosening require revision immediately or after fracture healing if still painful. Unstable fractures with or without component loosening require operative fixation with or withoutcomponent revision. If revision is necessary, the general principles of revision arthroplasty should be followed (see Chapters 8). Bone quality determines the need for supplemental allograft, strut grafts, methylmethacrylate cement, or autogenous bone grafts. Most patients requiring either hemiarthroplasty or total shoulder arthroplasty or elbow arthroplasty have age-related osteoporosis.When treating unstable periprosthetic humeral shaft fractures with well-fixed components, we have found the following guidelines helpful as outlined by Cameron and Iannotti: (1) displaced tuberosity fractures should be repaired with wire or heavy suture, and associated rotator cuff tears should be treated; (2) unstablediaphyseal fractures around or below the prosthesis require open reduction and internal fixation. Cerclage wire or limited screw fixation is unsatisfactory. A heavy plate with proximal cerclage wires and distal screws is preferred. At least four proximal cables and four distal screws, engaging eight cortices, are necessary. We recommend using 2-mm cables instead of the usual 1.6-mm cables. An anatomical reduction is necessary for union, and bone grafting the fracture site should be considered.When poor bone quality is present, fixation can be supplemented with methylmethacrylate cement. Cement should be kept out of the fracture site. If severeosteopenia is present, we recommend adding a full-thickness cortical allograft strut applied with additional cables 90 degrees to the plate-cable-screw construct.Autograft bone should be applied to the fracture site. We do not believe that a well-fixed, good functional shoulder or elbow arthroplasty should be revised to a long-stem implant just to repair a postoperative shaft fracture. Results with revision shoulder and elbow arthroplasty are not as satisfactory as primary arthroplasty.Instead we believe every effort should be made to achieve primary fracture union.Intraoperative fractures during shoulder arthroplasty can be avoided by careful attention to detail and respect for osteopenic bone. Intraoperative fractures should be repaired at the time of surgery by internal fixation or revision to a longer stem implant. The review by Cameron and Iannotti should be consulted for furtherinformation.The general treatment principles of periprosthetic humeral fractures around the humeral component of total elbow arthroplasties are as just outlined. Fractures of the medial or lateral column with a firmly seated implant can be treated with immobilization. Union of a column fracture is unnecessary for a good functional outcome.Copyright © 2008 Elsevier Inc. All rights reserved. - ww .d o c u -t r a c k .c w .d o c u -t r a c k .c o。
各种骨折英文名称
Aviator骨折:是距骨的骨折,在第一次世界大战期间被描述,是一种水平压力造成的骨折。
Barton骨折:累及橈骨远端尖节面移位骨折,可能发生腕矢节半脱位,骨折线可以发生在背侧或掌侧。
Bennett骨折:第1掌骨基底的斜形骨折,掌骨近端形成轴向移位,掌侧边缘形成三角形的骨碎片。
Bosworth骨折:腓骨远端骨折伴有胫骨脊近端后外的骨碎片。
Boxer骨折:第5掌骨颈骨折伴有掌骨头向掌侧移位。
Burst骨折椎体轴向压力造成的骨折,通常发生骨折碎片向外侧的移位。
可以发生在颈椎、胸椎或腰椎。
Chance骨折:胸腰段椎体的分离性骨折,伴随脊髓、神经根、椎体的水平方向的崩裂骨折。
Chauffeur骨折:橈骨干的斜形骨折,早期有机械性弯曲,进而通过逆性外力造成的斜形骨折。
Chopart骨折:骨折或移位累及足的Chopart尖节。
Clay-shoveler骨折:下颈椎或上胸椎脊柱序列的骨折,损伤是由于工人企图向上扔一满铁铲的泥土,但是泥土粘住铁铲,引起一个突然的屈曲力量反作用于颈部引起的损伤。
Colles骨折:橈骨远端骨折的一般术语,伴有挠骨远端向背侧的移位,可以有或没有尺骨干的骨折。
Cotton骨折:是指伴有双踝及后踝的三踝骨折。
Die-punch骨折:远端橈骨的尖节内骨折,伴有月骨陷窝背侧表面的压迫。
Dupuytren骨折:腓骨远端骨折伴有远端胫腓韧带断裂,以及距骨侧方移位。
Duverney骨折:骼骨翼的骨折,但么有骨盆环的分离移位。
Essex-Lopresti骨折:梯骨颈骨折伴有远端尺橈尖节分离。
Galeazzi骨折:楼骨远端1/3骨折伴有尺骨远端半脱位。
Greenstick骨折:儿童的不完全性骨折,伴有骨折的压力侧部分皮质和骨膜的连接。
Hangman骨折:骨折通过第2颈椎椎体(轴位)神经弓。
Hill-Sachs骨折:后外侧肱骨头压缩性骨折,是由于前方矢节盂移位或肱骨碰撞前方矢节盂边缘引起。
Holstein —Lewis骨折:肱骨远端1/3骨折伴橈神经嵌压。
骨科相关英语

骨科 ORTHOPEDICS1、概论 INTRODUCTION*fracture n.骨折pathological fracture 病理骨折fatigue fracture 疲劳骨折*open fracture 开放骨折close fracture 闭合骨折*comminuted fracture粉碎性骨折compressed fracture 压缩骨折shock n.休克*deformity n.畸形tenderness n.压痛swelling n.肿胀ecchymosis n.瘀斑obstacle n.功能障碍*bonefascial compartment syndrome 骨筋膜室综合征infection n.感染spinal cord injury 脊髓损伤surrounding nerve 周围神经*fat embolism 脂肪栓塞bedsore n.褥疮arthroclisis n.关节僵硬ischemic necrosis 缺血性坏死ischemic contraction 缺血性挛缩*traumatic arthritis 创伤性关节炎hematoma n.血肿*callus n.骨痂heal n.愈合*synovitis n.滑膜炎*ligament n.韧带*tendon n.肌腱* pyogenic osteomyelitis 化脓性骨髓炎*reduction n.复位*bone traction 骨牵引*osteoporosis n.骨质疏松2、上肢骨折FRACTURE OF UPPER EXTREMITIES clavicle n.锁骨*humerus n.肱骨*rotation n.旋转supracondyle n.髁上blister n.水疱pulsate n.搏动thrombus n.血栓*cancellous n.松质骨*epiphysis n.骨骺*injury n.损伤*joint n.关节stability n.稳定ulna n.尺骨radius n.桡骨metacarpal bone 掌骨bone graft 植骨hemostasis 止血*periosteum n.骨膜tension n.张力adhesion n.粘连*skin grafting 植皮*arthrodesis n.关节融合extrusion n.挤压gangrene n.坏疽pallor n.苍白、灰白*amputation n.截肢plaster n.石膏paralysis n.瘫痪bandage n.绷带2、手外伤 HAND TRAUMAavulsion n.撕脱*dislocation n.脱位stiff adj.僵硬3、下肢骨折与关节损伤 FRACTURE OF LOWER EXTREMITIES AND ARTICULAR INJURYfemur n.股骨adduction n.内收separate v.分离cartilage n.软骨*synovialis n.滑膜*spinal column 脊柱5、脊柱及骨盆骨折 FRACTURE OF VERTEBRAL COLUMN AND PELVIS column n.椎体cervical column 颈椎*lumber vertebra 腰椎sacrum n.骶椎sense n.感觉movement n.运动reflect v.反射*pelvis n.骨盆6、关节脱位 ARTICULAR DISLOCATIONcongenital dislocation 先天性脱位pathological dislocation 病理性脱位*osteoarthritis n.骨关节炎*total hip replacement 全髋置换术7、运动系统慢性损伤 CHRONIC STRAIN OF MOVEMENT SYSTEM strain n.劳损*cystis n.滑囊*stenosed tenosynovitis 狭窄性腱鞘炎*ganglion n.腱鞘囊肿degenerative adj.退行性变multiply v.增生abnormal sense 感觉异常8、腰腿痛和颈肩痛LUMBAGO AND SHOULDER PAINSstenosed column 椎管狭窄9、骨与关节化脓感染OSTEOARTICULAR PURULENT LNFECTION channel n.窦道drill hole 钻孔*drainage n.引流10、骨与关节结核 OSTEOARTICULAR TUBERCULOSISbone tuberculosis 骨结核spinal cord compression 脊髓压迫11、骨肿瘤BONE TUMORbone tumor 骨肿瘤*osteochondroma n.骨软骨瘤*osteosarcoma n.骨肉瘤chemotherapy n.化疗*synoviosarcoma n.滑膜肉瘤医学英语分科常用词汇人体解剖学 HUMAN ANATOMY之运动系统 LOCOMOTOR SYSTEM 1、中轴骨 AXIAL BONES*bone n.骨*vertebrae n.椎骨*cervical vertebrae 颈椎*thoracic vertebrae 胸椎lumbar vertebrae 腰椎*sacrum n.骶骨coccyx 尾骨atlas n.寰椎axis n.枢椎*sternum n.胸骨sternal angle 胸骨角sternal manubrium 胸骨柄xiphoid process 剑突*rib n.肋*thoracic cage 胸廓2、颅SKULL*skull n.颅*frontal bone 额骨*parietal bone 顶骨*occipital bone 枕骨*temporal bone 颞骨*sphenoid bone 蝶骨*ethmoid bone 筛骨*mandible n.下颌骨hyoid bone 舌骨vomer n.犁骨*maxilla n.上颌骨palatine bone 腭骨nasal bone 鼻骨lacrimal bone 泪骨inferior nasal concha 下鼻甲zygomatic bone 颧骨*coronal suture冠状缝*sagital suture 矢状缝*lambdoid suture 人字缝orbit n.眶cranial fontanelle 颅囟2、附肢骨TARSAL BONES AND EXTREMITAL BONES *clavicle n.锁骨*scapula n.肩胛骨*humerus n.肱骨*radius n.桡骨*ulna n.尺骨carpal bone 腕骨metacarpal bone 掌骨phalanges n.指骨,趾骨*hip bone 髋骨*ilium n.髂骨*ischium n.坐骨*pubis n.耻骨*femur n.股骨patella n.髌骨*tibia n.胫骨*fibula n.腓骨tarsal bone 跗骨metatarsal bone 跖骨4、关节学 ARTHROLOGY*articulation n.关节*ligament n.韧带*flexion n.屈*extension n.伸*adduction n.收*medial rotation 旋内*lateral rotation 旋外pronation n旋前.supination n.旋后circumduction n.环转*vertebral column脊柱*thoracic cage 胸廓*intervertebral disc 椎间盘*temporal-mandibular joint 颞下颌关节*shoulder joint 肩关节*elbow joint 肘关节*radiocarpal joint 桡腕关节*pelvis n.骨盆*hip joint 髋关节*knee joint 膝关节*ankle joint 踝关节5、肌肉系统 MUSCULATURE(1)肌学系统INTRODUCTION OF MUSCULATURE *muscle n.肌肉muscle belly 肌腹tendon n.肌腱aponeurosis n.腱膜*fascia n.筋膜*tendinous sheath 腱鞘(2)躯干肌TRUNK MUSCLEStrapezius n.斜方肌latissimus dorsi 背阔肌erector spinae 竖脊肌*sternocleidomastoid adj.胸锁乳突的*scalenus n.斜角肌pectoralis major 胸大肌intercostales n.肋间肌*diaphragm n.膈(肌)*inguinal canal 腹股沟管*sheath of rectus abdominis 腹直肌鞘(3)头肌 HEAD MUSCLESorbicularis oculi 眼轮匝肌masseter n.咬肌*temporalis n.颞肌*deltoid n.三角肌*biceps brachii 肱二头肌*triceps brachii 肱三头肌*axillary fossa 腋窝(4)附肢肌 MUSCLES ATTACHED TO EXTREMITTES *gluteus maximus 臀大肌piriformis n.梨状肌*sartorius n.缝匠肌*quadriceps femoris 股四头肌triceps surae 小腿三头肌*femoral triangle 股三角popliteal fossa 腘窝医学英语分科常用词汇诊断学——骨关节系统OSTEOARTICULAR SYSTEM*Codman’striangle 骨膜三角,科德曼三角H-shaped vertebra,butterfly vertebra 蝴蝶椎Rugger-Jersay vertebra 夹心椎体Scheuermann’s disease 绍尔曼病Schmorl’s nodule 施莫尔结节Shenton’s lin e 沈通氏线apophysis n. 骺状突*arthrography n.关节造影basilar impression,basilarinvagination 颅底凹陷block vertebra 融合椎bone island 骨岛bursography n.泪囊造影compacta n.骨密度cortical porosity 皮质骨疏松症craniolacunia,luckenschadel n.颅骨陷窝*empty sella 空蝶鞍endosteal proliferation 骨内膜增生*epiphysis n.骨骺Intratrabecular resorption 骨小梁内吸收ivory vertebra 象牙椎marrow-packing disease 骨髓充填疾病massive osteolysis 大片骨溶解melopheostosis n.蜡油骨症ossification n.骨化osteopathia striata 纹骨症*osteopenia n.骨质减少osteopetrosis n.石骨症osteopoikilosis n.斑骨症pars interarticularis 椎弓峡部periosteal reaction 骨膜反应physis n.骨生长端*pseudofracture, Looser zone n.假骨折spina ventosa 骨气鼓spongiosa 骨疏松woven bone 编织骨*zone of provisional calcification 临时钙化带骨科专业英语Abduction splint 外展石膏Absorbable screws 可吸收螺钉Acetabulum 髋臼Amputation 截肢Analgesic 止痛药Ankle clonus 踝阵挛Ankylosing spondylitis 强直性脊柱炎Annulus 纤维环Arthroscopy 关节镜检查Asteofascial compartment syndrome 骨筋膜室综合症Atrophy of quadriceps femoral 股四头肌萎缩A vascular necrosis ofA vascular necrosis (A VW) 缺血性坏死Bathesthesia 深感觉Bilateral femoral head 双股骨头缺血坏死Bone traction 骨牵引Bowel and bladder dysfunction 二便障碍Brachial plexus anesthesia 臂丛麻醉Bunion 拇囊炎Capitula fibula 腓骨小头Cerclage (骨折端)环扎法Cerclage bandage 环形绷带Cerebral hemorrhage 脑出血Cerebral thrombosis 脑血栓Cervical spondylosis 颈椎病Clavicle fracture 锁骨骨折Closed suction drains 闭式引流Colle’s Fracture 科雷氏骨折Comminuted fracture of left** 左***粉碎性骨折Comminuted open fracture of talus 距骨的开放粉碎骨折Common peroneal nerve 腓总神经Congenital kyphoscoliosis 先天性侧后凸畸形congenital scoliosis 先天性脊柱侧凸Conscious mind 神志清楚Continuous epidural anesthesia (连)硬外麻Contracture of both 臀肌挛缩Core compression 髓芯减压术Crossed kirschner fixation 交叉固定DAS 动力型髋螺丝钉Debridement 清创Deformity 畸形Defuts of segmentation 分布障碍Decompression 减压Decompression of spinal canal 椎管减压Diastematomyelia 脊髓纵裂Discectomy 椎间盘摘除Discectomy of hemivertebrae 半椎体切除Dislocation 脱位DM 糖尿病Dorsal artery of foot 足背动脉Elastic fixation 弹性固定End vertebra 端椎Extension 伸External fixture 外固定Emergency case 急诊病例Faciotomy 筋膜切除术Femoral neck 股骨颈Femoral neck fracture 股骨颈骨折Figure of 8 bandage 8字绷带Flexion 屈曲Forklike deformity 餐叉样畸形Fracture 骨折Fracture of alner bone 尺骨骨折Fracture of calcaneus 跟骨骨折Fracture of distal phalange 远端趾骨骨折Fracture of distal radius 桡骨远端骨折Fracture of femoral neck 股骨颈骨折Fracture of great tubercle 肱骨大结节骨折of humurusFracture of proximal femor 股骨近端骨折Fracture of phalange 指骨骨折Fracture of radius 桡骨骨折Fracture of the base ofFracture of the scaphoid 舟状骨骨折Fracture of the ulna 尺骨骨折Fracture of ulna ocleranon 尺骨鹰嘴骨折General anesthesia 全麻General surgical 基本外科Gleniod fossa 关节盂Gluteal musclesGreater tuberosity 大结节Helo-pelvis 头颅环-骨盆环Hallux valgus 拇外翻Hallux varus 拇内翻High fever 高热Hilgenreiner’s angle 髋臼指数(acetabular index)Hemopneumothorax 血气胸Humeral head 肱骨头Humeral shaft fracture 肱骨干骨折Hypertrophy of facet 小关节增生肥大Hypoesthesia 感觉减退Ice bag 冰袋In right elbow joint 右肘肿物切除Incomplete paraplegia 不全瘫Injection 肌肉注射Interbody 椎间体Interlocking medullary mailing 带锁髓内针Intermittent claudication 间歇跛行Internal fixation 内固定术Intertrochanteric fracture 粗隆间骨折Intramscular hematoma 肌间血肿Intrumedullary needleJonalgia 膝痛Kyphoscoliosis 侧后凸Kyphosis 脊柱后凸laminectomy 椎板切除术Lateral meuleouls 外踝lipoma 脂肪瘤Local anesthesia 局麻Lodorsis 脊柱前凸Lower limb (extremuty) 下肢Mc Murrag’s test麦氏实验Medial malleouls 内踝Metacarpophalangeal joint 掌指关节Metastaluc tumor 转移癌metastatic 转移瘤Metatarsalgia 柘骨痛Metatarsal fracture 跟骨骨折Myelogram 脊髓造影Nifedipine 心痛定Nitroglyccerin 硝酸甘油Numbness 麻木Old fracture 陈旧性骨折Osteoarthritis 骨关节炎Osteochondrdoma 软骨瘤Osteomyelitis 骨髓炎Paralytic scoliosis 麻痹性脊柱侧弯Paraplegia 截瘫Patellar fracture 髌骨骨折Pathologie diagnosis 病理诊断pediculate 椎弓根PercutaneousPhlebothrombosis 下肢静脉血栓Pilon fracture 胫腓骨下端骨折Plaster slab 石膏托Poliomyelitis 脊髓灰质炎Posterior malleolus fracture 后踝骨折Posterior malleolar fracture 后踝骨折Protrusion of intervertebral 腰椎间盘突出Protrusion of intervertebral disc 腰椎间盘突出Prolapsed intervertebral disc 椎间盘脱出Pubic symphysis 耻骨支Pulmanary function 肺功能Pulpous nuclear 髓核Radial head fracture 桡骨头骨折Radius and ulna 尺、桡骨Reduction by leverage 撬拨复位Regular operation 常规手术Resection of the massSacroiliac 骶髂关节Scholiosis 脊柱侧弯Sciatica 坐骨神经痛Sciatica 坐骨神经痛Sequela of poliomyelitis 小儿麻痹(脊髓灰质炎)后遗症Sinus tract 窦道Skin traction 皮牵引Sling(Triangular bandage) 悬吊(三角巾绷带)Spatula 压舌板Spinal stenosis 椎管狭窄Spondylolisthesis 脊柱滑脱Spondylolisthesis of lumber L4-5 L4-5脊柱滑脱Spondytolysis 蛱部裂Staticfixation 静力性固定Stenosis of Spinal Canal 椎管狭窄Stenosis of the lumbar spine 腰椎管狭窄Sublimation/semiluxation 半脱位Subluxation of ankle joint 踝关节半脱位subtrochanteric fracture 粗隆下骨折supracondylar fracture 踝上骨折suture stitch 缝针synovial membrance 滑膜Syringomyelia 脊髓空洞症Taction 触觉Tension band wire 张力带钢丝Tension bond 张力带Tetraplegia / quadriplegia 四肢瘫The fifth metacarple bone 第五掌骨基底骨折Thermesthesia 温度觉Tibia-talus semidislocation 半脱位Tibial fracture 胫骨骨折Tibial plateau fracture 胫骨平台骨折Total knee arthroplasty 全膝置换Total hip arthroplasty 全髋置换Trimalleolar fracture 三踝骨折Urinary incontinence 尿失禁V algus muscle strength 外翻肌力V eterbera fracture 椎体骨折。
骨科英文词汇

骨科 ORTHOPEDICS1、概论 INTRODUCTION*fracture n.骨折pathological fracture 病理骨折fatigue fracture 疲劳骨折*open fracture 开放骨折close fracture 闭合骨折*comminuted fracture粉碎性骨折compressed fracture 压缩骨折shock n.休克*deformity n.畸形tenderness n.压痛swelling n.肿胀ecchymosis n.瘀斑obstacle n.功能障碍*bonefascial compartment syndrome 骨筋膜室综合征infection n.感染spinal cord injury 脊髓损伤surrounding nerve 周围神经*fat embolism 脂肪栓塞bedsore n.褥疮arthroclisis n.关节僵硬ischemic necrosis 缺血性坏死ischemic contraction 缺血性挛缩*traumatic arthritis 创伤性关节炎hematoma n.血肿*callus n.骨痂heal n.愈合*synovitis n.滑膜炎*ligament n.韧带*tendon n.肌腱* pyogenic osteomyelitis 化脓性骨髓炎*reduction n.复位*bone traction 骨牵引*osteoporosis n.骨质疏松2、上肢骨折FRACTURE OF UPPER EXTREMITIESclavicle n.锁骨*humerus n.肱骨*rotation n.旋转supracondyle n.髁上blister n.水疱pulsate n.搏动thrombus n.血栓*cancellous n.松质骨*epiphysis n.骨骺*injury n.损伤*joint n.关节stability n.稳定ulna n.尺骨radius n.桡骨metacarpal bone 掌骨bone graft 植骨hemostasis 止血*periosteum n.骨膜tension n.张力adhesion n.粘连*skin grafting 植皮*arthrodesis n.关节融合extrusion n.挤压gangrene n.坏疽pallor n.苍白、灰白*amputation n.截肢plaster n.石膏paralysis n.瘫痪bandage n.绷带2、手外伤 HAND TRAUMAavulsion n.撕脱*dislocation n.脱位stiff adj.僵硬3、下肢骨折与关节损伤FRACTURE OF LOWEREXTREMITIES AND ARTICULARINJURYfemur n.股骨adduction n.内收separate v.分离cartilage n.软骨*synovialis n.滑膜*spinal column 脊柱5、脊柱及骨盆骨折 FRACTUREOF VERTEBRAL COLUMN ANDPELVIScolumn n.椎体cervical column 颈椎*lumber vertebra 腰椎sacrum n.骶椎sense n.感觉movement n.运动reflect v.反射*pelvis n.骨盆6、关节脱位 ARTICULARDISLOCATIONcongenital dislocation 先天性脱位pathological dislocation病理性脱位*osteoarthritis n.骨关节炎*total hip replacement 全髋置换术7、运动系统慢性损伤 CHRONICSTRAIN OF MOVEMENT SYSTEMstrain n.劳损*cystis n.滑囊*stenosed tenosynovitis 狭窄性腱鞘炎*ganglion n.腱鞘囊肿degenerative adj.退行性变multiply v.增生abnormal sense 感觉异常8、腰腿痛和颈肩痛LUMBAGOAND SHOULDER PAINSstenosed column 椎管狭窄9、骨与关节化脓感染OSTEOARTICULAR PURULENTLNFECTIONchannel n.窦道drill hole 钻孔*drainage n.引流10、骨与关节结核OSTEOARTICULARTUBERCULOSISbone tuberculosis 骨结核spinal cord compression 脊髓压迫11、骨肿瘤BONE TUMORbone tumor 骨肿瘤*osteochondroma n.骨软骨瘤*osteosarcoma n.骨肉瘤chemotherapy n.化疗*synoviosarcoma n.滑膜肉瘤医学英语分科常用词汇人体解剖学 HUMAN ANATOMY之运动系统 LOCOMOTORSYSTEM1、中轴骨 AXIAL BONES*bone n.骨*vertebrae n.椎骨*cervical vertebrae 颈椎*thoracic vertebrae 胸椎lumbar vertebrae 腰椎*sacrum n.骶骨coccyx 尾骨atlas n.寰椎axis n.枢椎*sternum n.胸骨sternal angle 胸骨角sternal manubrium 胸骨柄xiphoid process 剑突*rib n.肋*thoracic cage 胸廓2、颅SKULL*skull n.颅*frontal bone 额骨*parietal bone 顶骨*occipital bone 枕骨*temporal bone 颞骨*sphenoid bone 蝶骨*ethmoid bone 筛骨*mandible n.下颌骨hyoid bone 舌骨vomer n.犁骨*maxilla n.上颌骨palatine bone 腭骨nasal bone 鼻骨lacrimal bone 泪骨inferior nasal concha 下鼻甲zygomatic bone 颧骨*coronal suture冠状缝*sagital suture 矢状缝*lambdoid suture 人字缝orbit n.眶cranial fontanelle 颅囟2、附肢骨TARSAL BONES ANDEXTREMITAL BONES*clavicle n.锁骨*scapula n.肩胛骨*humerus n.肱骨*radius n.桡骨*ulna n.尺骨carpal bone 腕骨metacarpal bone 掌骨phalanges n.指骨,趾骨*hip bone 髋骨*ilium n.髂骨*ischium n.坐骨*pubis n.耻骨*femur n.股骨patella n.髌骨*tibia n.胫骨*fibula n.腓骨tarsal bone 跗骨metatarsal bone 跖骨4、关节学 ARTHROLOGY*articulation n.关节*ligament n.韧带*flexion n.屈*extension n.伸*adduction n.收*medial rotation 旋内*lateral rotation 旋外pronation n旋前.supination n.旋后circumduction n.环转*vertebral column脊柱*thoracic cage 胸廓*intervertebral disc 椎间盘*temporal-mandibular joint颞下颌关节*shoulder joint 肩关节*elbow joint 肘关节*radiocarpal joint 桡腕关节*pelvis n.骨盆*hip joint 髋关节*knee joint 膝关节*ankle joint 踝关节5、肌肉系统 MUSCULATURE(1)肌学系统INTRODUCTION OFMUSCULATURE*muscle n.肌肉muscle belly 肌腹tendon n.肌腱aponeurosis n.腱膜*fascia n.筋膜*tendinous sheath 腱鞘(2)躯干肌TRUNK MUSCLEStrapezius n.斜方肌latissimus dorsi 背阔肌erector spinae 竖脊肌*sternocleidomastoid adj.胸锁乳突的*scalenus n.斜角肌pectoralis major 胸大肌intercostales n.肋间肌*diaphragm n.膈(肌)*inguinal canal 腹股沟管*sheath of rectus abdominis腹直肌鞘(3)头肌 HEAD MUSCLESorbicularis oculi 眼轮匝肌masseter n.咬肌*temporalis n.颞肌*deltoid n.三角肌*biceps brachii 肱二头肌*triceps brachii 肱三头肌*axillary fossa 腋窝(4)附肢肌 MUSCLESATTACHED TO EXTREMITTES*gluteus maximus 臀大肌piriformis n.梨状肌*sartorius n.缝匠肌*quadriceps femoris 股四头肌triceps surae 小腿三头肌*femoral triangle 股三角popliteal fossa 腘窝医学英语分科常用词汇诊断学——骨关节系统OSTEOARTICULAR SYSTEM*Codman’striangle 骨膜三角,科德曼三角H-shapedvertebra,butterflyvertebra 蝴蝶椎Rugger-Jersay vertebra 夹心椎体Scheuermann’s disease 绍尔曼病Schmorl’s nodule 施莫尔结节Shenton’s line 沈通氏线apophysis n. 骺状突*arthrography n.关节造影basilarimpression,basilarinvagina tion 颅底凹陷block vertebra 融合椎bone island 骨岛bursography n.泪囊造影compacta n.骨密度cortical porosity 皮质骨疏松症craniolacunia,luckenschade l n.颅骨陷窝*empty sella 空蝶鞍endosteal proliferation 骨内膜增生*epiphysis n.骨骺Intratrabecular resorption 骨小梁内吸收ivory vertebra 象牙椎marrow-packing disease 骨髓充填疾病massive osteolysis 大片骨溶解melopheostosis n.蜡油骨症ossification n.骨化osteopathia striata 纹骨症*osteopenia n.骨质减少osteopetrosis n.石骨症osteopoikilosis n.斑骨症pars interarticularis 椎弓峡部periosteal reaction 骨膜反应physis n.骨生长端*pseudofracture, Looser zone n.假骨折spina ventosa 骨气鼓spongiosa 骨疏松woven bone 编织骨*zone of provisional calcification 临时钙化带。
骨科专业英语[解说]
![骨科专业英语[解说]](https://img.taocdn.com/s3/m/719d71c329ea81c758f5f61fb7360b4c2e3f2a61.png)
骨科ORTHOPEDICS1、概论INTRODUCTION*fracture n.骨折pathological fracture 病理骨折fatigue fracture 疲劳骨折*open fracture 开放骨折close fracture 闭合骨折*comminuted fracture粉碎性骨折compressed fracture 压缩骨折shock n.休克*deformity n.畸形tenderness n.压痛swelling n.肿胀ecchymosis n.瘀斑obstacle n.功能障碍*bonefascial compartment syndrome 骨筋膜室综合征infection n.感染spinal cord injury 脊髓损伤surrounding nerve 周围神经*fat embolism 脂肪栓塞bedsore n.褥疮arthroclisis n.关节僵硬ischemic necrosis 缺血性坏死ischemic contraction 缺血性挛缩*traumatic arthritis 创伤性关节炎hematoma n.血肿*callus n.骨痂heal n.愈合*synovitis n.滑膜炎*ligament n.韧带*tendon n.肌腱* pyogenic osteomyelitis 化脓性骨髓炎*reduction n.复位*bone traction 骨牵引*osteoporosis n.骨质疏松2、上肢骨折FRACTURE OF UPPER EXTREMITIES clavicle n.锁骨*humerus n.肱骨*rotation n.旋转supracondyle n.髁上blister n.水疱pulsate n.搏动thrombus n.血栓*cancellous n.松质骨*epiphysis n.骨骺*injury n.损伤*joint n.关节stability n.稳定ulna n.尺骨radius n.桡骨metacarpal bone 掌骨bone graft 植骨hemostasis 止血*periosteum n.骨膜tension n.张力adhesion n.粘连*skin grafting 植皮*arthrodesis n.关节融合extrusion n.挤压gangrene n.坏疽pallor n.苍白、灰白*amputation n.截肢plaster n.石膏paralys is n.瘫痪bandage n.绷带2、手外伤HAND TRAUMAavulsion n.撕脱*dislocation n.脱位stiff adj.僵硬3、下肢骨折与关节损伤FRACTURE OF LOWER EXTREMITIES AND ARTICULAR INJURYfemur n.股骨adduction n.内收separate v.分离cartilage n.软骨*synovialis n.滑膜*spinal column 脊柱5、脊柱及骨盆骨折FRACTURE OF VERTEBRAL COLUMN AND PELVIScolumn n.椎体cervical column 颈椎*lumber vertebra 腰椎sacrum n.骶椎sense n.感觉movement n.运动reflect v.反射*pelvis n.骨盆6、关节脱位ARTICULAR DISLOCATION congenital dislocation 先天性脱位pathological dislocation 病理性脱位*osteoarthritis n.骨关节炎*total hip replacement 全髋置换术7、运动系统慢性损伤CHRONIC STRAIN OF MOVEMENT SYSTEMstrain n.劳损*cystis n.滑囊*stenosed tenosynovitis 狭窄性腱鞘炎*ganglion n.腱鞘囊肿degenerative adj.退行性变multiply v.增生abnormal sense 感觉异常8、腰腿痛和颈肩痛LUMBAGO AND SHOULDER PAINSstenosed column 椎管狭窄9、骨与关节化脓感染OSTEOARTICULAR PURULENT LNFECTIONchannel n.窦道drill hole 钻孔*drainage n.引流10、骨与关节结核OSTEOARTICULAR TUBERCULOSISbone tuberculosis 骨结核spinal cord compression 脊髓压迫11、骨肿瘤BONE TUMORbone tumor 骨肿瘤*osteochondroma n.骨软骨瘤*osteosarcoma n.骨肉瘤chemotherapy n.化疗*synoviosarcoma n.滑膜肉瘤医学英语分科常用词汇人体解剖学HUMAN ANATOMY之运动系统LOCOMOTOR SYSTEM1、中轴骨AXIAL BONES*bone n.骨*vertebrae n.椎骨*cervical vertebrae 颈椎*thoracic vertebrae 胸椎lumbar vertebrae 腰椎*sacrum n.骶骨coccyx 尾骨atlas n.寰椎axis n.枢椎*sternum n.胸骨sternal angle 胸骨角sternal manubrium 胸骨柄xiphoid process 剑突*rib n.肋*thoracic cage 胸廓2、颅SKULL*skull n.颅*frontal bone 额骨*parietal bone 顶骨*occipital bone 枕骨*temporal bone 颞骨*sphenoid bone 蝶骨*ethmoid bone 筛骨*mandible n.下颌骨hyoid bone 舌骨vomer n.犁骨*maxilla n.上颌骨palatine bone 腭骨nasal bone 鼻骨lacrimal bone 泪骨inferior nasal concha 下鼻甲zygomatic bone 颧骨*coronal suture冠状缝*sagital suture 矢状缝*lambdoid suture 人字缝orbit n.眶cranial fontanelle 颅囟2、附肢骨TARSAL BONES AND EXTREMITAL BONES*clavicle n.锁骨*scapula n.肩胛骨*humerus n.肱骨*radius n.桡骨*ulna n.尺骨carpal bone 腕骨metacarpal bone 掌骨phalanges n.指骨,趾骨*hip bone 髋骨*ilium n.髂骨*ischium n.坐骨*pubis n.耻骨*femur n.股骨patella n.髌骨*tibia n.胫骨*fibula n.腓骨tarsal bone 跗骨metatarsal bone 跖骨4、关节学ARTHROLOGY*articulation n.关节*ligament n.韧带*flexion n.屈*extension n.伸*adduction n.收*medial rotation 旋内*lateral rotation 旋外pronation n旋前.supination n.旋后circumduction n.环转*vertebral column脊柱*thoracic cage 胸廓*intervertebral disc 椎间盘*temporal-mandibular joint 颞下颌关节*shoulder joint 肩关节*elbow joint 肘关节*radiocarpal joint 桡腕关节*pelvis n.骨盆*hip joint 髋关节*knee joint 膝关节*ankle joint 踝关节5、肌肉系统MUSCULATURE(1)肌学系统INTRODUCTION OF MUSCULATURE *muscle n.肌肉muscle belly 肌腹tendon n.肌腱aponeurosis n.腱膜*fascia n.筋膜*tendinous sheath 腱鞘(2)躯干肌TRUNK MUSCLEStrapezius n.斜方肌latissimus dorsi 背阔肌erector spinae 竖脊肌*sternocleidomastoid adj.胸锁乳突的*scalenus n.斜角肌pectoralis major 胸大肌intercostales n.肋间肌*diaphragm n.膈(肌)*inguinal canal 腹股沟管*sheath of rectus abdominis 腹直肌鞘(3)头肌HEAD MUSCLESorbicularis oculi 眼轮匝肌masseter n.咬肌*temporalis n.颞肌*deltoid n.三角肌*biceps brachii 肱二头肌*triceps brachii 肱三头肌*axillary fossa 腋窝(4)附肢肌MUSCLES ATTACHED TO EXTREMITTES*gluteus maximus 臀大肌piriformis n.梨状肌*sartorius n.缝匠肌*quadriceps femoris 股四头肌triceps surae 小腿三头肌*femoral triangle 股三角popliteal fossa 腘窝医学英语分科常用词汇诊断学——骨关节系统OSTEOARTICULAR SYSTEM*Codman’striangle 骨膜三角,科德曼三角H-shaped vertebra,butterfly vertebra 蝴蝶椎Rugger-Jersay vertebra 夹心椎体Scheuermann’s disease 绍尔曼病Schmorl’s nodule 施莫尔结节Shenton’s line 沈通氏线apophysis n. 骺状突*arthrography n.关节造影basilar impression,basilarinvagination 颅底凹陷block vertebra 融合椎bone island 骨岛bursography n.泪囊造影compacta n.骨密度cortical porosity 皮质骨疏松症craniolacunia,luckenschadel n.颅骨陷窝*empty sella 空蝶鞍endosteal proliferation 骨内膜增生*epiphysis n.骨骺Intratrabecular resorption 骨小梁内吸收ivory vertebra 象牙椎marrow-packing disease 骨髓充填疾病massive osteolysis 大片骨溶解melopheostosis n.蜡油骨症ossification n.骨化osteopathia striata 纹骨症*osteopenia n.骨质减少osteopetrosis n.石骨症osteopoikilosis n.斑骨症pars interarticularis 椎弓峡部periosteal reaction 骨膜反应physis n.骨生长端*pseudofracture, Looser zone n.假骨折spina ventosa 骨气鼓spongiosa 骨疏松woven bone 编织骨*zone of provisional calcification 临时钙化带。
骨科常见英语词汇
骨科英语词汇Achilles Tendonitis 跟腱炎Ruptured Achilles Tendon 跟腱破裂Ankle Sprain 踝部扭伤Ankle Fracture 踝部骨折Ankylosing Spondylitis 强直性脊柱炎Aseptic Necrosis 无菌性坏死Baker's Cyst 贝克囊肿Bone Tumors 骨肿瘤Carpal tunnel syndrome 腕管综合症Colles Fracture 桡骨下端骨折Compression Fracture of the Vertebrae 脊椎压缩性骨折Dislocation 脱位Tennis Elbow 网球肘Fibromyalgia 纤维组织肌痛Flat Foot 扁平足Hammer Toe 锤状趾Plantar Fasciitis 足底筋膜炎Clavicle Fracture 锁骨骨折Frozen Shoulder 冷冻肩Ganglion 腱鞘囊肿Hand Fracture 手骨折Heel Spurs 脚跟骨刺Herniated Disk 椎间盘突出Arthritis of the Hip 髋关节炎T otal hip replacement全髋关节置换术Total knee replacement全膝关节置换术Femoral neck fracture股骨颈骨折骨折I ntertrochanteric fracture粗隆间骨折Infectious Arthritis 感染性关节炎Knee Arthritis 膝关节炎Meniscus tear 半月板撕裂Mallet Finger 锤状指Morton Neuroma 莫耳通氏神经瘤Muscular Dystrophy 肌肉萎缩症Wry Neck 颈部僵硬Osteoarthritis 骨关节炎(退化性关节炎)Osteomalacia 软骨病Osteomyelitis 骨髓炎Osteoporosis 骨质疏松症Paget Disease Paget氏病Ribs and Cartilage Inflammation 肋与软骨炎Sciatica 坐骨神经痛Kyphosis 脊柱侧弯Scoliosis 脊柱侧弯Shoulder Dislocation 肩脱位Rotator Cuff Tear 肩袖损伤Swollen 肿胀Bursitis 滑囊炎Tenosynovitis 腱鞘炎Trigger Finger 扳机指Acetabulum 髋臼Amputation 截肢Analgesic 止痛药Arthroscopy 关节镜检查Osteofascial compartment syndrome骨筋膜室综合症Avascular necrosis of femoral head 股骨头缺血性坏死Bone traction 骨牵引Bowel and bladder dysfunction 二便障碍Brachial plexus anesthesia 臂丛麻醉Bunion 拇囊炎Cervical spondylosis 颈椎病Common peroneal nerve 腓总神经Congenital kyphoscoliosis 先天性侧后凸畸形Congenital scoliosis 先天性脊柱侧凸Contracture of both 臀肌挛缩Core decompression 髓芯减压术Debridement 清创Decompression of spinal canal 椎管减压Discectomy 椎间盘摘除Discectomy of hemivertebrae 半椎体切除Dorsal artery of foot 足背动脉Extension 伸直External fixture 外固定Faciotomy 筋膜切除术Femoral neck 股骨颈Flexion 屈曲Forklike deformity 餐叉样畸形Fracture of uln a r bone 尺骨骨折Fracture of calcaneus 跟骨骨折Fracture of distal phalange 远端趾骨骨折Fracture of distal radius 桡骨远端骨折Fracture of greater tuberosity of humerus 肱骨大结节骨折Fracture of proximal femur 股骨近端骨折Fracture of phalange 指骨骨折Fracture of radius 桡骨骨折Scapular glenoid fracture肩胛骨骨折Glenoid fossa 关节盂Hallux valgus 拇外翻Hallux varus 拇内翻Humeral head 肱骨头Humeral shaft fracture 肱骨干骨折Immobilization 制动Ice bag 冰袋Intermittent claudication 间歇跛行Intramscular hematoma 肌间血肿Intrumedullary needle 髓内针Kirschner wire 克氏针lipoma 脂肪瘤Mc Murray’s test 麦氏实验Meniscectomy 半月板切除Metacarpophalangeal joint 掌指关节Osteochondroma 软骨瘤Osteomyelitis 骨髓炎Paraplegia 截瘫Patellar fracture 髌骨骨折Plaster slab 石膏托Poliomyelitis 脊髓灰质炎Posterior malleolus fracture 后踝骨折Protrusion of intervertebral disc 腰椎间盘突出Reduction 复位Retinaculum 支持带Revision 翻修Sacroiliac 骶髂关节Sinus tract 窦道Skin traction 皮牵引Spondylolisthesis 脊柱滑脱Stenosis of Spinal Canal 椎管狭窄lumbar spinal stenosis 腰椎管狭窄Subluxation 半脱位subtrochanteric fracture 粗隆下骨折supracondylar fracture 髁上骨折synovial chondromatosis 滑膜软骨瘤病Syringomyelia 脊髓空洞症Tension band 张力带Tibial fracture 胫骨骨折Tibial plateau fracture 胫骨平台骨折Total knee arthroplasty 全膝置换Total hip arthroplasty 全髋置换Trimalleolar fracture 三踝骨折。
骨折分型参照表
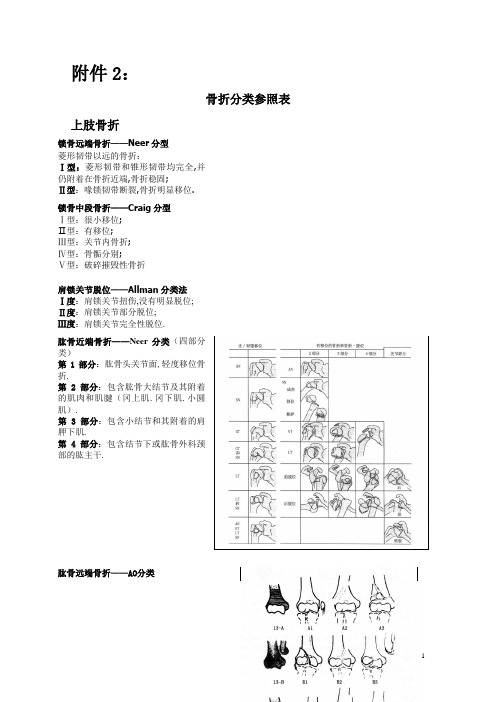
附件2:骨折分类参照表上肢骨折锁骨远端骨折——Neer分型菱形韧带以远的骨折:Ⅰ型:菱形韧带和锥形韧带均完全,并仍附着在骨折近端,骨折稳固;Ⅱ型:喙锁韧带断裂,骨折明显移位.锁骨中段骨折——Craig分型Ⅰ型:很小移位;Ⅱ型:有移位;Ⅲ型:关节内骨折;Ⅳ型:骨骺分别;Ⅴ型:破碎摧毁性骨折肩锁关节脱位——Allman分类法Ⅰ度:肩锁关节扭伤,没有明显脱位;Ⅱ度:肩锁关节部分脱位;Ⅲ度:肩锁关节完全性脱位.肱骨近端骨折——Neer分类(四部分类)第1部分:肱骨头关节面,轻度移位骨折.第2部分:包含肱骨大结节及其附着的肌肉和肌腱(冈上肌.冈下肌.小圆肌).第3部分:包含小结节和其附着的肩胛下肌.第4部分:包含结节下或肱骨外科颈部的肱主干.肱骨远端骨折——AO分类A关节外骨折A1骨突撕脱:a外上髁;b内上髁,无箝卡型;c内上髁,箝卡型;A2单纯干骺部骨折:a斜行向内向下型;b 斜行向外向下型;c横行;A3干骺部多块骨折:a楔形骨块相连;b破碎摧毁的楔形骨块;c复合型;B部分关节骨折B1外侧矢状位:a肱骨小头;b单纯经滑车型;c经滑车多块骨片型;B2内侧矢状位:a单纯经滑车型,经由内测;b单纯经滑车型,经滑车沟;c经滑车多块骨片型;B3冠状位:a小头;b滑车;c小头加滑车C全关节型骨折C1单纯关节类,单纯干骺部型:a轻度移位型;b重度移位型;c骨骺部T型骨折;C2单纯关节类,骨骺部多块骨片型:a横行骨片相连;b多块横行骨片型;c复合型;C3多块骨片型:a单纯干骺部型;b干骺部横行骨块;c干骺部复合型肱骨小头骨折——Bryan-Morrey分类I型:小头完全骨折;II型:小头部分骨折;III型:小头破碎摧毁骨折.尺骨鹰嘴骨折——Colton分型Ⅰ型:撕脱骨折Ⅱ型:斜行骨折Ⅲ型:横行骨折Ⅳ型:斜行伴随破碎摧毁骨折Ⅴ型:破碎摧毁性骨折Ⅵ型:骨折脱位尺骨冠状突骨折——Regan-Morrey分型Ⅰ型:单纯的冠状突尖端撕脱;Ⅱ型:简略或破碎摧毁性骨折,伤及冠状突少于50%;Ⅲ型:简略或破碎摧毁性骨折,伤及冠状突的50%以上.桡.尺骨远端骨折——Compbell分类法1.未进入关节的桡骨下端骨折:向掌侧成角及向背侧移位的称为Colles骨折;项背侧成角及向掌侧移位的称为Smith骨折.2.桡骨远端关节面背侧边沿骨折:伴随腕关节向背侧脱位或半脱位称为背侧Barton 骨折;桡骨远端关节面掌侧边沿骨折,伴随腕关节向掌侧脱位或半脱位称为掌侧Barton 骨折.桡骨头骨折(改进Mason分型)I型:小的或边沿骨折,骨折无移位;II型:边沿骨折有分别移位;III型:破碎摧毁或明显移位的骨折,包含明显移位的桡骨颈骨折.胸锁关节脱位按脱位的偏向可分为:1.前脱位;2.后脱位(罕有)孟氏骨折——Bado分型I型(前侧型或伸展型):尺骨骨折向前成角,桡骨头向前脱位;II型(后侧型或愚昧型):尺骨骨折向后成角,桡骨头向后脱位;III型(外侧型或内收型):尺骨近干骺端骨折,桡骨头向外脱位;IV型(特别型):桡骨头向前脱位,尺桡骨近双骨折.盖氏骨折(Galeazzi骨折,Compbell称之为“必须骨折”)按照骨折的稳固程度及移位偏向,临床上可分为三类:1.稳固型:桡骨远端青枝骨折归并尺骨小头骨骺分别,均为儿童,此型毁伤较轻,易于整复.2.不稳固型:桡骨下1/3骨折,骨折可为横型.短斜形.斜形.短缩移位明显,下尺桡关节脱位明显.多为摔倒时手掌撑地致伤,前臂旋前位致伤时桡骨远折段向背侧移位,前臂旋后位致伤时桡骨远折段向掌侧移位,临床上以掌侧移位者多见.此型毁伤较重,下尺桡关节掌背侧韧带.三角纤维软骨盘多已断裂,骨间膜亦有必定的毁伤.3.特别型:尺桡主干双骨折伴下尺桡关节脱位.多为机械绞轧伤所致,毁伤重,此时除下尺桡关节掌.背侧韧带,三角纤维软骨盘多断裂外,骨间膜多有轻微毁伤.凋谢性骨折——Gustilo分型Ⅰ型:伤口<1cm的凋谢骨折,伤口很清洁,最可能系由骨折尖端自内向外刺伤皮肤所致,没有挤压和软组织毁伤;Ⅱ型:伤口>1cm,软组织毁伤普遍;形成皮瓣或扯破,轻到中度挤压伤,但没有软组织普遍撕脱或挤压,有轻度污染;Ⅲ型:所有归并轻微软组织毁伤和污染的凋谢骨折,包含皮肤.肌肉.神经血管普遍毁伤:分三个亚型.ⅢA型:有普遍的软组织毁伤,但完全清创后,骨折仍有优越的软组织笼罩,伤口可延期愈合;ⅢB型:有更普遍的软组织毁伤,骨膜掀起或骨袒露,必须行肌瓣笼罩,伴轻微污染;ⅢC型:所有归并有动脉毁伤的凋谢骨折,假如要保存肢体必须修复毁伤的动脉.闭合骨折—软组织毁伤Tscherne分型0级:直接暴力导致的骨折,软组织毁伤可以疏忽不计;Ⅰ级:骨折概况的软组织有从内向外的力导致的轻度擦伤或挤压伤;Ⅱ级:有明显的肌肉挤压伤,可以有重度污染的皮肤擦伤;Ⅲ级:皮肤有普遍的碾搓伤,皮肤与肌肉分别或撕脱,伴随轻微的肌肉伤害,常归并有动脉毁伤和筋膜距离分解征.呈轻微破碎摧毁骨折.下肢骨折骨盆骨折——Tile分类法A型:没有累及骨盆环的撕脱骨折,骨盆后部和顶部的骨和韧带保持完全.1型:撕脱骨折:1.1撕脱骨折;1.2髂嵴骨折;1.3坐骨结节骨折.2型:髂骨骨折:2.1髂骨翼骨折;2.2单侧前弓骨折;2.3双侧前弓骨折.3型:骶骨横型骨折:3.1骶尾骨折;3.2无移位的骶骨骨折;3.3有移位的骶骨骨折.B型:骨盆环没有完全断裂,骶髂后韧带和骨间韧带仍完全.1型:外旋力致伤的“翻书”骨折,或经由过程耻骨结合分别或前骨盆环骨折的前部凋谢毁伤,后骶髂韧带和骨间韧带保持完全:1.1耻骨结合分别<2.5cm,骶脊韧带完全;1.2耻骨结合分别>2.5cm,骶脊韧带和前骶髂韧带断裂;1.3双侧骨折.2型:内旋力致伤的侧方挤压骨折:2.1同侧前后毁伤;2.2对侧(桶柄)毁伤.3型:双侧毁伤.C型:扭转和垂直均不稳固骨折,包含造成后部韧带复合体断裂的垂直剪力和前方挤压毁伤,骨盆后环完全断裂.1型:单侧骨折:1.1髂骨骨折;1.2骶骨骨折脱位;1.3骶骨骨折.2型:双侧骨折,个中一侧为B型骨折,一侧为C型骨折.3型:双侧完全不稳固骨折.骶骨骨折——Denis分类法Ⅰ型:位于骶神经孔的外侧,骨折线经由过程骶骨翼;Ⅱ型:骨折经骶神经孔;Ⅲ型:位于骶神经孔内侧(中心侧),包含横行骨折.髋臼骨折——Letournel-Judet分类1.简略骨折型:累及髋臼一个壁或柱,同时有横型骨折,又包含后壁.后柱.前壁或前柱骨折和横型骨折.2.归并骨折型:包含T型骨折.后柱和后壁的横型骨折和后部骨折的结合骨折.后部半横型骨折和前柱骨折及双柱骨折的结合骨折.髋脱位——Thompson-Epstein分类Ⅰ型:脱位归并稍微骨折或无骨折;Ⅱ型:脱位归并髋臼后壁大块简略骨折;Ⅲ型:脱位归并髋臼后壁破碎摧毁骨折,可有或无大块骨折;Ⅳ型:脱位归并髋臼顶骨折;Ⅴ型:脱位归并股骨头骨折.股骨头骨折——Pipkin分类法Ⅰ型:髋关节后脱位归并头凹下方的股骨头骨折;Ⅱ型:髋关节后脱位归并头凹上方的股骨头骨折;Ⅲ型:Ⅰ型或Ⅱ型髋关节后脱位归并股骨头骨折;Ⅳ型:Ⅰ型.Ⅱ型或Ⅲ型髋关节后脱位归并髋臼骨折.股骨颈骨折——Garden分类法Ⅰ度:不完全嵌插骨折,头向后外侧竖直;Ⅱ度:完全骨折,但无移位;Ⅲ度:完全骨折,有部分移位(经由过程火干间骨小梁偏向剖断).但骨折端仍然互相接触;Ⅳ度:完全骨折,完全移位,股骨头内骨小梁同髋臼内骨小梁从新分列.转子间骨折——Evans 分类法Ⅰ型:骨折线从小粗隆向外.向上延长: Ⅰa 型:骨折无移位,小粗隆无骨折;Ⅰb 型:骨折有移位,小粗隆有骨折,但复位后内侧皮质能附着,骨折稳固;Ⅰc 型:骨折有移位,小粗隆有骨折,但复位后内侧骨皮质不克不及附着,骨折仍不稳固;Ⅰd 型:破碎摧毁骨折至少包含大小粗隆4部分骨折块.骨折不稳固;Ⅱ型:骨折线自小粗隆斜向外下方,骨折不稳固,骨折远端常向内移位.转子间骨折——AO 分类法A1:单纯骨折,即两部分骨折: 1.骨折线延长至粗隆间线; 2.骨折线经由过程大粗隆; 3.骨折线位于小粗隆下部.A2:骨折线延长至内侧骨皮质两处以上: 1.有一内侧骨块; 2.稀有块内侧骨块;3.向小粗隆下延长超出1cm.A3:骨折经由过程股骨外侧皮质: 1.近端.斜行; 2.简略.横行; 3.破碎摧毁.转子下骨折(股骨近端)——AO 分类法股骨下端骨折——Müller 分型(即AO)依据骨折部位及骨折程度分型:A型:关节外骨折,骨折仅累及股骨远端主干(髁上),可有不合程度破碎摧毁:A1型:单纯螺旋形关节外骨折:①骨突骨折;②干骺端斜型或螺旋型骨折;③干骺端横型骨折;A2型:关节外干骺端T形骨折,①完全楔形骨折;②外侧破碎摧毁骨折;③内侧破碎摧毁骨折;A3型:关节外干骺端破碎摧毁骨折,①伴一块内侧劈裂骨折;②无纪律,骨折限于干骺端;③无纪律,骨折延至主干;B型骨折:部分关节内骨折,骨折累及髁部:B1型:部分关节内骨折,股骨外髁矢状劈裂骨折:①简略骨折,经髁间窝;②简略骨折,经负重面;③破碎摧毁骨折;B2型:部分关节内骨折,股骨内髁矢状劈裂骨折:①简略骨折,经髁间窝;②简略骨折,经负重面;③破碎摧毁骨折;B3型:冠状骨折:①前外侧小片骨折;②后侧单髁骨折;③后侧双髁骨折;C型:完全关节内骨折,T型或Y型髁间骨折:C1型:关节内简略骨折,干骺端简略骨折,骨折无破碎摧毁性骨折,①T型及Y型,轻度移位②T型及Y型,明显移位③T型骨骺骨折C2型:股主干破碎摧毁骨折归并两个重要的关节骨块C3型:关节内破碎摧毁性骨折髌骨骨折——按骨折线外形分类1.横行骨折:累及髌骨中1/3部分,有时也累及高低极.2.垂直骨折:累及髌骨中外1/3部分,假如只有髌骨的内侧或外侧缘受累,称为边沿骨折.,平日归并有移位.股骨头坏逝世——Marcus分类Ⅰ期:髋无症状,X线片仅在股骨头前方承重部位有黑点状稍微密度增高(点状密度增高);Ⅱ期:有分界明显的骨梗逝世区,其基底部可见密度增高的边沿;Ⅲ期:股骨头稍变平或可见透亮的“新月征”(系软骨下骨小梁与软骨分别或塌陷现象);Ⅳ期:缺血部明显塌陷,股骨头球面中止,在骨坏逝世区的边沿可见到关节面骨折;Ⅴ期:有髋关节退行性关节炎表示,关节间隙变窄,在股骨头软骨下骨质和髋臼承重部分可见小骨赘和囊性变;Ⅵ期:有明显的退行性转变,关节间隙变窄,股骨头塌陷.胫骨平台骨折——Schatzker分类法Ⅰ型:单纯楔形骨折或劈裂骨折,典范的单纯的楔形骨块通胫骨分别,轻度向外.向下移位; Ⅱ型:劈裂和紧缩结合骨折,外侧楔形骨块分别,且关节面被压入干骺端Ⅲ型:单纯中间紧缩骨折,关节面塌陷,外侧皮质完全;Ⅳ型:内髁骨折,胫骨嵴常受累,骨折趋于向内翻位;Ⅴ型:双髁骨折,胫骨两个平台均有劈裂,但干骺端和主干仍然持续;Ⅵ型:有干骺端和主干分别的平台骨折,胫骨近端可为横行或斜行骨折,同时有一个或两个髁及关节面骨折.胫骨下端Pilon骨折—Rüedi-Allgöwer分类Ⅰ型:仅累及关节面的骨折,骨折线有分别但无移位;Ⅱ型:仅累及关节面的骨折,骨折线分别且有移位;但无或轻度破碎摧毁;Ⅲ型:骨折累及干骺端和关节面,且为破碎摧毁性骨折.骨骺毁伤——Salter-Harris分类Ⅰ型:单纯骨骺分别,有或内有移位;Ⅱ型:骨骺分别经由过程骨骼,有一干骺端骨块仍附着在分别的骨骺上;Ⅲ型:骨骺分别,并有一经由过程骨骺的骨折线进入关节,当骨折有移位时关节关系转变;Ⅳ型:骨折经由过程干骺端.骨骼.骨骺,并进入关节,有可能消失关节关系转变;Ⅴ型:骨骺紧缩骨折.踝关节骨折——Lauge-Hansen分类旋后-内收型(SA):Ⅰ度:外踝韧带断裂或外踝撕脱骨折,外踝骨折低于踝关节程度间隙;Ⅱ度:第Ⅰ度加内踝骨折.旋后-外旋型(SER):Ⅰ度:下胫腓前韧带断裂或胫骨前结节撕脱骨折;Ⅱ度:第Ⅰ度加外踝鄙人胫腓结合程度位于冠状面自前下向后上的斜形骨折;Ⅲ度:第Ⅱ度加后踝骨折;Ⅳ度:第Ⅲ度加内踝骨折或三角韧带断裂. 旋前-外展型(PA):Ⅰ度:内踝撕脱骨折或三角韧带断裂;Ⅱ度:第Ⅰ度加下胫腓韧带部分或全体毁伤;Ⅲ度:第Ⅱ度加外踝鄙人胫腓结合稍上方之短斜形骨折或伴随小蝶形片的破碎摧毁骨折,蝶形骨折片常位于外侧.Dupuytren骨折脱位是一种少见的旋前-外展型毁伤,即腓骨高位骨折.胫骨下端腓骨切迹部位撕脱骨折.三角韧带断裂同时有下胫腓分别.旋前-外旋型(PER):Ⅰ度:内踝撕脱骨折或三角韧带断裂;Ⅱ度:第Ⅰ度加下胫腓前韧带.骨间韧带断裂,如下胫腓前韧带保持完全也可产生胫骨远端前结节撕脱骨折(Tillaux骨折);Ⅲ度:第Ⅱ度加腓骨鄙人胫腓结合程度以上的短螺旋形或斜形骨折;Ⅳ度:第Ⅲ度中下胫腓后韧带断裂,导致下胫腓分别,如下胫腓后韧带保持完全也可产生后踝撕脱骨折.垂直紧缩型(PD):1.单纯垂直紧缩外力骨折依受伤时踝及足所处地位不合分为背伸型毁伤-胫骨下端前缘紧缩骨折.跖屈型毁伤-胫骨下端后缘紧缩骨折以及垂直毁伤-胫骨下端破碎摧毁骨折,常同时有腓骨下端的破碎摧毁骨折或斜形骨折;2.复合垂直紧缩外力骨折分为垂直外力与外旋外力复合引起者,多见于旋后-外旋型骨折中;垂直外力与内收外力复合引起者,胫骨下端内侧呈破碎摧毁或明显紧缩骨折;垂直外力与外展外力复合引起者,胫骨下端外侧呈明显紧缩骨折,腓骨下端呈破碎摧毁骨折.跟骨骨折——Essex-lopresti没进入距下关节的骨折:A.跟骨体纵行骨折,但距下关节完全;B.跟骨体上缘骨折(鸟嘴形骨折);C.载距突骨折;D.跟骨体骨折,骨折线接近距下关节,但没进入关节内;影响到距下关节的骨折:E.舌型骨折;F.关节紧缩骨折跟骨骨折CT分类——Sander分类Ⅰ型:所有没有移位的关节骨折,不管骨折线的数目若干;Ⅱ型:所有跟骨后关节面的两部分骨折,依据重要骨折线的部位分为Ⅱa.Ⅱb.Ⅱc三个亚型;Ⅲ型:所有跟骨后关节面的三部分骨折,中间骨块下沉,依据重要骨折线的部位分为Ⅲa.Ⅲb.Ⅲc三个亚型;Ⅳ型:所有四部分骨折,轻微破碎摧毁骨折,常有4块以上骨块.距骨颈骨折——Hawkins分类体系Ⅰ型:距骨颈无移位的垂直骨折;Ⅱ型:骨折有移位,距下关节有半脱位或脱位;Ⅲ型:距下关节和踝关节均有脱位;Ⅳ型:距下关节和踝关节均有脱位,骨折块脱出.足舟骨骨折——Sangeorzan分类Ⅰ型:由沿着足的中间轴进行的外力引起.骨折线一般为横行,将舟骨分为背跖两部分;Ⅱ型:骨折线从背外侧到跖.内侧走行,常归并距舟关节半脱位或脱位;Ⅲ型:常损坏舟骰关节,舟骨的内侧或外侧部分常有紧缩,罕有破碎摧毁.移位型骨折,并有骰骨.跟骨和跟骰关节毁伤同时消失.半月板毁伤——O’Connor分类法Ⅰ型:纵行扯破;Ⅱ型:程度扯破,毁伤可将半月板分层;Ⅲ型:斜行扯破;Ⅳ型:放射状扯破;Ⅴ型:其他,包含瓣状扯破.完全扯破和退行性扯破等.主干骨折——AO分型肱主干骨折——AO分型A简略骨折A1螺旋形简略骨折A2斜形简略骨折(≥30°)A3横断简略骨折(<30°)B楔形骨折Bl螺旋楔形骨折B2 曲折楔形骨折B3 碎裂楔形骨折C 庞杂骨折Cl 螺旋庞杂骨折C2 多段庞杂骨折C3 无纪律庞杂骨折尺桡主干骨折——AO分型A简略骨折A1.尺骨骨折桡骨完全(A13伴桡骨头脱位Monteggia);A2.桡骨骨折尺骨完全(A23伴下尺桡关节脱位)A3.尺桡骨简略双骨折.B楔形骨折B1. 尺骨楔形骨折桡骨完全;B2. 桡骨楔形骨折尺骨完全;B3. 一骨楔形骨折,另一骨楔形或简略骨折.C庞杂骨折C1. 尺骨庞杂骨折,桡骨完全;C2. 桡骨庞杂骨折;C3. 尺桡骨双骨庞杂骨折.胫骨骨折——AO分类法A1 螺旋形;A2. 斜形(≥30°); A3 横断(<30°). B.楔形骨折B1 螺旋楔形;B2 曲折楔形;B3 破碎摧毁楔形.C1 有二个内侧骨块; C2 多段;C3 不规矩.。
骨科英语
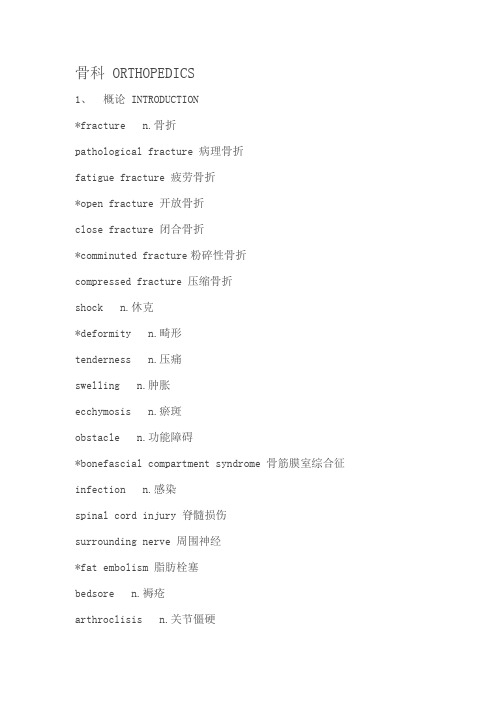
骨科 ORTHOPEDICS1、概论 INTRODUCTION*fracture n.骨折pathological fracture 病理骨折fatigue fracture 疲劳骨折*open fracture 开放骨折close fracture 闭合骨折*comminuted fracture粉碎性骨折compressed fracture 压缩骨折shock n.休克*deformity n.畸形tenderness n.压痛swelling n.肿胀ecchymosis n.瘀斑obstacle n.功能障碍*bonefascial compartment syndrome 骨筋膜室综合征infection n.感染spinal cord injury 脊髓损伤surrounding nerve 周围神经*fat embolism 脂肪栓塞bedsore n.褥疮arthroclisis n.关节僵硬ischemic necrosis 缺血性坏死ischemic contraction 缺血性挛缩*traumatic arthritis 创伤性关节炎hematoma n.血肿*callus n.骨痂heal n.愈合*synovitis n.滑膜炎*ligament n.韧带*tendon n.肌腱* pyogenic osteomyelitis 化脓性骨髓炎*reduction n.复位*bone traction 骨牵引*osteoporosis n.骨质疏松2、上肢骨折FRACTURE OF UPPER EXTREMITIES clavicle n.锁骨*humerus n.肱骨*rotation n.旋转supracondyle n.髁上blister n.水疱pulsate n.搏动thrombus n.血栓*cancellous n.松质骨*epiphysis n.骨骺*injury n.损伤*joint n.关节stability n.稳定ulna n.尺骨radius n.桡骨metacarpal bone 掌骨bone graft 植骨hemostasis 止血*periosteum n.骨膜tension n.张力adhesion n.粘连*skin grafting 植皮*arthrodesis n.关节融合extrusion n.挤压gangrene n.坏疽pallor n.苍白、灰白*amputation n.截肢plaster n.石膏paralysis n.瘫痪bandage n.绷带2、手外伤 HAND TRAUMAavulsion n.撕脱*dislocation n.脱位stiff adj.僵硬3、下肢骨折与关节损伤 FRACTURE OF LOWER EXTREMITIES AND ARTICULAR INJURYfemur n.股骨adduction n.内收separate v.分离cartilage n.软骨*synovialis n.滑膜*spinal column 脊柱5、脊柱及骨盆骨折 FRACTURE OF VERTEBRAL COLUMN AND PELVIS column n.椎体cervical column 颈椎*lumber vertebra 腰椎sacrum n.骶椎sense n.感觉movement n.运动reflect v.反射*pelvis n.骨盆6、关节脱位 ARTICULAR DISLOCATIONcongenital dislocation 先天性脱位pathological dislocation 病理性脱位*osteoarthritis n.骨关节炎*total hip replacement 全髋置换术7、运动系统慢性损伤 CHRONIC STRAIN OF MOVEMENT SYSTEM strain n.劳损*cystis n.滑囊*stenosed tenosynovitis 狭窄性腱鞘炎*ganglion n.腱鞘囊肿degenerative adj.退行性变multiply v.增生abnormal sense 感觉异常8、腰腿痛和颈肩痛LUMBAGO AND SHOULDER PAINSstenosed column 椎管狭窄9、骨与关节化脓感染OSTEOARTICULAR PURULENT LNFECTION channel n.窦道drill hole 钻孔*drainage n.引流10、骨与关节结核 OSTEOARTICULAR TUBERCULOSISbone tuberculosis 骨结核spinal cord compression 脊髓压迫11、骨肿瘤BONE TUMORbone tumor 骨肿瘤*osteochondroma n.骨软骨瘤*osteosarcoma n.骨肉瘤chemotherapy n.化疗*synoviosarcoma n.滑膜肉瘤医学英语分科常用词汇人体解剖学 HUMAN ANATOMY之运动系统 LOCOMOTOR SYSTEM 1、中轴骨 AXIAL BONES*bone n.骨*vertebrae n.椎骨*cervical vertebrae 颈椎*thoracic vertebrae 胸椎lumbar vertebrae 腰椎*sacrum n.骶骨coccyx 尾骨atlas n.寰椎axis n.枢椎*sternum n.胸骨sternal angle 胸骨角sternal manubrium 胸骨柄xiphoid process 剑突*rib n.肋*thoracic cage 胸廓2、颅SKULL*skull n.颅*frontal bone 额骨*parietal bone 顶骨*occipital bone 枕骨*temporal bone 颞骨*sphenoid bone 蝶骨*ethmoid bone 筛骨*mandible n.下颌骨hyoid bone 舌骨vomer n.犁骨*maxilla n.上颌骨palatine bone 腭骨nasal bone 鼻骨lacrimal bone 泪骨inferior nasal concha 下鼻甲zygomatic bone 颧骨*coronal suture冠状缝*sagital suture 矢状缝*lambdoid suture 人字缝orbit n.眶cranial fontanelle 颅囟2、附肢骨TARSAL BONES AND EXTREMITAL BONES *clavicle n.锁骨*scapula n.肩胛骨*humerus n.肱骨*radius n.桡骨*ulna n.尺骨carpal bone 腕骨metacarpal bone 掌骨phalanges n.指骨,趾骨*hip bone 髋骨*ilium n.髂骨*ischium n.坐骨*pubis n.耻骨*femur n.股骨patella n.髌骨*tibia n.胫骨*fibula n.腓骨tarsal bone 跗骨metatarsal bone 跖骨4、关节学 ARTHROLOGY*articulation n.关节*ligament n.韧带*flexion n.屈*extension n.伸*adduction n.收*medial rotation 旋内*lateral rotation 旋外pronation n旋前.supination n.旋后circumduction n.环转*vertebral column脊柱*thoracic cage 胸廓*intervertebral disc 椎间盘*temporal-mandibular joint 颞下颌关节*shoulder joint 肩关节*elbow joint 肘关节*radiocarpal joint 桡腕关节*pelvis n.骨盆*hip joint 髋关节*knee joint 膝关节*ankle joint 踝关节5、肌肉系统 MUSCULATURE(1)肌学系统INTRODUCTION OF MUSCULATURE *muscle n.肌肉muscle belly 肌腹tendon n.肌腱aponeurosis n.腱膜*fascia n.筋膜*tendinous sheath 腱鞘(2)躯干肌TRUNK MUSCLEStrapezius n.斜方肌latissimus dorsi 背阔肌erector spinae 竖脊肌*sternocleidomastoid adj.胸锁乳突的*scalenus n.斜角肌pectoralis major 胸大肌intercostales n.肋间肌*diaphragm n.膈(肌)*inguinal canal 腹股沟管*sheath of rectus abdominis 腹直肌鞘(3)头肌 HEAD MUSCLESorbicularis oculi 眼轮匝肌masseter n.咬肌*temporalis n.颞肌*deltoid n.三角肌*biceps brachii 肱二头肌*triceps brachii 肱三头肌*axillary fossa 腋窝(4)附肢肌 MUSCLES ATTACHED TO EXTREMITTES *gluteus maximus 臀大肌piriformis n.梨状肌*sartorius n.缝匠肌*quadriceps femoris 股四头肌triceps surae 小腿三头肌*femoral triangle 股三角popliteal fossa 腘窝医学英语分科常用词汇诊断学——骨关节系统OSTEOARTICULAR SYSTEM*Codman’striangle 骨膜三角,科德曼三角H-shaped vertebra,butterfly vertebra 蝴蝶椎Rugger-Jersay vertebra 夹心椎体Scheuermann’s disease 绍尔曼病Schmorl’s nodule 施莫尔结节Shenton’s lin e 沈通氏线apophysis n. 骺状突*arthrography n.关节造影basilar impression,basilarinvagination 颅底凹陷block vertebra 融合椎bone island 骨岛bursography n.泪囊造影compacta n.骨密度cortical porosity 皮质骨疏松症craniolacunia,luckenschadel n.颅骨陷窝*empty sella 空蝶鞍endosteal proliferation 骨内膜增生*epiphysis n.骨骺Intratrabecular resorption 骨小梁内吸收ivory vertebra 象牙椎marrow-packing disease 骨髓充填疾病massive osteolysis 大片骨溶解melopheostosis n.蜡油骨症ossification n.骨化osteopathia striata 纹骨症*osteopenia n.骨质减少osteopetrosis n.石骨症osteopoikilosis n.斑骨症pars interarticularis 椎弓峡部periosteal reaction 骨膜反应physis n.骨生长端*pseudofracture, Looser zone n.假骨折spina ventosa 骨气鼓spongiosa 骨疏松woven bone 编织骨*zone of provisional calcification 临时钙化带骨科专业英语Abduction splint 外展石膏Absorbable screws 可吸收螺钉Acetabulum 髋臼Amputation 截肢Analgesic 止痛药Ankle clonus 踝阵挛Ankylosing spondylitis 强直性脊柱炎Annulus 纤维环Arthroscopy 关节镜检查Asteofascial compartment syndrome 骨筋膜室综合症Atrophy of quadriceps femoral 股四头肌萎缩Avascular necrosis ofAvascular necrosis (A VW) 缺血性坏死Bathesthesia 深感觉Bilateral femoral head 双股骨头缺血坏死Bone traction 骨牵引Bowel and bladder dysfunction 二便障碍Brachial plexus anesthesia 臂丛麻醉Bunion 拇囊炎Capitula fibula 腓骨小头Cerclage (骨折端)环扎法Cerclage bandage 环形绷带Cerebral hemorrhage 脑出血Cerebral thrombosis 脑血栓Cervical spondylosis 颈椎病Clavicle fracture 锁骨骨折Closed suction drains 闭式引流Colle’s Fracture 科雷氏骨折Comminuted fracture of left** 左***粉碎性骨折Comminuted open fracture of talus 距骨的开放粉碎骨折Common peroneal nerve 腓总神经Congenital kyphoscoliosis 先天性侧后凸畸形congenital scoliosis 先天性脊柱侧凸Conscious mind 神志清楚Continuous epidural anesthesia (连)硬外麻Contracture of both 臀肌挛缩Core compression 髓芯减压术Crossed kirschner fixation 交叉固定DAS 动力型髋螺丝钉Debridement 清创Deformity 畸形Defuts of segmentation 分布障碍Decompression 减压Decompression of spinal canal 椎管减压Diastematomyelia 脊髓纵裂Discectomy 椎间盘摘除Discectomy of hemivertebrae 半椎体切除Dislocation 脱位DM 糖尿病Dorsal artery of foot 足背动脉Elastic fixation 弹性固定End vertebra 端椎Extension 伸External fixture 外固定Emergency case 急诊病例Faciotomy 筋膜切除术Femoral neck 股骨颈Femoral neck fracture 股骨颈骨折Figure of 8 bandage 8字绷带Flexion 屈曲Forklike deformity 餐叉样畸形Fracture 骨折Fracture of alner bone 尺骨骨折Fracture of calcaneus 跟骨骨折Fracture of distal phalange 远端趾骨骨折Fracture of distal radius 桡骨远端骨折Fracture of femoral neck 股骨颈骨折Fracture of great tubercle 肱骨大结节骨折of humurusFracture of proximal femor 股骨近端骨折Fracture of phalange 指骨骨折Fracture of radius 桡骨骨折Fracture of the base ofFracture of the scaphoid 舟状骨骨折Fracture of the ulna 尺骨骨折Fracture of ulna ocleranon 尺骨鹰嘴骨折General anesthesia 全麻General surgical 基本外科Gleniod fossa 关节盂Gluteal musclesGreater tuberosity 大结节Helo-pelvis 头颅环-骨盆环Hallux valgus 拇外翻Hallux varus 拇内翻High fever 高热Hilgenreiner’s angle 髋臼指数(acetabular index)Hemopneumothorax 血气胸Humeral head 肱骨头Humeral shaft fracture 肱骨干骨折Hypertrophy of facet 小关节增生肥大Hypoesthesia 感觉减退Ice bag 冰袋In right elbow joint 右肘肿物切除Incomplete paraplegia 不全瘫Injection 肌肉注射Interbody 椎间体Interlocking medullary mailing 带锁髓内针Intermittent claudication 间歇跛行Internal fixation 内固定术Intertrochanteric fracture 粗隆间骨折Intramscular hematoma 肌间血肿Intrumedullary needleJonalgia 膝痛Kyphoscoliosis 侧后凸Kyphosis 脊柱后凸laminectomy 椎板切除术Lateral meuleouls 外踝lipoma 脂肪瘤Local anesthesia 局麻Lodorsis 脊柱前凸Lower limb (extremuty) 下肢Mc Murrag’s test麦氏实验Medial malleouls 内踝Metacarpophalangeal joint 掌指关节Metastaluc tumor 转移癌metastatic 转移瘤Metatarsalgia 柘骨痛Metatarsal fracture 跟骨骨折Myelogram 脊髓造影Nifedipine 心痛定Nitroglyccerin 硝酸甘油Numbness 麻木Old fracture 陈旧性骨折Osteoarthritis 骨关节炎Osteochondrdoma 软骨瘤Osteomyelitis 骨髓炎Paralytic scoliosis 麻痹性脊柱侧弯Paraplegia 截瘫Patellar fracture 髌骨骨折Pathologie diagnosis 病理诊断pediculate 椎弓根PercutaneousPhlebothrombosis 下肢静脉血栓Pilon fracture 胫腓骨下端骨折Plaster slab 石膏托Poliomyelitis 脊髓灰质炎Posterior malleolus fracture 后踝骨折Posterior malleolar fracture 后踝骨折Protrusion of intervertebral 腰椎间盘突出Protrusion of intervertebral disc 腰椎间盘突出Prolapsed intervertebral disc 椎间盘脱出Pubic symphysis 耻骨支Pulmanary function 肺功能Pulpous nuclear 髓核Radial head fracture 桡骨头骨折Radius and ulna 尺、桡骨Reduction by leverage 撬拨复位Regular operation 常规手术Resection of the massSacroiliac 骶髂关节Scholiosis 脊柱侧弯Sciatica 坐骨神经痛Sciatica 坐骨神经痛Sequela of poliomyelitis 小儿麻痹(脊髓灰质炎)后遗症Sinus tract 窦道Skin traction 皮牵引Sling(Triangular bandage) 悬吊(三角巾绷带)Spatula 压舌板Spinal stenosis 椎管狭窄Spondylolisthesis 脊柱滑脱Spondylolisthesis of lumber L4-5 L4-5脊柱滑脱Spondytolysis 蛱部裂Staticfixation 静力性固定Stenosis of Spinal Canal 椎管狭窄Stenosis of the lumbar spine 腰椎管狭窄Sublimation/semiluxation 半脱位Subluxation of ankle joint 踝关节半脱位subtrochanteric fracture 粗隆下骨折supracondylar fracture 踝上骨折suture stitch 缝针synovial membrance 滑膜Syringomyelia 脊髓空洞症Taction 触觉Tension band wire 张力带钢丝Tension bond 张力带Tetraplegia / quadriplegia 四肢瘫The fifth metacarple bone 第五掌骨基底骨折Thermesthesia 温度觉Tibia-talus semidislocation 半脱位Tibial fracture 胫骨骨折Tibial plateau fracture 胫骨平台骨折Total knee arthroplasty 全膝置换Total hip arthroplasty 全髋置换Trimalleolar fracture 三踝骨折Urinary incontinence 尿失禁Valgus muscle strength 外翻肌力Veterbera fracture 椎体骨折。
骨科常用英语词汇
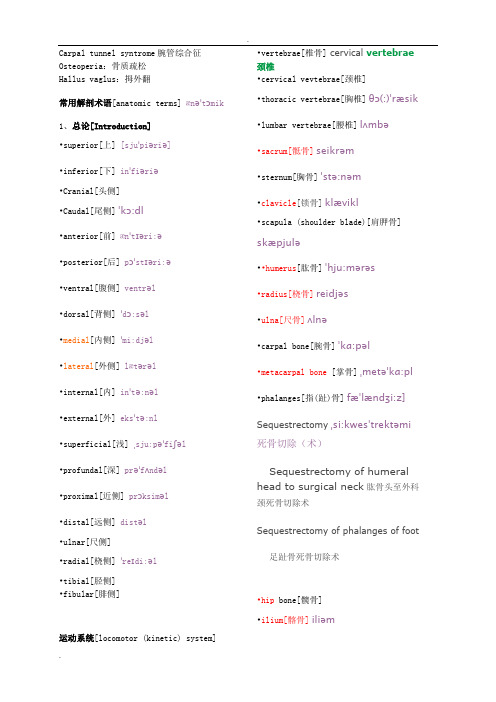
.Carpal tunnel syntrome腕管综合征Osteoperia:骨质疏松Hallus vaglus:拇外翻常用解剖术语[anatomic terms] ænəˈtɔmik 1、总论[Introduction]•superior[上] [sjuˈpiəriə]•inferior[下] inˈfiəriə•Cranial[头侧]•Caudal[尾侧]ˈkɔ:dl•anterior[前] ænˈtɪəri:ə•posterior[后] pɔˈstɪəri:ə•ventral[腹侧] ventrəl•dorsal[背侧] ˈdɔ:səl•medial[内侧] ˈmi:djəl•lateral[外侧] lætərəl•internal[内] inˈtə:nəl•external[外] eksˈtə:nl•superficial[浅] ˌsju:pəˈfiʃəl •profundal[深] prəˈfʌndəl•proximal[近侧] prɔksiməl•distal[远侧] distəl•ulnar[尺侧]•radial[桡侧] ˈreɪdi:əl•tibia l[胫侧]•fibular[腓侧]运动系统[locomotor (kinetic) system] •vertebrae[椎骨] cervical vertebrae 颈椎•cervical vevtebrae[颈椎]•thoracic vertebrae[胸椎]θɔ(:)ˈræsik •lumbar vertebrae[腰椎]lʌmbə•sacrum[骶骨]seikrəm•sternum[胸骨]ˈstə:nəm•clavicle[锁骨]klævikl•scapula (sho ulder blade)[肩胛骨]skæpjulə••humerus[肱骨]ˈhju:mərəs•radius[桡骨]reidjəs•ulna[尺骨]ʌlnə•carpal bone[腕骨]ˈkɑ:pəl •metacarpal bone [掌骨]ˌmetəˈkɑ:pl •phalanges[指(趾)骨]fæˈlændʒi:z]Sequestrectomyˌsi:kwesˈtrektəmi 死骨切除(术)Sequestrectomy of humeral head to surgical neck肱骨头至外科颈死骨切除术Sequestrectomy of phalanges of foot 足趾骨死骨切除术•hip bone[髋骨]•ilium[髂骨]iliəm.•ischium [坐骨]iskiəm•pubis[耻骨]•femur [股骨]ˈfi:mə•patella[髌骨]pəˈtelə•tibia[胫骨]ˈtɪbi:ə•fibula [腓骨]fibjulə•articulation[关节]ɑ:ˌtikjuˈleiʃən •ligament[韧带]lɪgəmənt•flexion[屈]Full extension and full flexion should be assessed actively, along with pronation and supination.应该评估主动的完全伸直和完全弯曲,以及手臂内旋和外转•extension[伸]iksˈtenʃən •adduction[收]əˈdʌkʃən•abduction[展]əbˈdʌkʃən•medial rotation[旋内]rəʊˈteɪʃənThe seasons follow each other in rotation.四季循环交替。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
• Empiric antibiotic therapy
Fixation Methods: Group 1
• Lag screw fixation • Comminution is supported by small or mini-fragment buttress plate • Bone graft is considered for comminution and required for bone loss
• Hinged joint with single axis of rotation (trochlear axis) • Trochlea is center point with a lateral and medial column
distal humeral triangle
Functional Anatomy
Mechanism of Injury
• The fracture is related to the position of elbow flexion when the load is appPhysical exam
– Soft tissue envelope – Vascular status
Surgical Anatomy
• Medial and lateral columns diverge from humeral shaft at 45 degree angle • The columns are the important structures for support of the “distal humeral triangle”
– Distal humerus • Extra-articular • Intra-articular
Note: Fixation tactics & implants are based on groups
Treatment Principles
1. Anatomic articular reduction 2. Stable internal fixation of the articular surface 3. Restoration of articular axial alignment 4. Stable internal fixation of the articular segment to the metaphysis and diaphysis 5. Early range of motion of the elbow
– Definitive fixation at repeat evaluation
• Empiric antibiotic therapy • Repeat evaluation in OR until soft tissue closure (2-5 days)
Treatment: Closed Fracture
• Median nerve - rarely injured • Ulnar nerve
Evaluation
• Radiographic exam
– Anterior-posterior and lateral radiographs – Traction views are necessary to evaluate intraarticular extension and for pre-operative planning (“ligamentotaxis”) – Traction removes overlap – CT scan helpful in selected cases
Treatment: Open Fracture
• Emergent I&D • Definitive reduction and internal fixation • Temporary external fixation across elbow if definitive fixation not possible
• The distal humerus angles forward • Lateral positioning during ORIF facilitates reconstruction of this angle
Surgical Anatomy
• The trochlear axis compared to longitudinal axis is 94-98 degrees in valgus • The trochlear axis is 3-8 degrees externally rotated • The intramedullary canal ends 2-3 cm above the olecranon fossa
• Comminuted capitellum or trochlea
OTA Classification
• Follows AO Long Bone System • Humerus, distal segment given # 13 • 3 Main Types
• Extra-articular fracture (13-A) • Partial articular fracture (13-B) • Complete articular fracture (13-C)
• “Bag of bones” technique
– Rarely indicated if at all
• Cast or cast / brace
– Indicated for completely non-displaced, stable fractures
Literature: John, et al, 1994
Summary - Classifications
• Classifications are useful for research! • Classification data may not be reproducible between different surgeons! • Classification data may not be reproduced by the same surgeon at different times!
Literature: Cobb & Morrey, 1997
• 20 patients – (avg age 72 yrs) • TEA for distal humeral fracture • Conclusion
Summary - Classifications
• Meaningful patterns
– Extra-articular distal humerus
• Medial epicondyle • Lateral epicondyle • Distal metaphyseal humerus
– Partial articular distal humerus
• Capitellum • Trochlea
– Complete articular distal humerus
Simplicity
• Group 1
– – – – Lateral epicondyle Medial epicondyle Capitellum Trochlea
• Group 2
Other Potential Options
• Total elbow arthroplasty
– Comminuted intra-articular fracture in the elderly – Promotes immediate ROM – Usually limited by poor remaining bone stock
100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Result very good good fair/poor
Literature: Pereles, et al, 1997
• 18 patients (> 60 yrs, avg age: 71 yrs) • SF-36 evaluation • All patients had a good or excellent clinical result • Their general health was comparable to published norms
• Radial and ulnar pulses
– Neurologic status
• Radial nerve - most commonly injured
– 14 cm proximal to the lateral epicondyle – 20 cm proximal to the medial epicondyle
• Definitive reduction and internal fixation
– Timing
• Within 24 hours or at 5-7 days – The inflammatory response peaks at 3 days post injury. ORIF during that peak may lead to excessive heterotopic ossification
• Each broad category further subdivided into 9 specific fracture types
OTA Classification
• Humerus, distal segment (13) – Types • Extra-articular fracture (13-A) • Partial articular fracture (13-B) • Complete articular fracture (13-C)
